Abstract
Objective
To assess the effect of 4 years of anti-inflammatory therapy on markers of subclinical vascular disease in rheumatoid arthritis patients.
Methods
Carotid intima media thickness (IMT), augmentation index (AIx@75) and pulse wave velocity (PWV) measurements were performed repeatedly in 61 RA patients (30 early RA starting with csDMARDs and 31 established RA starting with adalimumab) for 4 years. These markers were also measured in 29 controls with osteoarthritis at baseline (BL).
Results
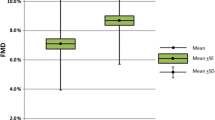
IMT and AIx@75 at BL were higher in RA compared to OA, while PWV was higher in OA. In RA patients, AIx@75 and PWV decreased in the first 6 months after starting anti-inflammatory therapy. At 48 M, the level of AIx@75 remained lower than before therapy, while PWV at 48 M was comparable to BL (AIx@75: BL 28% (95% confidence interval 25–30%), 6 M 23% (20–26%), 48 M 25% (22–28%); PWV: BL 8.5 (7.8–9.2), 6 M 8.0 (7.1–8.9), 48 M 8.6 (7.6–9.6) m/s). IMT remained stable. There was an effect of disease activity (longitudinally, adjusted for changes over time) on IMT, AIx@75 and PWV.
Conclusion
This study suggests modest beneficial changes in some surrogate markers of subclinical vascular disease after anti-inflammatory therapy. These changes were associated with improvement in disease activity markers. Whether or not these beneficial changes ultimately predict a reduction in clinicalcardiovascular endpoints remains to be established in prospective studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic disease characterized by systemic inflammation, mainly affecting the joints. RA is associated with an increased risk of cardiovascular disease (CVD) and CVD-associated mortality [1,2,3]. Traditional cardiovascular (CV) risk factors in RA only partly explain the increased CVD risk in these patients. This suggests that chronic systemic inflammation itself contributes to (accelerated) atherosclerotic plaque development and/or instability [1, 4, 5]. Strategies to reduce CV risk in RA are modification of traditional risk factors (e.g. lifestyle recommendations, antihypertensive treatment, and cholesterol lowering agents), but accumulating evidence suggest that anti-inflammatory treatment (e.g. with conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs) or biological DMARDs (bDMARD, such as TNF-blockers) also reduces CV risk in RA patients [6,7,8,9].
Established markers for subclinical vascular disease are carotid intima media thickness (IMT; thickness of inner layer of the arterial wall), pulse wave velocity (PWV; represents arterial wall stiffness) and augmentation index (AIx; another measure for arterial stiffness) [10,11,12,13]. These markers are often used in trials to assess the effect of interventions on CV risk [14]. Studies to assess whether short-term anti-inflammatory therapy (follow-up period ranging between 1 and 12 months) has a favorable effect on these surrogate markers are inconclusive [15,16,17,18]. This is the first study to investigate the long-term effect of anti-inflammatory.
The aim of this explorative study was to assess the effect of 4 years of anti-inflammatory therapy on IMT, AIx and PWV in RA patients. Insight in these surrogate markers and the changes over time after anti-inflammatory treatment can provide additional information on the treatment of cardiovascular comorbidities in RA.
Methods
Study participants
Participants with active RA (i.e. disease activity score of 28 joints with erythrocyte sedimentation rate (DAS28-ESR) ≥ 4) of ≥ 50 years starting with anti-inflammatory treatment, and age-and sex-matched osteoarthritis (OA) controls, were recruited between October 2011 and February 2017 from outpatient clinics of the departments of Rheumatology of Reade and Amsterdam UMC, location VUmc, Amsterdam, the Netherlands, as described previously [19, 20]. Exclusion criteria were active tuberculosis or other severe infections, pregnancy, moderate to severe heart failure (NYHA class III/IV), cancer, and life expectancy < 12 months. Patients were categorized into three groups: (1) newly diagnosed patients with early RA, not yet on DMARD therapy, and starting with methotrexate (MTX) or another csDMARD (sulfasalazine or hydroxychloroquine, whether or not combined with short-term glucocorticoids), (2) patients with established RA, already on csDMARDs, and starting with a first biological DMARD (adalimumab) in combination to the csDMARDs they already used prior to the study and (3) age- and sex-matched controls with OA of the knee or hip, not using DMARD of corticosteroid therapy. The study was approved by the Slotervaartziekenhuis and Reade medical ethics committee (protocol number: NL34047.048.10, approval date: 23–12-2010) and a written informed consent form was obtained from all participants, according to the principles of the Declaration of Helsinki.
Study visits
For RA patients, study visits were scheduled at baseline (BL) and 6, 12, 24, 36 and 48 months after starting treatment. Patients who discontinued treatment of interest (csDMARDs for early RA and adalimumab for established RA) during follow-up were excluded as per protocol, but they were invited for the 6- and 48-month visits to be included in the intention-to-treat analysis. Therefore, intention-to-treat analysis only includes the visits at BL, 6 and 48 months. OA controls were measured once, in order to cross-sectionally compare baseline measurements in RA with a group of patients that also suffers from joint problems and subsequent mobility limitations (resulting in lower physical activity), but without systemic inflammation.
Surrogate markers
Surrogate markers (IMT, AIx@75 and PWV) were measured by three observers (ABB, RA, AMvS), all trained by the same trainers of the Clinical Research Unit, Internal Medicine, Amsterdam UMC, location VUmc. Each observer performed a reproducibility test with the trainer before starting to perform measurements (a maximum of 10% inter- and intra-observer variability was allowed).
Mean carotid IMT of three measurements 10 mm proximal to the carotid bifurcation in the right common carotid artery (far wall) was acquired using Artlab echotracking system with a 7.5 MHz linear probe (Esaote, Maastricht, the Netherlands), according to Mannheim consensus [21]. Pulse wave analysis was performed with applanation tonometry (SphygmoCor, AtCor medical, Sydney, Australia). Carotid and femoral pulse waves were measured sequentially and gated by a simultaneously recorded ECG signal. Carotid-femoral PWV was determined by the transit time of the pulse wave between the carotid and femoral artery divided by the distance between the two recording sites (m/s). For AIx, the central aortic waveform was mathematically derived from the radial pulse wave. AIx was then determined by subtracting the first from the second (the augmented) systolic pressure peak of the central aortic waveform and expressed as a percentage of the pulse pressure. Mean of three measurements was taken and normalized to heart rate of 75 beats/minute (AIx@75).
Clinical assessments
Demographic data, medical history, medication use, smoking status, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), DAS28-CRP, health assessment questionnaire (HAQ), blood pressure (BP), heart rate, hypertension (systolic BP > 140 mmHg and/or diastolic BP > 90 mmHg and/or currently on antihypertensive treatment), body mass index (BMI), total cholesterol (TC), high-density lipoprotein cholesterol (HDLc), low-density lipoprotein cholesterol (LDLc) and triglycerides (TG) were assessed at all visits. Good response to therapy was defined as achieving low disease activity on DAS28-CRP after 6 months, with low disease activity defined as DAS28-CRP < 2.7, according to [22]).
Statistical analysis
Data are presented as mean ± standard deviation (SD) for normally distributed variables, median with interquartile range (IQR) for skewed continuous variables, or frequencies for categorical variables. Normality of dependent variables, or residuals after regression analysis, were assessed by visual inspection of the histogram and quantile–quantile plot. For regression analyses, linearity and homoscedasticity were assessed by plotting residuals versus predicted values and observed versus predicted values. Cross-sectional differences in surrogate markers between the groups were assessed with independent t test. Longitudinal analysis was done with linear mixed-effect models, allowing adjustment for the potential correlations between repeated measurements within the same patients over time. A random intercept was added to all models, while log-rank test was done to determine whether a random slope (with unstructured correlation matrix) was necessary. Because of slight heteroscedasticity (mainly for PWV), robust standard errors were estimated. For the analysis comparing response versus non-response, a visit was marked as good response if the patient had DAS28-CRP < 2.7 during that visit. To analyze the effect of four estimates of disease activity (ESR, CRP, DAS28-CRP and HAQ) on the surrogate markers, adjusting for the changes over time, we used univariate linear mixed effect models with time added as covariate to the model. For this analysis, standardized regression coefficients are reported, representing the number of SDs that the surrogate markers change, when the independent variable changes one SD. Data analysis was performed using SPSS version 24 and STATA SE 13.
Results
The study population consisted of 61 RA patients (30 early RA and 31 established RA patients) and 29 age-and-sex-matched controls with OA. Baseline characteristics are shown in Table 1. During the 48 months follow-up, 19 (32%) patients dropped out (n = 6, 5, 2, 3 and 3 at month 6, 12, 24, 36 and 48, respectively). Reasons were withdrawal of informed consent (n = 6), lost-to-follow-up (n = 7) and death (n = 6). In total, 227 visits were performed, and IMT, AIx@75 and PWV were measured in 92%, 84% and 73% of the visits, respectively. Main reasons for not having a measurement were material breakage, unavailability of equipment due to maintenance and measurement failure due to irregular heartbeat or weak signal because of cervical adipose tissue. The number of patients per visit is shown in Supplementary Fig. 1.
As shown in Table 1, 14 (23%) RA patients had a history of CVD at baseline, including cerebrovascular event (n = 6), acute coronary syndrome (n = 5), congestive heart failure (n = 1), peripheral artery disease (n = 1) and acute coronary syndrome plus congestive heart failure (n = 1). During follow-up, 2 patients developed CVD (fatal cerebrovascular event (n = 1) and non-fatal acute coronary syndrome (n = 1), both in early RA group) and 5 patients deceased of non-CVD related causes.
Cross-sectional comparison RA and OA patients
When comparing RA (all RA patients combined) with OA at baseline (Table 1), mean values of IMT and AIx@75 were slightly higher for the RA group (IMT: RA 0.67 ± 0.11 vs. OA 0.64 ± 0.09, p = 0.19, AIx@75: RA 28 ± 10 vs. OA 24 ± 10, p = 0.19). In contrast, PWV was higher in OA patients (RA 8.5 ± 2.5 vs. OA 9.9 ± 2.3, p = 0.053). Stratified analysis comparing early with established RA showed that all indices of subclinical vascular disease were highest for early RA patients, who also had highest RA disease activity and blood pressure (IMT: early RA 0.68 ± 0.10 vs. established RA 0.66 ± 0.12, AIx@75: early RA 29 ± 10 vs. established RA 27 ± 11, PWV: established RA 8.8 ± 2.3 vs. 8.2 ± 2.8, all statistically non-significant p > 0.05).
Longitudinal intention-to-treat analysis
In the early RA group, 23 (85%) patients had started with csDMARD monotherapy, 2 (7%) with methotrexate + other csDMARD(s) and 1 (4%) with csDMARD(s) other than methotrexate. In the established RA group, 4 (15%) patients had started with adalimumab as monotherapy and 21 (78%) as addition to the csDMARDs they were already using prior to the study (12 (44%) methotrexate, 2 (7%) other csDMARDs and 7 (26%) methotrexate + other csDMARDs). An overview of anti-inflammatory treatment use per study visit is shown in Supplemental Fig. 1. In total, 36 (59%) of the patients achieved low disease activity at 6 months after starting treatment (defined as ‘response’).
Longitudinal effect of anti-inflammatory treatment on surrogate markers and disease activity: Intention-to-treat analysis. Results of univariate linear mixed-effects models (with random intercept, and random slope when necessary (log-rank test)), with robust standard errors, AIx@75: augmentation index normalized to heart rate of 75 beats/minute, CRP: C-reactive protein, DAS28: disease activity score of 28 joints, IMT: intima media thickness, PWV: pulse wave velocity, RA: rheumatoid arthritis. Intention-to-treat analysis. For exact numbers refer to Supplemental Table 1
In the total group of RA patients, AIx@75 decreased in the first 6 months after starting anti-inflammatory therapy, while PWV showed a decreasing trend, particularly in responding patients (Fig. 1, Supplemental Table 1, p < 0.001 and p = 0.103, respectively). At 48 months, the level of AIx@75 still remained lower than before therapy (p = 0.016), while PWV at 48 months was comparable to that at BL (p = 0.900). In contrast, IMT seemed to slightly increase at 6 months (p = 0.257), but was comparable to BL at 48 months (p = 0.788).
Stratification for early and established RA showed that both IMT and PWV decreased over the 4 years for established RA, while increasing over time for early RA patients (non-significant, Supplemental Table 1). For AIx@75 there was no clear difference between the groups.
Stratification for response and non-response showed that mainly in the first 6 months there was a difference between these two groups: IMT remained stable in responders, while it increased in non-responders (p = 0.998 and p = 0.050, respectively), AIx@75 decreased slightly more for responders (p = 0.001 for responders, p = 0.150 for non-responders), and PWV decreased in responders, while increased in non-responders (p = 0.003 and p = 0.552, respectively) (Supplemental Table 1). For IMT and AIx, these minor short-term differences did not persist on long term.
Table 2 shows the effect of disease activity on IMT, AIx@75 and PWV, adjusted for time. All three surrogate markers were positively associated with serological inflammatory markers: when ESR or CRP increased with 1 SD, the surrogate markers increased with 0.09 to 0.24 SDs. In addition, DAS28-CRP and HAQ were positively associated with AI@75 and PWV (betas 0.19–0.24).
Longitudinal per protocol analysis
In total, 24 (39%) patients were excluded for the per protocol analysis, because of discontinuing treatment of interest during the 48-month period (csDMARDs for early RA or adalimumab for established RA). Reasons for discontinuing treatment were side effects (n = 12), treatment failure (n = 8), both side effects and treatment failure (n = 2), tapering due to good effect (n = 1) and practical reasons (n = 1). Results in patients actively on csDMARDs (early RA) or adalimumab (established RA) therapy (per protocol analysis, Supplemental Table 2), were comparable to the results in the total group of patients (intention-to-treat analysis, as described above).
Discussion
We performed an explorative study on surrogate markers for vascular disease in RA patients starting with anti-inflammatory treatment. To our knowledge, this is the first clinical study following patients for up to 4 years after starting with anti-inflammatory therapy. Our key findings were modest beneficial changes in vascular surrogate markers after anti-inflammatory treatment, and that these changes were associated with improvement in markers of disease activity. Altogether, the results can inform researchers planning new studies on assessing the effect of anti-inflammatory treatment on the arterial system and investigating which endpoints to use.
Previous studies investigating the effect of TNF inhibiting therapy on IMT, AIx and PWV have shown conflicting results [15,16,17,18]. A systematic review concluded that there is no strong evidence for an effect of TNF inhibiting therapy on IMT, AIx and PWV [17], whereas a meta-analysis concluded that the balance of evidence suggests a beneficial effect of TNF inhibiting therapy on AIx and PWV [18]. Results of studies concerning the effect of csDMARDs are also conflicting [23,24,25,26,27].
In our study, we observed a short-term effect of anti-inflammatory therapy on AIx@75 and PWV at 6 months, after which both increased again. AIx@75 was still lower at 48 months than at baseline, and PWV was at a comparable level as baseline. IMT seemed to remain rather stable over the 48 months. From previous research, it was expected that without an intervention these surrogate markers would increase over time due to aging [28, 29]. As the largest reduction in inflammation is achieved within the first 6 months, it is possible that a steady-state occurs after which no further decline can be expected, and subsequent increase in the surrogate markers is due to aging. However, we did not longitudinally measure the surrogate markers in our control group, and future research with additional longitudinal measurements in a control group is warranted to investigate whether there is a delay of deterioration in the vasculature as a result of the effect by anti-inflammatory therapy. In addition, the beneficial changes we found after anti-inflammatory therapy were modest, and it can be argued whether these are clinically relevant or not. This remains to be established in future prospective studies assessing the effect of anti-inflammatory therapy on long-term CVD risk in RA patients, which could also include additional measurements for arterial calcification such as multi-slice computed tomography, and other measures relevant in the context of arterial calcification, such as lipoprotein (a) and vitamin D levels.
A large proportion of the patients in the established RA group used glucocorticosteroids at baseline. While chronic treatment with prednisone increases the risk of atherosclerotic CVD, its effects on these markers for subclinical CVD are still unclear [30, 31].
Multiple measures for RA disease activity (serological inflammatory markers, composite measure for disease activity and questionnaire for functional disability status) were associated with IMT, AIx@75 and PWV, providing further support for a link between the reduction of systemic inflammation and arterial stiffness and arterial wall thickening.
For the cross-sectional comparison we included OA patients, as these also suffer from joint problems and subsequent mobility issues, but without auto-inflammatory characteristics. The included OA patients (matched on age and sex) had highest prevalence of previous CVD and hypertension. This might be responsible for the higher PWV in OA compared to RA.
Limitations of this study are a low sample size and rather high drop-out rate, increasing the risk of selection bias. In addition, measurements were performed by different investigators at different consecutive timepoints and we therefore cannot rule out a systematic measurement difference between timepoints. Nonetheless, all three investigators were tested for inter-rater reliability by the same trainer to minimize this observer bias.
In conclusion, this study has shown modest beneficial changes in some surrogate markers of subclinical vascular disease after anti-inflammatory therapy and these changes were associated with improvement in disease activity markers. Whether or not these beneficial changes ultimately lead to a significant reduction of clinically overt cardiovascular endpoints remains to be established in prospective studies.
References
Agca R, Heslinga SC, van Halm VP, Nurmohamed MT (2016) Atherosclerotic cardiovascular disease in patients with chronic inflammatory joint disorders. Heart 102(10):790–795. https://doi.org/10.1136/heartjnl-2015-307838
Peters MJ, van Halm VP, Voskuyl AE, Smulders YM, Boers M, Lems WF et al (2009) Does rheumatoid arthritis equal diabetes mellitus as an independent risk factor for cardiovascular disease? A prospective study. Arth Rheum 61(11):1571–1579. https://doi.org/10.1002/art.24836
van Halm VP, Peters MJ, Voskuyl AE, Boers M, Lems WF, Visser M et al (2009) Rheumatoid arthritis versus diabetes as a risk factor for cardiovascular disease: a cross-sectional study, the CARRE Investigation. Ann Rheum Dis 68(9):1395–1400. https://doi.org/10.1136/ard.2008.094151
Sattar N, McCarey DW, Capell H, McInnes IB (2003) Explaining how “high-grade” systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation 108(24):2957–2963. https://doi.org/10.1161/01.CIR.0000099844.31524.05
Libby P (2008) Role of inflammation in atherosclerosis associated with rheumatoid arthritis. Am J Med 121(10 Suppl 1):S21-31. https://doi.org/10.1016/j.amjmed.2008.06.014 (PubMed PMID: 18926166)
Tam LS, Kitas GD, Gonzalez-Gay MA (2014) Can suppression of inflammation by anti-TNF prevent progression of subclinical atherosclerosis in inflammatory arthritis? Rheumatology 53(6):1108–1119. https://doi.org/10.1093/rheumatology/ket454
Heathfield SK, Parker B, Zeef LA, Bruce IN, Alexander MY (2013) Certolizumab pegol attenuates the pro-inflammatory state in endothelial cells in a manner that is atheroprotective. Clin Exp Rheumatol 31(2):225–233
van Halm VP, Nurmohamed MT, Twisk JW, Dijkmans BA, Voskuyl AE (2006) Disease-modifying antirheumatic drugs are associated with a reduced risk for cardiovascular disease in patients with rheumatoid arthritis: a case control study. Arthritis Res Ther 8(5):R151. https://doi.org/10.1186/ar2045
Jacobsson LT, Turesson C, Gulfe A, Kapetanovic MC, Petersson IF, Saxne T et al (2005) Treatment with tumor necrosis factor blockers is associated with a lower incidence of first cardiovascular events in patients with rheumatoid arthritis. J Rheumatol 32(7):1213–1218
Tardif JC, Heinonen T, Orloff D, Libby P (2006) Vascular biomarkers and surrogates in cardiovascular disease. Circulation 113(25):2936–2942. https://doi.org/10.1161/CIRCULATIONAHA.105.598987
Bots ML (2006) Carotid intima-media thickness as a surrogate marker for cardiovascular disease in intervention studies. Curr Med Res Opin 22(11):2181–2190. https://doi.org/10.1185/030079906X148472
Lim HE, Park CG, Shin SH, Ahn JC, Seo HS, Oh DJ (2004) Aortic pulse wave velocity as an independent marker of coronary artery disease. Blood Press 13(6):369–375. https://doi.org/10.1080/08037050410004800
Rosenbaum D, Giral P, Chapman J, Rached FH, Kahn JF, Bruckert E et al (2013) Radial augmentation index is a surrogate marker of atherosclerotic burden in a primary prevention cohort. Atherosclerosis 231(2):436–441. https://doi.org/10.1016/j.atherosclerosis.2013.10.004
Bots ML, Evans GW, Riley WA, Grobbee DE (2003) Carotid intima-media thickness measurements in intervention studies: design options, progression rates, and sample size considerations: a point of view. Stroke 34(12):2985–2994. https://doi.org/10.1161/01.STR.0000102044.27905.B5
Mangoni AA, Baghdadi LR, Shanahan EM, Wiese MD, Tommasi S, Elliot D et al (2017) Methotrexate, blood pressure and markers of arterial function in patients with rheumatoid arthritis: a repeated cross-sectional study. Ther Adv Musculoskel Dis 9(9):213–229. https://doi.org/10.1177/1759720X17719850
Furer V, Fayad ZA, Mani V, Calcagno C, Farkouh ME, Greenberg JD (2012) Noninvasive cardiovascular imaging in rheumatoid arthritis: current modalities and the emerging role of magnetic resonance and positron emission tomography imaging. Semin Arthritis Rheum 41(5):676–688. https://doi.org/10.1016/j.semarthrit.2011.08.007
Knowles L, Nadeem N, Chowienczyk PJ (2020) Do anti-tumour necrosis factor-alpha biologics affect subclinical measures of atherosclerosis and arteriosclerosis? A systematic review. Br J Clin Pharmacol 86(5):837–851. https://doi.org/10.1111/bcp.14215
Vlachopoulos C, Gravos A, Georgiopoulos G, Terentes-Printzios D, Ioakeimidis N, Vassilopoulos D et al (2018) The effect of TNF-a antagonists on aortic stiffness and wave reflections: a meta-analysis. Clin Rheumatol 37(2):515–526. https://doi.org/10.1007/s10067-017-3657-y
Agca R, Blanken AB, van Sijl AM, Smulders YM, Voskuyl AE, van der Laken C et al (2021) Arterial wall inflammation is increased in rheumatoid arthritis compared with osteoarthritis, as a marker of early atherosclerosis. Rheumatology. https://doi.org/10.1093/rheumatology/keaa789
Blanken AB, Agca R, van Sijl AM, Voskuyl AE, Boellaard R, Smulders YM et al (2021) Arterial wall inflammation in rheumatoid arthritis is reduced by anti-inflammatory treatment. Semin Arthritis Rheum 51(2):457–463. https://doi.org/10.1016/j.semarthrit.2021.03.008
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovascular diseases. 2012;34(4):290–6. doi: https://doi.org/10.1159/000343145.
Inoue E, Yamanaka H, Hara M, Tomatsu T, Kamatani N (2007) Comparison of Disease Activity Score (DAS)28- erythrocyte sedimentation rate and DAS28- C-reactive protein threshold values. Ann Rheum Dis 66(3):407–409. https://doi.org/10.1136/ard.2006.054205
Kim HJ, Kim MJ, Lee CK, Hong YH (2015) Effects of methotrexate on carotid intima-media thickness in patients with rheumatoid arthritis. J Korean Med Sci 30(11):1589–1596. https://doi.org/10.3346/jkms.2015.30.11.1589
Pinto MRC, Kakehasi AM, Souza AJ, Tavares WC Jr, Rocha MA, Trant C et al (2019) Methotrexate use, not interleukin 33, is associated with lower carotid intima-media thickness in patients with rheumatoid arthritis. Adv Rheumatol 59(1):15. https://doi.org/10.1186/s42358-019-0060-1
Tam LS, Shang Q, Li EK, Wang S, Li RJ, Lee KL et al (2012) Infliximab is associated with improvement in arterial stiffness in patients with early rheumatoid arthritis – a randomized trial. J Rheumatol 39(12):2267–2275. https://doi.org/10.3899/jrheum.120541
Ferrante A, Giardina AR, Ciccia F, Parrinello G, Licata G, Avellone G et al (2009) Long-term anti-tumour necrosis factor therapy reverses the progression of carotid intima-media thickness in female patients with active rheumatoid arthritis. Rheumatol Int 30(2):193–198. https://doi.org/10.1007/s00296-009-0935-2
Mazzoccoli G, Notarsanto I, de Pinto GD, Dagostino MP, De Cata A, D’Alessandro G et al (2010) Anti-tumor necrosis factor-alpha therapy and changes of flow-mediated vasodilatation in psoriatic and rheumatoid arthritis patients. Intern Emerg Med 5(6):495–500. https://doi.org/10.1007/s11739-010-0458-6
Diaz A, Tringler M, Wray S, Ramirez AJ, Cabrera Fischer EI (2018) The effects of age on pulse wave velocity in untreated hypertension. J Clin Hypertens 20(2):258–265. https://doi.org/10.1111/jch.13167
Su TC, Chien KL, Jeng JS, Chen MF, Hsu HC, Torng PL et al (2012) Age- and gender-associated determinants of carotid intima-media thickness: a community-based study. J Atheroscler Thromb 19(9):872–880. https://doi.org/10.5551/jat.10728
Dalbeni A, Giollo A, Bevilacqua M, Cioffi G, Tagetti A, Cattazzo F et al (2020) Traditional cardiovascular risk factors and residual disease activity are associated with atherosclerosis progression in rheumatoid arthritis patients. Hypertension Res 43(9):922–928. https://doi.org/10.1038/s41440-020-0441-1
MacLeod C, Hadoke PWF, Nixon M (2021) Glucocorticoids: Fuelling the Fire of Atherosclerosis or Therapeutic Extinguishers? Int J Mol Sci. https://doi.org/10.3390/ijms22147622
Acknowledgements
We gratefully thank Ingrid Knufman and Jeannette Boerop for excellent assistance with blood sampling and measurement support, and Inge Goldhoorn for your profound data entry activities. In addition, we thank all the patients of the outpatient clinics of Reade and Amsterdam UMC, location VUmc who participated in this study.
Funding
This study was partly financially supported by AbbVie.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael T. Nurmohamed declares to have received consulting fees from AbbVie, Celgene, Celltrion, Eli Lilly, Janssen, and Sanofi, speaker’s fees from AbbVie, Bristol-Myers Squibb, Eli Lilly, Roche, and Sanofi, and research funding from AbbVie, Bristol-Myers Squibb, Celgene, Eli Lilly, Janssen, MSD, Grunenthal, Mundipharma, Novartis, Pfizer, Roche, and Sanofi. All other authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blanken, A.B., Raadsen, R., Agca, R. et al. Effect of anti-inflammatory therapy on vascular biomarkers for subclinical cardiovascular disease in rheumatoid arthritis patients. Rheumatol Int 43, 315–322 (2023). https://doi.org/10.1007/s00296-022-05226-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05226-w