Abstract
The aim of this study was to identify the role of nasal Staphylococcus aureus (S. aureus) colonization and the effect of systemic or local antibiotic treatment on disease activity in patients with antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis and ear nose and throat (ENT) involvement. Clinical, laboratory and histological data from all patients with ANCA-associated vasculitis and ENT involvement, who were diagnosed in two medical centres in The Netherlands between 1981 and 2020, were retrospectively collected. Nasal S. aureus colonization was defined as at least one positive nasal swab during follow-up. Data on systemic (cotrimoxazole and azithromycin) and local (mupirocin) antibiotic use were collected. Disease activity was divided into systemic and local disease activity. Univariate analyses and regression analyses (negative binomial Poisson and binary regression) were used. Two-hundred and thirteen patients were available for analysis. Median follow-up time was 8 (IQR 3–17) years. S. aureus colonization was tested in 100 (46.9%) cases of whom 44 patients (44%) tested positive. In these 100 patients, systemic and local disease activity at baseline and at last visit were comparable between patients with and without S. aureus colonization. Twenty-eight of the 44 S. aureus positive patients received antibiotics aimed at eradication of S. aureus. No statistically significant difference was found between the treated versus non-treated group with regard to systemic and local disease activity. Nasal S. aureus colonization does not influence systemic or local disease activity. Antibiotic treatment aimed at eradication did not modify disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) is a necrotizing vasculitis, predominantly affecting small or medium vessels with few or no immune deposits [1]. Presence of autoantibodies directed against neutrophil cytoplasmic constituents, predominantly proteinase 3 (PR3) and myeloperoxidase (MPO), is a hallmark of AAV [2].
AAV is subdivided into three subtypes; microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) and eosinophilic granulomatosis with polyangiitis (EGPA) [3].
The clinical characteristics can vary among these three subtypes. Both GPA and EGPA are characterized by necrotizing granulomatous inflammation often involving the respiratory tract. Ear nose and throat (ENT) involvement is most common in GPA [4, 5].
AAV has a relapsing—remitting disease course. Several risk factors for relapses have been reported, including bacterial infections especially nasal Staphylococcus aureus (S. aureus) infections in GPA [6,7,8,9,10,11,12] Some studies have shown a higher rate of chronic nasal colonization with S. aureus in GPA patients compared to healthy individuals [7, 10, 13, 14]. In contrast to the general population of which one-third has intermittent and one-third has chronic colonization of S.aureus, in GPA patients 60–70% is carrier [15]. Nasal S.aureus carriage is a global phenomenon. In The Netherlands an estimated 35% of the healthy population is colonized with S.aureus [16]. In some studies, nasal S.aureus colonization in AAV was associated with relapse of disease activity. This finding led to the use of antibiotics in AAV [17, 18].
However, the effect of antibiotics on disease activity in AAV patients with S. aureus colonization is controversial. Some studies showed earlier time to remission [17, 19] or prevention of relapses [9, 17, 20] in GPA patients when treated with cotrimoxazole. Other studies found no beneficial effect of cotrimoxazole on disease activity in GPA patients colonized with S. aureus [10, 13, 21]. Efficacy of other antibiotics than cotrimoxazole on disease activity, and the effect of antibiotics in S. aureus colonized EGPA and MPA patients are not known [17]. Therefore, the aim of this study is to determine the effect of nasal S. aureus colonization and treatment with local or systemic antibiotics on disease activity in AAV patients with ENT involvement.
Methods
Case definition
In this retrospective cohort study, we analysed the presence of nasal S.aureus colonization in patients with ANCA-associated vasculitis and ENT involvement. In case of S.aureus colonization, we analysed the effect of antibiotic treatment on disease activity.
Disease activity was divided into systemic and local disease activity. Systemic disease outcomes included history of one or more relapses, relapse number per patient year and BVAS3 score at last visit. Local disease outcomes included the development of saddle nose deformity or subglottic stenosis during follow-up and history of one or more ENT relapses.
Data collection and participants
Data from patients with AAV from the University Medical Centre Utrecht and Meander Medisch Centrum Amersfoort diagnosed between 1981 and 2020 were collected. Both centres are vasculitis referral centres. Patients were identified using related International Classification of Diseases (ICD) codes. AAV was defined by the Chapel Hill consensus criteria [3]. ENT involvement was defined as presence of at least one of the ENT symptoms stated in Birmingham vasculitis activity score (BVAS) version 3 (BVAS3) [22]. Saddle nose deformity or subglottic stenosis were defined as irreversible damage.
Clinical, laboratory and histopathology data were prospectively collected (during routine care patients visits) and retrospectively extracted from the electronic patient records. Two medical experts were consulted in case medical data appeared indistinct.
Clinical data included gender, disease duration, age at disease onset and last visit, ethnicity, comorbidities according to the Charlson comorbidity index [23], AAV type, ANCA status, organ involvement, disease activity defined by the BVAS3 at diagnosis and at last visit, number and characteristics of relapses [22]. Relapse was defined as a rise in BVAS3 score of at least one point, new or progression of existing symptoms or the need for treatment intensification [22]. No difference was made between major and minor relapse. The follow-up period was defined as the period between diagnosis and last clinic visit or death. Treatment related data that were collected included details concerning induction and maintenance therapy, dose, duration and administration route, maximum dosage of steroids and cumulative dose of cyclophosphamide.
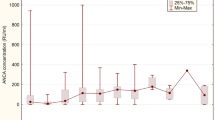
Laboratory results were collected at diagnosis and at last visit within a time frame of 3 months at diagnosis and within a time frame of 6 months at last visit. These included ANCA-titre, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), leukocyte count, estimated glomerular filtration rate (eGFR), serum creatinine and the presence of protein in urine (proteinuria).
Histopathology data included results from tissue biopsies performed on ENT, kidney, lung, skin and/or other tissue. Results were divided into supportive, inconclusive or non-supportive for the diagnosis of AAV as concluded by the pathologist.
Data on ENT involvement included ENT symptoms according to BVAS3 score (either reported in patient records or calculated based on reported symptoms) at diagnosis and during follow-up and presence of irreversible damage (saddle nose deformity and subglottic stenosis). ENT limited AAV was defined as the presence of vasculitis activity in the nose without further systemic disease activity. Additionally, information with regard to S. aureus colonization and treatment with systemic antibiotics (cotrimoxazole and azithromycin), local antibiotics (mupirocin), and nasal steroids or nasal lavage with saline solution (NaCl 0.9%) was collected. Colonization was defined as at least one positive nasal swab during follow-up.
Inclusion and exclusion criteria
Inclusion criteria were patients aged 18 years and older, with AAV defined by the Chapel Hill consensus criteria and ENT involvement according to BVAS3 score and a performed S.aureus colonization test. Exclusion criteria were patients without available data on ENT involvement or colonization.
Statistical analysis
Descriptive tests were used for baseline characteristics of the study population. Categorical data were presented in numbers and percentages, continuous variables were described as median with interquartile ranges (IQR).
First, univariate analyses were used to analyse the influence of S. aureus on disease activity.
Presence of relapse was analysed by Pearson chi-square test and relapse number per patient year and BVAS3 score at last visit were analysed using Mann–Whitney U test.
Local disease activity, consisting of presence of ENT relapse, development of saddle nose deformity or subglottic stenosis during follow-up were analysed by Pearson Chi-Square tests.
Second, to correct for confounders gender, age at onset, AAV type, follow-up time and use of nasal steroids, regression analyses were performed to analyse the effect of S. aureus colonization on disease activity. The number of patients with subglottic stenosis at last visit was too small for regression analysis.
The number of relapses per patient year were analysed using a negative binomial Poisson regression because of non-normal distribution of data to calculate incidence rate-ratios of relapses during follow-up. Binary regression analyses were used to analyse the effect of S. aureus colonization on the presence of one or more ENT relapses during follow-up and the development of saddle nose deformity during follow-up presented as odds ratio (OR) with 95% confidence interval (CI).
To analyse the effect of S. aureus eradication, the same univariate analyses and systemic and local outcome measurements were used as mentioned above. Patient numbers were too small to perform regression analysis on the effect of antibiotic treatment on systemic and local disease activity.
P values ≤ 0.05 were considered statistically relevant. IBM SPSS Statistics version 25.0.0.2 was used.
Results
Baseline patient characteristics
A total of 213 AAV patients with ENT involvement were included. Baseline characteristics and treatment details of all included patients and patients with a performed test for S. aureus colonization are mentioned in Table 1. Median follow-up time was 8 (IQR 3–17) years. Use of nasal steroids during follow-up were prescribed to 37.6% of the patients.
S. aureus colonization was evaluated in 100 (46.9%) cases, of which 44 (44%) tested positive. Within the group of tested patients, antibiotics were prescribed to 40 (40%) patients regardless the presence of S. aureus colonization. A flow-chart is shown in Fig. 1. Cotrimoxazole was administered in 32 patients, azithromycin in two patients and 28 patients received nasal mupirocin ointment. In the patients who tested positive, 28 (28%) patients received antibiotic treatment. Dosages and duration of antibiotics varied amongst patients.
Relapse number per patient year was 0.1 (IQR 0–0.2) and the median BVAS3 score at last visit was 0 (IQR 0–4). Only one patient developed subglottic stenosis and 13 patients developed a saddle nose deformity during follow-up.
Nasal S. aureus colonization and disease activity
There was no significant difference in systemic disease activity in patients with and without S. aureus colonization. The risk of relapse, relapse rate and BVAS3 at last visit were similar in patients with and without S. aureus colonization as shown in Table 2. With regard to local disease activity, 15 (50.0%) of the S. aureus colonized patients had at least one ENT relapse during follow-up compared to 25 (59.5%) of the S. aureus negative patients (P = 0.42). Four (11.4%) S. aureus colonized patients compared to three (6.4%) patients with a negative S. aureus test developed a saddle nose deformity (P = 0.42). Due to missing data not all 100 patients were included in each univariate analysis. For an overview of the number of included patients per each analysis, see supplementary table A.
Regression analysis showed that when corrected for gender, age at onset, AAV type, follow-up time and use of nasal steroids, there was no difference in relapse number per patient year between AAV patients colonized with S. aureus versus non-colonized patients (RR 2.03; P = 0.06) as shown in Table 3. Also, no difference was found in ENT relapses (OR 0.13; P = 0.14) and saddle nose deformity (OR 0.61; P = 0.74) between patients with and without S. aureus colonization.
Antibiotic treatment and disease activity
Of the 44 patients with S. aureus colonization, 28 (63.6%) patients received antibiotics aimed to eradicate S. aureus. In the 56 patients without S. aureus colonization, 12 (21%) received antibiotics. No data was available concerning antibiotic use from four of 44 S. aureus colonized patients.
No statistically significant difference in systemic and local disease activity was found between AAV patients colonized with S. aureus that received antibiotics for S. aureus eradication compared with patients colonized with S. aureus not receiving these antibiotics, as shown in Table 4. The number of patients was too small for regression analysis. Due to missing data not all 40 patients were included in each univariate analysis. For an overview of the number of included patients per each analysis, see Supplementary table B.
Discussion
Our study shows no difference in systemic and local disease activity between the patients colonized with S. aureus and S. aureus negative patients. Neither did we observe an effect of antibiotics on local and systemic disease activity.
These outcomes are in line with results from a prospective observational cohort study by Tan et al. [13]. In this study, adult AAV patients were observed for 4 years. No association was found between nasal S. aureus colonization and the extent of symptoms. Low-dose cotrimoxazole (dosage 400–80 mg/day), achieved less nasal S. aureus colonization over time. However, no effect on AAV evolution was observed.
In contrast to our findings, Salmela et al. did find an association between v and disease activity suggesting that S. aureus could play a role in triggering more active GPA [10]. In a prospective multicentre survey study (SAVAS), based on two randomized controlled trials, a significant association between chronic S. aureus nasal colonization and relapse rate in generalized AAV and in early systemic AAV was observed. Chronic nasal S. aureus colonization was almost exclusively seen in GPA patients and therefore only GPA patients were included. No data from MPA or EGPA patients were included in the analyses.
It is possible that S. aureus is found more often in patients with chronically active ENT disease as a result of local damage, creating an opportunity for S. aureus to colonize patients. In this scenario chronic S. aureus colonization is a result of active disease rather than a causative factor. This would also explain why a single positive swab does not necessarily has to relate with disease activity, as was found in our and other studies [13, 24].
Also, the absence of difference between the S. aureus positive and negative group in disease activity, could indicate that S. aureus may play only a minor pathogenic role. Research from Rhee et al. examined nasal microbiota (bacteria and fungi) in GPA patients and compared this to healthy controls [25]. They found that GPA patients compared to healthy individuals, had a significantly different microbial composition and had dysbiosis in the nose resulting in a lower prevalence of Propionibacterium acnes and Staphylococcus epidermidis which both compete with S. aureus [26, 27]. However they found no difference in the abundance of S. aureus between GPA and controls in contrast to previous studies [28, 29]. Rhee et al. suggested that manipulation of the nasal microbiome could be a novel therapeutic target [25]. This could mean that the role of solely S. aureus colonization in AAV pathophysiology is smaller than assumed.
With regard to antibiotic use, we found no beneficial effect on disease activity. According to Salmela et al. the use of cotrimoxazole treatment in low doses did not influence the relapse risk even though the rate of chronic nasal S. aureus colonization was almost completely prevented [10]. The absence of effect of antibiotics on disease activity is in line with our findings as well as the findings of Tan et al. but in strong contrast with Stegeman et al. who performed a prospective, randomized, placebo-controlled study to evaluate the efficacy of high dose cotrimoxazole in preventing relapses in GPA patients [9]. This study consisted of a group of 41 patients receiving cotrimoxazole and 40 patients received placebo. GPA patients with and without ENT involvement were enrolled. They found that cotrimoxazole in a dosage of 960 mg twice daily for a period of 24 months, reduced the incidence of ENT relapses in GPA patients and the use of cotrimoxazole was identified as a factor related to disease free interval. A potential explanation for the lack of effect of antibiotics on disease activity in our study and others could be the lower dosages used [10, 13, 21]. In our study different dosages and duration of antibiotics were used, and a small group of patients used the higher dosage of 960 mg of cotrimoxazole twice daily. Unfortunately, subgroup analysis was not possible due to small group size. Furthermore, patients included in the randomized, placebo-controlled trial from Stegeman et al. were patients with GPA in remission in contrast to our study were no difference was made in remission or active disease.
Limitations of our study include the small number of patients tested for S. aureus colonization and the small group of patients receiving antibiotic treatment. Due to the retrospective design of our study, there were missing data on duration of antibiotic treatment and confounding by indication could have occurred. Also, some patients did not receive antibiotic treatment aimed at S. aureus colonization but did receive cotrimoxazole as prophylaxis for Pneumocystis jiroveci-pneumonia. This could have been a confounder not being corrected for. Lastly, we defined S. aureus colonization as at least one positive test during follow-up time, therefore no differentiation between intermittent and chronic carriers could be made.
In conclusion, in this retrospective cohort study in AAV patients with ENT involvement, no difference was found in local and systemic disease activity between patients with and without nasal S. aureus colonization. In case of nasal S. aureus colonization, antibiotic treatment did not influence local or systemic disease activity. It is therefore possible that S. aureus plays a smaller role in AAV than previously thought. The role of antibiotic treatment in AAV patients colonized with S. aureus on AAV disease activity needs to be prospectively evaluated in a larger cohort.
References
Kallenberg CGM (2010) Pathophysiology of ANCA-associated small vessel vasculitis. Curr Rheumatol Rep 12:399–405. https://doi.org/10.1007/s11926-010-0138-6
Kallenberg CGM, Stegeman CA, Abdulahad WH, Heeringa P (2013) In translation pathogenesis of ANCA-associated vasculitis: new possibilities for intervention. Am J Kidney Dis 62:1176–1187. https://doi.org/10.1053/j.ajkd.2013.05.009
Jennette JC (2013) Overview of the 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Clin Exp Nephrol 17:603–606. https://doi.org/10.1007/s10157-013-0869-6
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F et al (2013) 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. ARTHRITIS Rheum 65:1–11. https://doi.org/10.1002/art.37715
Tadema H, Heeringa P, Kallenberg CGM (2011) Bacterial infections in Wegener’s granulomatosis: mechanisms potentially involved in autoimmune pathogenesis. Curr Opin Rheumatol 23:366–371. https://doi.org/10.1097/BOR.0b013e328346c332
Min C, Kallenberg CGM (2010) ANCA-associated vasculitides–advances in pathogenesis and treatment. Nat Rev Rheumatol 6:653–664
Stegeman CA, Cohen Tervaert JW, Sluiter WJ, Manson WL, de Jong PE, Kallenberg CGM (1994) Association of chronic nasal carriage of Staphylococcus aureus and higher relapse rates in Wegener granulomatosis. Ann Intern Med 1994(120):12–17
Popa ER, Stegeman CA, Abdulahad WH, Van Der Meer B, Arends J, Manson WM et al (2007) Staphylococcal toxic-shock-syndrome-toxin-1 as a risk factor for disease relapse in Wegener’s granulomatosis. Rheumatology 46:1029–1033
Stegeman CA, Cohen Tervaert JW, de Jong PE, Kallenberg CGM (1996) Trimethoprim-sulfamethoxazole (co-trimoxazole) for the prevention of relapses of Wegener’s granulomatosis. N Engl J Med 335:16–20
Salmela A, Rasmussen N, Tervaert JWC, Jayne DRW, Ekstrand A (2017) Chronic nasal Staphylococcus aureus carriage identifies a subset of newly diagnosed granulomatosis with polyangiitis patients with high relapse rate. Rheumatol (United Kingdom) 56:965–972. https://doi.org/10.1093/rheumatology/kex001
Brons RH, Bakker HI, Van Wijk RT, Van Dijk NW, Muller Kobold AC, Limburg PC et al (2000) Staphylococcal acid phosphatase binds to endothelial cells via charge interaction; a pathogenic role in Wegener’s granulomatosis? Clin Exp Immunol 119:566–573
Geetha D, Jefferson JA (2019) ANCA-associated vasculitis: core curriculum 2020. Am J Kidney Dis 75:124–137. https://doi.org/10.1053/j.ajkd.2019.04.031
Tan BK, Crabol Y, Tasse J, Dé Laurent FR, Nekkab N, Vinter C et al (2020) No evident association of nasal carriage of Staphylococcus aureus or its small-colony variants with cotrimoxazole use or ANCA-associated vasculitis relapses. Rheumatol 59:77–83. https://doi.org/10.1093/rheumatology/kez236
Lamprecht P, Fischer N, Huang J, Burkhardt L, Lütgehetmann M, Arndt F et al (2019) Changes in the composition of the upper respiratory tract microbial community in granulomatosis with polyangiitis. J Autoimmun 97:29–39. https://doi.org/10.1016/j.jaut.2018.10.005
Kallenberg CGM, Tadema H (2008) Vasculitis and infections: Contribution to the issue of autoimmunity reviews devoted to ‘autoimmunity and infection.’ Autoimmun Rev 8:29–32. https://doi.org/10.1016/j.autrev.2008.07.020
Karthikeyan S, Nitya Venkataraman AMC (2009) Staphylococcus aureus nasal carriage and its contributing factors. Future Microbiol 4:999–1008. https://doi.org/10.2217/fmb.09.79.Staphylococcus
Stegeman CA, Cohen Tervaert JW, de Jong PE, Kallenberg CGM (2018) Trimethoprim-sulfamethoxazole and antineutrophil cytoplasmic antibodies-associated vasculitis. Curr Op Rheumatol 30:388–394. https://doi.org/10.1097/BOR.0000000000000508
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T et al (2016) EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis 75:1583–1594. https://doi.org/10.1136/annrheumdis-2016-209133
DeRemee RA, McDonald TJ, Weiland LH (1985) Wegener’s granulomatosis: observations on treatment with antimicrobial agents. Mayo Clin Proc 60:27–32. https://doi.org/10.1016/S0025-6196(12)65279-3
Zycinska K, Wardyn KA, Zielonka TM, Krupa R, Lukas W (2009) Co-trimoxazole and prevention of relapses of PR3-ANCA positive vasculitis with pulmonary involvement. Eur J Medi 14:265–267
Kallenberg CGM (2011) What is the evidence for prophylactic antibiotic treatment in patients with systemic vasculitides ? Curr Opin Rheumatol 23:311–316. https://doi.org/10.1097/BOR.0b013e328344f323
Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S et al (2009) Modification and validation of the Birmingham vasculitis activity score (version 3). Ann Rheum Dis 68:1827–1832. https://doi.org/10.1136/ard.2008.101279
Moltó A, Dougados M (2014) Comorbidity indices. Clin Exp Rheumatol 32:S131–S134
Besada E, Koldingsnes W, Nossent JC (2015) Staphylococcus Aureus carriage and long-term rituximab treatment for granulomatosis with polyangiitis. PeerJ 2015:1–13. https://doi.org/10.7717/peerj.1051
Rhee RL, Sreih AG, Najem CE, Grayson PC, Zhao C, Bittinger K et al (2018) Characterisation of the nasal microbiota in granulomatosis with polyangiitis. Ann Rheum Dis 77:1448–1453. https://doi.org/10.1136/annrheumdis-2018-213645
Wagner J, Harrison EM, Martinez Del Pero M, Blane B, Mayer G, Leierer J et al (2019) The composition and functional protein subsystems of the human nasal microbiome in granulomatosis with polyangiitis: a pilot study. Microbiome. https://doi.org/10.1186/s40168-019-0753-z
Lina G, Boutite F, Tristan A, Bes M, Etienne J, Vandenesch F (2003) Bacterial competition for human nasal cavity colonization: role of Staphylococcal agr alleles. Appl Environ Microbiol 69:18–23
Popa ER, Stegeman CA, Kallenberg CGM, Tervaert JWC (2002) Staphylococcus aureus and Wegener’s granulomotosis. Arthritis Res 4:77–79. https://doi.org/10.1186/ar392
Tadema H, Abdulahad WH, Stegeman CA, Kallenberg CGM, Heeringa P (2011) Increased expression of toll-like receptors by monocytes and natural killer cells in ANCA-associated vasculitis. PLoS ONE. https://doi.org/10.1371/journal.pone.0024315
Funding
No funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no conflicts of interest. All co-author’s take full responsibility for the accuracy and integrity of all aspects of this manuscript.
Ethical approval
This study was classified by the Medical Research Ethics Committee Utrecht as exempt from the Medical Research Involving Human Subjects Act on the 12th of May 2020 (reference number WAG/mb/20/017914). There is no medical scientific research according to the definition of the Central Committee on Research Involving Human Subjects and participants were not subjected to procedures or required to follow rules of behaviour.
Informed consent
Informed consent from all participants cannot reasonably be expected given the retrospective nature and purpose of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
296_2022_5228_MOESM1_ESM.docx
The effect of nasal Staphylococcus aureus colonization and antibiotic treatment on disease activity in ANCA-associated vasculitis1 (DOCX 19 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schaap, C.M., Krol, R.M., Remmelts, H.H.F. et al. The effect of nasal Staphylococcus aureus colonization and antibiotic treatment on disease activity in ANCA-associated vasculitis: a retrospective cohort study in the Netherlands. Rheumatol Int 43, 467–475 (2023). https://doi.org/10.1007/s00296-022-05228-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05228-8