Abstract
A literature review on new-onset autoimmune connective tissue diseases (ACTDs) following COVID-19 is lacking. We evaluated potential associations between COVID-19 and the development of new-onset ACTDs. The “population” was adults with disease terms for ACTDs, including systemic lupus erythematosus (SLE), Sjogren’s syndrome, systemic sclerosis (SSc), idiopathic inflammatory myositis (IIM), anti-synthetase syndrome, mixed CTD and undifferentiated CTD, and “intervention” as COVID-19 and related terms. Databases were searched for English-language articles published until September 2022. We identified 2236 articles with 28 ultimately included. Of the 28 included patients, 64.3% were female, with a mean age was 51.1 years. The USA reported the most cases (9/28). ACTD diagnoses comprised: 11 (39.3%) IIM (including four dermatomyositis); 7 (25%) SLE; four (14.3%) anti-synthetase syndrome; four (14.3%) SSc; two (7.1%) other ACTD (one lupus/MCTD overlap). Of eight, four (14.3%) patients (including that with lupus/MCTD) had lupus nephritis. The average time from COVID-19 to ACTD diagnosis was 23.7 days. A third of patients were admitted to critical care, one for treatment of haemophagocytic lymphohistiocytosis in SLE (14 sessions of plasmapheresis, rituximab and intravenous corticosteroids) and nine due to COVID-19. 80% of patients went into remission of ACTD following treatment, while three (10%) patients died—one due to macrophage activation syndrome with anti-synthetase syndrome and two from unreported causes. Our results suggest a potential association between COVID-19 and new-onset ACTDs, notably in young females, reflecting more comprehensive CTD epidemiology. The most common diagnosis in our cohort was IIM. The aetiology and mechanisms by which ACTDs emerge following COVID-19 remain unknown and require further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic resulted in substantial mortality and morbidity [1]. Globally, an estimated 6.49 million people have died due to COVID-19 and its complications [2]. Although primarily a respiratory disease, SARS-CoV-2 infection has been linked to hyperinflammation in multiple organs due to cytokine storm and molecular mimicry [3, 4]. Several new autoimmune and autoinflammatory conditions have been reported among the SARS-CoV-2 survivors [5,6,7]. A systematic review (SR) by Saad et al. discovered that SARS-CoV-2 infection is associated with neurological, cardiological, and musculoskeletal inflammatory diseases [8].
Similarly, recent studies have linked SARS-CoV-2 infection to the onset of systemic autoimmune rheumatic diseases (SARD) following SARS-CoV-2 infection [9, 10]. An SR by Chaudhry et al. elucidated that eight patients developed new rheumatoid arthritis (RA) and several others had flare-ups of their existing RA after being infected with SARS-CoV-2 [11], aligning with another SR of literature on the vasculitides after COVID-19 infection [12]. Despite the emergence of new-onset autoimmune connective tissue diseases (ACTDs) following COVID-19 infection, an SR of the literature is lacking. Our objectives were twofold: (i) to investigate the prevalence, clinical outcomes, treatment, and prognosis of new-onset ACTDs after SARS-CoV-2 infection and (ii) to evaluate the potential association between COVID-19 infection and the development of new-onset ACTDs in adults.
Methods
This SR was conducted in accordance with the Cochrane Handbook and reported as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [13, 14].
The protocol was developed and registered in the PROSPERO database of SRs (CRD42022358750). The review question was: Is there an association between COVID-19 infection and the development of new-onset ACTDs in adults? We assessed the incidence of new cases of ACTDs developing after COVID-19 infection and their clinical characteristics, treatment, and outcomes.
Population
We included adults with ACTDs, including (but not limited to) systemic lupus erythematosus (SLE), Sjogren’s syndrome, systemic sclerosis (SSc), any idiopathic inflammatory myositis (IIM), anti-synthetase syndrome, mixed CTD and undifferentiated CTD (and related database specific indexing terms), with “intervention” as COVID-19 and related terms. All indexing terms and related keywords used are detailed within the supplementary materials.
We excluded patients developing new-onset ACTDs without prior SARS CoV-2 infection or patients without developing new-onset ACTD or flare of existing ACTDs.
Patients developing a systemic autoimmune rheumatic disease, not included in the above list, were excluded (such as inflammatory arthropathies and vasculitides).
Outcome
Outcomes were demographics, clinical characteristics and disease trajectory, treatment, and timing of developing new-onset ACTDs after SARS-CoV-2.
Intervention and comparator descriptors were not applied to this review.
Search strategy, databases and study selection
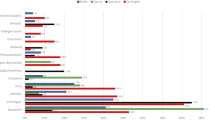
The search strategy is strategies are available in the online supplementary material. To ensure full comprehensive coverage, indexing terms (MeSH, applicable to Medline and Cochrane, and Emtree headings used on Embase) along with relevant keyword searching were incorporated. For terms for COVID-19, a dedicated search strategy developed by the National Institute for Clinical Excellence was used (Fig. 1). Medline, Embase, and Cochrane databases were searched from 2019 till September 2022, restricted to English-language articles only concerning adult populations. Eligible articles were: case reports and series (of any sample size), observational studies, qualitative studies and randomised controlled trials. Patients developing ACTDs without prior COVID-19 or reporting flares of existing ACTDs were excluded. Information was extracted on patient demographics, new ACTDs’ onset time, clinical characteristics, COVID-19 and ACTD treatment, and COVID-19 and ACTD outcomes.
Full-length articles were uploaded into EndNote V.X9 (Clarivate Analytics, Pennsylvania, USA), with duplicates removed (Fig. 2). Titles and abstracts were screened for eligibility, and articles meeting inclusion criteria were examined in further detail. For validation, 20% of the articles were screened. There were nil disagreements.
All retrieved articles were either case reports or case series; therefore, no formal risk of bias assessment was possible.
Results
After deduplication, 2336 articles were identified. After screening the title and abstract, 2293 papers were excluded, with 43 proceeding to full-text screening. Ultimately, 28 articles (all single case reports) were included.
Article information and basic demographics are detailed in Table 1. Of the 28 included patients, 64.3% were female. The mean age was 51.1 years (range 20–89 years). Most case reports were from the USA (9/28), followed by Iran (4/28).
ACTD diagnoses comprised: 11 (39.3%) IIM (including 4 cases of dermatomyositis); 7 (25%) SLE; 4 (14.3%) anti-synthetase syndrome; 4 (14.3%) SSc; 2 (7.1%) other ACTD (one diagnosed with lupus/MCTD overlap). Of the eight patients diagnosed with SLE or lupus/MCTD, four (14.3%) were diagnosed with lupus nephritis. The average onset time from COVID-19 infection to ACTD diagnosis was 23.7 days.
The majority of cases (n = 16) were reported in 2022 and only one case of lupus nephritis was reported in 2020.
Investigations carried out varied markedly depending on geographic region (Table 2). Serum inflammatory markers (ESR and CRP) were gathered before the diagnosis of CTD in (9 ESR) and (14 CRP) cases with a mean of 70.2 mm/hr and 74.3 mg/L, respectively. One case had a normal ESR prior to diagnosis of ACTD and two patients had CRP levels reported within the normal range prior to ACTD diagnosis. Post-diagnosis of ACTD, there was reduction in both the ESR and CRP levels of those reported initially, with a mean of 53 mm/hr and 12.2 mg/L, respectively. One case had ESR within the normal range, and one had CRP within the normal range post-CTD diagnosis.
Regarding autoantibody levels (Table 2), anti-nuclear antibody (ANA) was the most commonly positive autoantibody in this cohort (n = 16), with a speckled pattern most commonly described. Where ANA was reported, two cases reported normal ANA titres and normal levels for the remaining autoantibody panel (including myositis-specific antigens). Details regarding all other autoantibodies are available in Table 2.
The most common imaging modality reported for our patients was computed tomography (CT) of the chest (n = 17) with the most common finding being “changes suggestive of interstitial lung disease (n = 13). Four cases did not find any pulmonary changes, out of which three cases had magnetic resonance (MRI) evidence suggestive of inflammatory myositis. Seven cases had MRI imaging of the muscles, which demonstrated muscle oedema suggestive of inflammatory myositis; one had electromyography to confirm the diagnosis.
The most commonly diagnosed CTD in our review was IIM, with 11 cases identified, four dermatomyositis. There was a wide age range (20–89 years), with female predominance (n = 9). CTD symptoms onset time also varied markedly, ranging from 14 to 112 days since COVID-19 diagnosis. Autoantibody serology also varied, with just three cases reporting positive ANA [19,20,21] and six reporting positivity for other autoantibodies, including NXP2, Mi2, Ku, and Ro [19,20,21,22,23,24]. In three cases with negative autoantibody serology, a diagnosis of myositis was made based on MRI muscle imaging, skin biopsy histology (consistent with dermatomyositis) and electromyography findings [23, 25,26,27]. Three cases did not report serology or imaging justification of diagnosis, with these diagnoses based on classic symptoms including “malaise, muscle weakness and skin lesions” and “severe intractable pain in bilateral lower extremities and subjective pelvic girdle weaknesses’’ associated with a high creatinine phosphokinase level [25, 28, 29].
COVID-19 treatment differed depending on the stage of pandemic and the country. Ten patients were admitted to critical care, one for ACTD treatment for SLE with haemophagocytic lymphohistiocytosis (HLH; 14 sessions of plasmapheresis, rituximab and intravenous corticosteroids) and nine for COVID-19. Five cases made explicit comments about the severity of COVID-19. However, no articles specified which grading system was used. There are several COVID-19 severity indices available, e.g. National Institute for Health, World Health Organisation, but none were mentioned in the texts. Nonetheless, three were classified as “mild”, one as “low severity” and one as “severe”.
Seventeen case reports provided details of treatment for COVID-19 (either the details of therapies given, or the fact that none were administered; Table 3). The following specific treatments were described for these patients: one case received a combination of tocilizumab, anticoagulation, hydroxychloroquine, and azithromycin; one received tapering corticosteroids and nintedanib for post-COVID-19 lung fibrosis; one received supplemental oxygen, dexamethasone, ipratropium bromide and enoxaparin; one received azithromycin, hydroxychloroquine; one received naproxen and Diphenhydramine syrup; one received hydroxychloroquine, cefazolin and azithromycin; one received “broad-spectrum antibiotics”, convalescent plasma and dexamethasone; one received remdesivir, corticosteroids, colchicine and plasmapheresis; one received levofloxacin and dexamethasone; one received oxygen, lopinavir/ritonavir, hydroxychloroquine, doxycycline, ceftriaxone and anticoagulant. Two cases of COVID-19 infection received no treatment.
Regarding CTD treatment, of those described (27), different strengths of corticosteroids (methylprednisolone in 8 and oral prednisone in 15) were the most frequently prescribed (Table 3). This was followed by hydroxychloroquine (n = 9), mycophenolate mofetil (MMF) (n = 8), rituximab (n = 4), intravenous immunoglobulins (n = 3), azathioprine (n = 3), methotrexate (n = 2), cyclophosphamide (n = 2), plasmapheresis (n = 1), ciclosporin (n = 1), tofacitinib (n = 1), nifedipine (n = 1), tacrolimus (n = 1) and colchicine (n = 1). Antibiotic prophylaxis was administered in two cases, and vitamins B and D each in one case. The majority (80%) of patients experienced remission of ACTD following treatment. In comparison, three (10%) patients died—one from macrophage activation syndrome associated with anti-synthetase syndrome and two from unknown causes.
Discussion
This SR summarised the data on new-onset ACTDs following infection with SARS-CoV-2. Our findings from the 28 included cases suggest a potential association between COVID-19 infection and new-onset ACTDs, particularly in young females, reflective of wider CTD epidemiology. To our knowledge, this is the first SR to examine the association between COVID-19 and new-onset ACTDs, including the temporal relationship, diagnostic parameters and treatment.
Since March 2020, as the COVID-19 pandemic has progressed, so has our understanding of clinical sequelae arising following the infection. During the early stages of the pandemic, it was recognised that SARS-CoV-2 infection could cause a flare in SARD, including CTDs, which was well reported in the literature [15, 16]. ANA positivity was noted in 25% of hospitalised patients with acute COVID-19 infection, with a proportion of patients presenting with rheumatic manifestations, such as muscle weakness for myositis and rash and arthralgia for SLE, as in some of the cases described herein [16, 17]. An association was observed between severe COVID-19 and multisystem inflammatory syndromes and “cytokine storm”, similar to HLH and macrophage activation syndrome previously associated with ACTDs [17, 18]. Likewise, a temporal association between acute COVID-19 infection and the onset of ACTD became apparent in increasing number of cases.
The most common CTD following COVID-19 infection identified in our cohort was IIM, with four cases of dermatomyositis. Interestingly, IIM was diagnosed with negative autoantibody serology and solely on imaging or histology finding. In some cases, no investigative finding was reported, and a diagnosis was made based on symptoms [25, 28, 29]. It remains to be seen whether a subset of IIM is required within the nomenclature to account for such diagnoses arising post-COVID-19 infections, especially in the absence of typical serology.
Seven patients included in our review were diagnosed with SLE, and one with lupus/mixed connective tissue disease (MCTD) overlap [30,31,32,33,34,35,36,37]. Of these eight patients, four presented with lupus nephritis [30, 31, 33, 34]. Again, a wide age range was noted (22–85 years) with, 75% (6/8) of cases being female. One patient with SLE and antiphospholipid syndrome died following admission to the intensive therapy unit (ITU), although it was not specified which treatment she received for either COVID-19 or SLE [35]. Most patients required high-dose intravenous corticosteroids, followed by DMARDs, such as mycophenolate mofetil or hydroxychloroquine. One patient received plasmapheresis and rituximab after requiring ITU admission to treat ACTD and associated HLH [36]. In addition, Nunes et al. reported a case of toxic epidermal necrolysis-like lupus presentation following SARS-Cov-2 infection in a 70-year-old female with hypertension, who went into CTD remission following treatment with hydroxychloroquine and corticosteroids [38].
Our findings were consistent with those of Chaudry et al. [11], who conducted a similar literature review and discovered limited evidence of inflammatory arthritis developed following COVID-19 infection. However, this could be explained by the possible heterogeneity of the cases. On the other hand, an SR of case reports and case series by Wong et al. [12] found an association between COVID-19 and vasculitis. Moreover, COVID-19 has been linked to cytokine storm leading to an immune response to small vessel damage causing vasculitis and other immune-mediated inflammatory diseases [48]. Therefore, more research is needed to investigate the association between ACTDs and COVID-19.
The aetiology and mechanisms by which ACTDs emerge following COVID-19 infection remain unknown and require more robust epidemiological data. It is possible that patients had a mild asymptomatic disease in a genetically predisposed individual prior to COVID-19 infection, with SARS-CoV-2 triggering a flare due to the hyperinflammatory state [3]. Machado et al. recently proposed a new entity of “COVID-19-associated arthritis” in a similar review of inflammatory arthritis following COVID-19 infection. It may be that such nomenclature is required for those developing ACTD following SARS-COv-2 infection [39]. Further studies to elucidate the pathogenesis and aetiology of new-onset ACTD in these cases will aid the characterisation and understanding of these diseases.
Strengths and limitations
Our SR included a small number of cases due to the specific area of rheumatology it covered and the rarity of the ACTD subset we investigated. This might have resulted in biased results, and it is important not to infer causality solely from these cases. However, it is an important subset of ACTDs following SARS-CoV-2 infection, which are relatively unexplored. Our findings will pave the way for future research and better care for ACTD patients. This SR only included case reports that were limited in establishing a cause–effect relationship and, thus, were not generalisable. Therefore, extensive and longitudinal studies to determine causation are recommended to supplement the current literature.
In conclusion, we summarised 28 cases of new-onset ACTD in this SR, the most common presentations being IIM and SLE. However, cases of SSc and rarer diseases such as anti-synthetase syndrome were also identified. Further epidemiological studies of ACTD diagnosed post-COVID-19 infection will help us better understand this association and help identify those at risk of developing ACTD after contracting SARS-CoV-2 infection.
Data availability
Data available upon request.
References
Matta S, Chopra KK, Arora VK (2020) Morbidity and mortality trends of Covid 19 in top 10 countries. Indian J Tuberc 67(4S):S167–S172
WHO Coronavirus (COVID-19) dashboard | WHO Coronavirus (COVID-19) dashboard with vaccination data. https://covid19.who.int/?mapFilter=deaths.
Caso F, Costa L, Ruscitti P, Navarini L, Del Puente A, Giacomelli R et al (2020) Could Sars-coronavirus-2 trigger autoimmune and/or autoinflammatory mechanisms in genetically predisposed subjects? Autoimmun Rev 19(5):102524
Liu Y, Sawalha AH, Lu Q (2021) COVID-19 and autoimmune diseases. Curr Opin Rheumatol 33(2):155–162
Yazdanpanah N, Rezaei N (2022) Autoimmune complications of COVID-19. J Med Virol 94(1):54–62
Dotan A, Muller S, Kanduc D, David P, Halpert G, Shoenfeld Y (2021) The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmun Rev 20(4):102792
Galeotti C, Bayry J (2020) Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol 16(8):413–414
Saad MA, Alfishawy M, Nassar M, Mohamed M, Esene IN, Elbendary A (2021) COVID-19 and autoimmune diseases: a systematic review of reported cases. Curr Rheumatol Rev 17(2):193–204
Tang KT, Hsu BC, Chen DY (2021) Autoimmune and rheumatic manifestations associated with COVID-19 in adults: an updated systematic review. Front Immunol 12:645013
Nune A, Iyengar KP, Mulherin D, Ish P, Musat CA, Sapkota HR (2022) Granulomatosis with polyangiitis and COVID-19 pneumonia. Indian J Rheumatol 17(2):210–212
Chaudhry ZS, Nellessen N, Reis C, Sharip A (2022) The development of inflammatory arthritis following SARS-CoV-2 infection: a systematic review of the literature. Fam Pract. https://doi.org/10.1093/fampra/cmac029
Wong K, Farooq Alam Shah MU, Khurshid M, Ullah I, Tahir MJ, Yousaf Z (2022) COVID-19 associated vasculitis: a systematic review of case reports and case series. Ann Med Surg 74:103249
Cochrane Handbook for Systematic Reviews of Interventions | Cochrane Training. https://training.cochrane.org/handbook/current.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Di Iorio M, Cook CE, Vanni KMM, Patel NJ, D’Silva KM, Fu X et al (2022) DMARD disruption, rheumatic disease flare, and prolonged COVID-19 symptom duration after acute COVID-19 among patients with rheumatic disease: a prospective study. Semin Arthritis Rheum 55:152025
Ahmed S, Zimba O, Gasparyan AY (2021) COVID-19 and the clinical course of rheumatic manifestations. Clin Rheumatol 40(7):2611–2619
Lerma LA, Chaudhary A, Bryan A, Morishima C, Wener MH, Fink SL (2020) Prevalence of autoantibody responses in acute coronavirus disease 2019 (COVID-19). J Transl Autoimmun 3:100073
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ et al (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395:1033–1034
Holzer MT, Krusche M, Ruffer N, Haberstock H, Stephan M, Huber TB et al (2022) New-onset dermatomyositis following SARS-CoV-2 infection and vaccination: a case-based review. Rheumatol Int 42(12):2267
Borges NH, Godoy TM, Kahlow BS (2021) Onset of dermatomyositis in close association with COVID-19-a first case reported. Rheumatology (Oxford) 60(SI):SI96
Sacchi MC, Tamiazzo S, Lauritano EC, Bonometti R (2020) Case report of COVID-19 in an elderly patient: could SARS-CoV2 trigger myositis? Eur Rev Med Pharmacol Sci 24(22):11960–11963
Zhang H, Charmchi Z, Seidman R, Anziska Y, Velayudhan V, Perk J (2022) COVID-19 associated myositis with severe proximal and bulbar weakness (P9-9.006). Neurology 98(18 Supplement)
Okayasu T, Ohta R, Igarashi M, Kurita Y, Hayakawa M, Sano C (2022) Coexistence of pancytopenia and myositis after developing COVID-19. Cureus. https://doi.org/10.7759/cureus.26978
Okada Y, Izumi R, Hosaka T, Watanabe S, Shijo T, Hatchome N et al (2022) Anti-NXP2 antibody-positive dermatomyositis developed after COVID-19 manifesting as type I interferonopathy. Rheumatology (Oxford) 61(4):E90–E92
Shahidi Dadras M, Rakhshan A, Ahmadzadeh A, Hosseini SA, Diab R, Safari Giv T et al (2021) Dermatomyositis-lupus overlap syndrome complicated with cardiomyopathy after SARS-CoV-2 infection: a new potential trigger for musculoskeletal autoimmune disease development. Clin Case Rep 9(10):e04931
Assar S, Pournazari M, Soufivand P, Mohamadzadeh D (2022) Successful treatment of COVID-19 induced neutrophilic myositis with intravenous immunoglobulin and corticosteroids: a case report. Reumatismo 73(4):232–235
Amin S, Rahim F, Noor M, Bangash A, Ghani F (2022) Polymyositis: the comet tail after COVID-19. Cureus 14(6):e26453
Aldaghlawi F, Shammah A, Kio E (2021) SARS-CoV-2 infection complicated with cold agglutinin disease and myositis. Clin Case Rep 9(4):2196–2199
Lokineni S, Mortezavi M (2021) Delayed-onset necrotizing myositis following COVID-19 infection. Eur J Case Rep Intern Med 8(4):002461
Ramachandran L, Dontaraju VS, Troyer J, Sahota J (2022) New onset systemic lupus erythematosus after COVID-19 infection: a case report. AME Case Rep 6:14
Kazzi B, Fine D, Geetha D, Chung M, Monroy-Trujillo M, Timlin H (2022) New-onset lupus nephritis associated with COVID-19 infection. Lupus 31(8):1007–1011
Assar S, Pournazari M, Soufivand P, Mohamadzadeh D (2022) Systemic lupus erythematosus after coronavirus disease-2019 (COVID-19) infection: case-based review. Egypt Rheumatol 44(2):145–149
Ali S, Almas T, Zaidi U, Ahmed F, Shaikh S, Shaikh F et al (2022) A novel case of lupus nephritis and mixed connective tissue disorder in a COVID-19 patient. Ann Med Surg 78:103653
Zamani B, Moeini Taba SM, Shayestehpour M (2021) Systemic lupus erythematosus manifestation following COVID-19: a case report. J Med Case Rep 15(1):1–4
Slimani Y, Abbassi R, El Fatoiki FZ, Barrou L, Chiheb S (2021) Systemic lupus erythematosus and varicella-like rash following COVID-19 in a previously healthy patient. J Med Virol 93(2):1184–1187
Ali R, Mehannek R, Patel A, Paige A, Reddy S, Guma M et al (2021) Systemic lupus erythematosus with hemophagocytic lymphohistiocytosis: is COVID-19 the inciting factor? Cureus 13(11):e19657
Bonometti R, Sacchi MC, Stobbione P, Lauritano EC, Tamiazzo S, Marchegiani A et al (2020) The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection. Eur Rev Med Pharmacol Sci 24(18):9695–9697
Nunes AL, Simoes L, Figueiredo C, Carvalho R, Lima J, Santos RM (2022) Toxic epidermal necrolysis-like lupus erythematous presentation following SARS-CoV-2 infection. J Med Cases 13(2):89–93
Farisogullari B, Pinto AS, Machado PM (2022) COVID-19-associated arthritis: an emerging new entity? RMD Open 8(2):e002026
Pereira M, Shivdasani D, Roy D, Rungta R, Dang S, Singh N (2022) Post-COVID-19 unusual inflammatory syndromes detected on 18F-FDG PET/CT scan. Clin Nucl Med 47(4):E363–E365
Giuggioli D, Spinella A, de Pinto M, Mascia MT, Salvarani C (2022) From Raynaud phenomenon to systemic sclerosis in COVID-19: a case report. Adv Skin Wound Care 35(2):123–124
Chandra A, Kahaleh B (2022) Systemic sclerosis (SSc) after COVID-19: a case report. Cureus 14(3):e23179
Bouchard Marmen M, Ellezam B, Fritzler MJ, Troyanov Y, Gould PV, Satoh M et al (2022) Anti-synthetase syndrome occurring after SARS-CoV-2 infection. Scand J Rheumatol 51(3):255–257
Blum FR, Sampath AJ, Gilbert AL, Foulke GT (2022) Diffuse systemic sclerosis following COVID-19 infection. Scand J Rheumatol. https://doi.org/10.1080/03009742.2022.2103935
Anderle K, Machold K, Kiener HP, Bormann D, Hoetzenecker K, Geleff S et al (2022) COVID-19 as a putative trigger of anti-MDA5-associated dermatomyositis with acute respiratory distress syndrome (ARDS) requiring lung transplantation, a case report. BMC Rheumatol. https://doi.org/10.1186/s41927-022-00271-1
Keshtkarjahromi M, Chhetri S, Balagani A et al (2021) Macrophage activation syndrome in MDA5 antibody-positive dermatomyositis and COVID-19 infection. BMC Rheumatol 5(1):59
Fineschi S (2021) Case report: systemic sclerosis after Covid-19 infection. Front Immunol 12:2439
Galeotti C, Bayry J (2020) Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol 16:413–414. https://doi.org/10.1038/s41584-020-0448-7
Funding
Nil funding to declare.
Author information
Authors and Affiliations
Contributions
Conceptualization: KK, MD, AN; Methodology: KK, MD, HE, AN, Formal analysis and investigation: KK, MD; Writing—original draft preparation: KK, MD; Writing—review and editing: KK, MD, HE, AN; Supervision: AN. All co-authors take full responsibility for the integrity and accuracy of all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors (KK, MD, HE, AN) declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kouranloo, K., Dey, M., Elwell, H. et al. A systematic review of the incidence, management and prognosis of new-onset autoimmune connective tissue diseases after COVID-19. Rheumatol Int 43, 1221–1243 (2023). https://doi.org/10.1007/s00296-023-05283-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05283-9