Abstract
To examine the association between common comorbidities, eGFR and loci involved in the hyperuricaemia-gout transition. This study was conducted in people with gout from the UK Biobank. Logistic regression was used to examine the association between self-reported physician-diagnosed hypertension, diabetes, hypercholesterolemia and ischaemic heart disease (IHD) with the following variants: rs1260326(GCKR), rs16890979(SLC2A9), rs2231142(ABCG2), rs1229984(ADH1B) and rs2078267(SLC22A11) and adjusted for age, sex and 10-principal components. Linear regression was used to examine the association with eGFR. 7,049 participants with gout were included. After adjusting for multiple testing, there was a statistically significant positive association between urate lowering allele at SLC2A9 and hypertension, and negative association between urate raising allele at ABCG2 and hypertension (OR 1.17 and OR 0.86, respectively). Number of urate lowering risk alleles associated with hypertension [OR (95%CI) 1.13 (1.06–1.21)]. High eGFR associated with urate raising allele at rs2231142 (β = 1.38). The SNP in ADH1B that protects from alcohol excess showed a negative association with IHD (OR 0.53). Unlike in general population studies urate lowering genetic variants associate with hypertension in gout patients with dose–response. This may be due to high prevalence of other risk factors of hypertension such as obesity, poor diet etc. and needs validation in independent datasets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gout is a common inflammatory arthritis and is associated with comorbidities such as hypertension, ischaemic heart disease (IHD) and chronic kidney disease (CKD) in observational studies [1, 2]. However, mendelian randomisation (MR) studies that have tested causality gave a conflicting picture with genetic urate variants associated with some comorbidities i.e. hypertension, IHD, hypercholesterolemia, but not with other comorbidities e.g. CKD and diabetes [3,4,5,6,7]. A meta-analysis of genome-wide association studies (GWAS) in 5 population-based cohorts of the Cohorts for Heart and Aging Research in Genome Epidemiology consortium (n = 28 283) did not find an association between genetic urate score and blood pressure, glucose, CKD, or coronary heart disease [8]. Other studies have reported a negative association between urate genetic risk score and blood pressure [9]. However, these studies were conducted in the general population.
Recent GWAS identified genetic variants in urate transporters (ABCG2, SLC2A9, SLC22A11) and metabolic genes (GCKR, ADH1B) to be associated with the transition from hyperuricaemia to gout [10], and several of these associated with serum urate (SU) and gout in previous studies [11,12,13,14,15]. Whether these genetic variants are associated with comorbidities in people with gout has not been examined before. This is an important question as comorbidities are common in gout and genetic variants involved in hyperuricemia-gout transition have associations beyond urate handling. For instance, the A allele at rs1229984 in ADH1B is associated negatively with IHD, while the T allele at rs1260326 in GCKR is associated with high triglyceride and low blood sugar levels in the general population [16, 17].
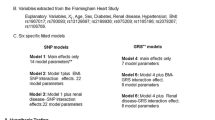
Thus, the purpose of this study was to examine the association between hypertension, diabetes, hypercholesterolemia, IHD, and estimated glomerular filtration rate (eGFR) and lead single nucleotide polymorphisms (SNPs) in urate transporter (rs16890979, rs2231142, and rs2078267 in SLC2A9, ABCG2, SLC22A11 respectively) and other genes (rs1260326 and rs1229984 in GCKR and ADH1B, respectively) associated with hyperuricaemia-gout transition.
Methods
Data source
This study was conducted using data from the United Kingdom (UK) Biobank (UK Biobank Project ID 45,987, approval date: 18th April 2019). The UK Biobank is a large population-based prospective study. Participants aged 40–69 years were recruited between 2006 and 2010 across England, Wales and Scotland. Data were collected on sociodemographic characteristics, lifestyle information, health status, family medical history and cognitive function. Physical and functional measurements were recorded and biological samples were collected for biomarkers measurements and genetic analyses. UK Biobank has approval from the North West Multi-Centre Research Ethics Committee (REC reference 16/NW/0274). This study did not involve re-contacting participants and no separate ethics approval was required. Details about recruitment and sample processing are described elsewhere [18].
Subjects
This research included UK Biobank participants with gout with genome-wide genotype data available (n = 7049). Exclusion criteria were non-European ethnicity, self-reported and genetic sex mismatches, kinship coefficients equivalent to second degree (or greater) relatives, call-rate < 90% and heterozygosity outliers [defined as ± 3 standard deviations (SD) from the mean]. Gout was defined as present if participants met any of the following criteria: self-reported physician diagnosed gout, urate-lowering treatment prescription without a hospital diagnosis of lymphoma or leukaemia, or a primary or secondary hospital diagnosis of gout using the International Classification of Diseases (ICD)-10 codes M10 (Gout), M100 (Idiopathic gout), M101 (Lead induced gout), M102 (Drug Induced Gout), M103 (Gout Due to Renal Impairment), M104 (Other Secondary Gout) and M109 (Gout, unspecified).
Study-design
Cases-control study
Separate case–control analyses were performed to examine the association between hypertension, diabetes mellitus, hypercholesterolemia and IHD with candidate SNPs. Cases were participants with hypertension, diabetes mellitus, hypercholesterolemia and IHD, respectively while controls did not have the index comorbidity. Comorbidities were categorised as present if they were self-reported as physician diagnosed.
Cross-sectional study
A cross-sectional study was conducted to examine the association between eGFR calculated using the CKD-EPI equation and candidate SNPs.
SNP selection and genotyping
A recent GWAS of gout cases and hyperuricaemic controls reported loci associated with hyperuricemia-gout transition [10]. From these loci, we selected the following key SNPs to perform the association analyses: rs1260326 (GCKR), rs16890979 (SLC2A9), rs2231142 (ABCG2), rs1229984 (ADH1B) and rs2078267 (SLC22A11). These SNPs were obtained from the directly genotyped UK Biobank data. Details about genotyping and the internal quality control (QC) procedures performed by the UK Biobank have been described previously [18]. The variants were evaluated to verify they did not deviate from Hardy–Weinberg equilibrium and had a call-rate > 95%.
Statistical analyses
Number (%) and SD were calculated for descriptive purposes. Independent sample t test and Χ2 test were used for comparing continuous and categorical data respectively. Logistic regression was used to examine the allelic association of each SNP included in the study with comorbidities of interest. The number of risk alleles in rs2231142 and rs16890979 were added (range 0–2) and included as a continuous independent variable in logistic regression to examine their association with hypertension. Linear regression was used to determine the allelic association between SNPs and eGFR. Analyses were adjusted for age, sex, body mass index (BMI) and the first 10 principal components (PCs). Adjusted odds ratios (aORs) and 95% confidence intervals (CI), or Beta coefficients and standard error (SE) were calculated as appropriate. Bonferroni correction was used to account for multiple testing. The obtained p values were multiplied by 25 to obtain Bonferroni corrected p values and, pcorr < 0.05 was regarded as statistically significant. Data were managed and analysed using Stata/MP, and PLINK V.1.9 was used for QC analyses.
Results
Data for 7049 gout cases (6479, 91.9% men) were included. Their mean (SD) age and body mass index was 60.09 (6.86) years and 30.74 (4.95) kg/m2 respectively. 2411 (34.2%), 1940 (27.5%), 1589 (22.5%), 406 (5.8%) and 693 (9.8%), participants self-reported alcohol consumption daily, 3–4 times/week, 1–2 times/week, < 1 per week and never or on special occasions respectively. The prevalence of current, ex- and non-smokers was 8.8% (n = 617), 50.3% (n = 3546), and 40.6% (n = 3560), respectively. The demographic characteristics of cases with index comorbidity and controls without comorbidity were comparable except for younger age in cases with diabetes compared to controls, and higher SU in cases with IHD (Supplementary Tables S1–S4).
There was an association between the T allele at rs16890979 (SLC2A9 gene) and hypertension with aOR (95%CI) 1.17 (1.06–1.29), pcorr 0.0355 (Table 1). There was also a negative association between T allele at rs2231142 (ABCG2 gene) and hypertension with aOR (95%CI) 0.86 (0.79–0.93), pcorr 0.0080 (Table 1). In previous studies, the T allele at rs16890979 and the G allele at rs2231142 have been associated with low SU level [8]. Thus, we defined the T allele at rs16890979 polymorphism and G allele at rs2231142 polymorphism [the G allele at rs2231142 associated with hypertension with aOR (95%CI) 1.16 (1.07–1.1.27)] as the risk alleles for exploring their additive effects on the association with hypertension. We observed that each additional risk allele increased the aOR (95%) for hypertension by 1.13 (1.06–1.21), with no risk allele referent (Table 2). The ORs increased progressively but were not significantly different for 1 or 2 alleles (Table 2). There was a statistically significant negative association between T allele at rs1229984 (ADH1B gene) and IHD [aOR (95%CI) 0.53 (0.38–0.74)], pcorr 0.0047. eGFR associated with T allele at rs2231142 (ABCG2 gene) with beta coefficient (SE) 1.38 (0.374), pcorr 0.0055. Additionally, there was a nominal association between T allele at rs1229984 and diabetes and eGFR associated with T allele at rs12603262 (GCKR gene) that was non-significant on accounting for multiple tests (Table 1).
Discussion
This study examined the genetic factors associated with comorbidities in gout. It reported a statistically significant negative association between SNPs in the ABCG2 and SLC2A9 genes that are associated with high SU and hypertension with evidence of dose response. There was a negative association between SNP in ADH1B gene and IHD, and an association between T allele at ABCG2 polymorphism associated with high urinary urate excretion, and higher eGFR [20].
The association between genetic variants associated with low SU and hypertension is counterintuitive and not consistent with most of the results of epidemiological and MR studies that reported an association between gout and hypertension, and urate variants and hypertension and systolic blood pressure, respectively [2,3,4, 7]. However, a study by Sumpter et al. reported a negative association of a genetic risk score mostly driven by variants in ABCG2 and ADH1B [OR 0.88 (0.78–0.99); OR 0.69 (0.54–0.89) respectively] with the presence of any comorbidity in gout [21]. Hyperuricaemia induced by urate under-excretion was observed to be causal in animal models of hypertension and further research is required to understand why this is different in people with gout [22]. However, in healthy adults, acute infusion of uric acid did not increase blood pressure or cause any cardiovascular haemodynamic effects [23]. Nevertheless, the results of the current study imply that genotyping for polymorphism at the SLC2A9 and ABCG2 genes may be useful when counselling gout patients about risk of hypertension and the need to take preventative measures.
Our finding of a negative association between polymorphisms in ADHB1 gene and IHD is consistent with previous reports in the general population and may be due to a protective effect on excessive alcohol intake and/or binge drinking from this polymorphism [24]. It underlines the importance of the need to advice to reduce excess alcohol intake in people with gout.
The association between T allele at rs2231142 and gout differs across ethnicities [25]. Moreover, the T allele at rs2231142 is more common in the South-East Asian ethnicities than in the white Caucasian population [26,27,28]. Converse is true for the G allele at rs2231142. Further research in other ethnicities is required to confirm if these findings of an association between SU lowering alleles and hypertension holds true across populations.
Strengths of this study included large sample size, evaluation of dose response, use of eGFR values as continuous variables rather than categorical CKD stages, recruitment from the general population, and correction for multiple testing. However, the study had several limitations. Comorbidities were self-reported as being physician diagnosed. This has the potential to affect the strength of association due to biassed recall and is a key limitation. However, participants in UK Biobank reported their health conditions with the support of a research nurse present. Moreover, data on these covariates have been used extensively in research using UK Biobank data. In a validation study, self-reported physician diagnosed comorbidities in the UK Biobank had the same association with mortality as comorbidities ascertained using hospitalisation records alone [29]. Similarly, as information on the presence of monosodium urate crystals, tophi, bone erosions and other radiographic findings typical of MSU crystal deposits are not included in the UK Biobank, gout status could only be ascertained using self-report of physician diagnosis, ULT prescription and hospitalisation codes. Although not 100% specific, this case definition strategy has high sensitivity and precision for detecting association in genetic epidemiological studies of gout [30]. Inclusion of hospital discharge diagnosis increased the potential for this definition to include cases with more severe gout that may not have been diagnosed in primary-care or treated with ULT. Participants were not required to meet the 2015 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) gout classification criteria as the UK Biobank baseline data collection occurred between 2006 and 2010, before the ACR/EULAR gout classification criteria had been published. This has the potential to reduce the validity of the results and our findings ought to be confirmed in independent datasets of gout cases meeting the ACR/EULAR classification criteria.
In conclusion, this study reported genetic factors associated with comorbidities in people with gout. The results may be used to risk-stratify gout cases for closer monitoring of comorbidities and for the use of primary prevention strategies. These results should also be validated in independent datasets, preferably in people from other ethnicities.
Data availability
Data used in this study were made available to the study team by the UK Biobank under study specific licence that does not allow us to make the data publicly available. Raw data used in the study may be obtained form the UK Biobank on application.
References
Zhu Y, Pandya BJ, Choi HK (2012) Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am J Med 125:679-687.e1. https://doi.org/10.1016/j.amjmed.2011.09.033
Singh JA, Gaffo A (2020) Gout epidemiology and comorbidities. Semin Arthritis Rheum 50:S11–S16. https://doi.org/10.1016/j.semarthrit.2020.04.008
Gill D, Cameron AC, Burgess S, Li X, Doherty DJ, Karhunen V et al (2021) Urate, blood pressure, and cardiovascular disease. Hypertension 77:383–392
Li X, Meng X, He Y, Spiliopoulou A, Timofeeva M, Wei W-Q et al (2019) Genetically determined serum urate levels and cardiovascular and other diseases in UK Biobank cohort: a phenome-wide mendelian randomization study. PLoS Med 16:e1002937
Jordan DM, Choi HK, Verbanck M, Topless R, Won H-H, Nadkarni G et al (2019) No causal effects of serum urate levels on the risk of chronic kidney disease: a Mendelian randomization study. PLoS Med 16:e1002725-e
Keerman M, Yang F, Hu H, Wang J, Wang F, Li Z et al (2020) Mendelian randomization study of serum uric acid levels and diabetes risk: evidence from the Dongfeng-Tongji cohort. BMJ Open Diabetes Res Care 8:e000834
McCormick N, O’Connor MJ, Yokose C, Merriman TR, Mount DB, Leong A et al (2021) Assessing the causal relationships between insulin resistance and hyperuricemia and gout using bidirectional Mendelian randomization. Arthritis Rheumatol 73:2096–2104
Yang Q, Köttgen A, Dehghan A, Smith AV, Glazer NL, Chen MH et al (2010) Multiple genetic loci influence serum urate levels and their relationship with gout and cardiovascular disease risk factors. Circ Cardiovasc Genet 3:523–530
Sedaghat S, Pazoki R, Uitterlinden AG, Hofman A, Stricker BHC, Ikram MA et al (2014) Association of uric acid genetic risk score with blood pressure. Hypertension 64:1061–1066
Sandoval-Plata G, Morgan K, Abhishek A (2021) Variants in urate transporters, ADH1B, GCKR and MEPE genes associate with transition from asymptomatic hyperuricaemia to gout: results of the first gout versus asymptomatic hyperuricaemia GWAS in Caucasians using data from the UK Biobank. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2020-219796
Dehghan A, Köttgen A, Yang Q, Hwang S-J, Kao WHL, Rivadeneira F et al (2008) Association of three genetic loci with uric acid concentration and risk of gout: a genome-wide association study. Lancet 372:1953–1961
Kottgen A, Albrecht E, Teumer A, Vitart V, Krumsiek J, Hundertmark C et al (2013) Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat Genet 45:145–154
Phipps-Green AJ, Merriman ME, Topless R, Altaf S, Montgomery GW, Franklin C et al (2016) Twenty-eight loci that influence serum urate levels: analysis of association with gout. Ann Rheum Dis 75:124–130
Matsuo H, Yamamoto K, Nakaoka H, Nakayama A, Sakiyama M, Chiba T et al (2016) Genome-wide association study of clinically defined gout identifies multiple risk loci and its association with clinical subtypes. Ann Rheum Dis 75:652–659
Li C, Li Z, Liu S, Wang C, Han L, Cui L et al (2015) Genome-wide association analysis identifies three new risk loci for gout arthritis in Han Chinese. Nat Commun 6:7041
Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z et al (2014) (2014) Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ (Clinical Research Ed) 349:g4164-g
Vaxillaire M, Cavalcanti-Proença C, Dechaume A, Tichet J, Marre M, Balkau B et al (2008) The common P446L polymorphism in GCKR inversely modulates fasting glucose and triglyceride levels and reduces type 2 diabetes risk in the DESIR prospective general French population. Diabetes 57:2253
Welsh S (2017) Genotyping of 500,000 UK Biobank participants: description of sample processing workflow and preparation of DNA for genotyping
Cadzow M, Merriman TR, Dalbeth N (2017) Performance of gout definitions for genetic epidemiological studies: analysis of UK Biobank. Arthritis Res Ther 19(1):181
Ichida K, Matsuo H, Takada T, Nakayama A, Murakami K, Shimizu T et al (2012) Decreased extra-renal urate excretion is a common cause of hyperuricemia. Nat Commun 3:764. https://doi.org/10.1038/ncomms1756
Sumpter N, Cadzow M, So A, Reynolds R, Merriman T (2020) Analysis of Common Gout Comorbidities in the UK Biobank Cohort Reveals Sex-Specific Effects and Genetic Differentiation [abstract]. Arthritis Rheumatol.2020; 72 (suppl 10). https://acrabstracts.org/abstract/analysis-of-common-gout-comorbidities-in-the-uk-biobank-cohort-reveals-sex-specific-effects-and-genetic-differentiation/. Accessed 29 April 2022
Mazzali M, Hughes J, Kim Y-G, Jefferson JA, Kang D-H, Gordon KL et al (2001) Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 38:1101–1106
Waring WS, Adwani SH, Breukels O, Webb DJ, Maxwell SR (2004) Hyperuricaemia does not impair cardiovascular function in healthy adults. Heart 90:155–159
Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z et al (2014) Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ (Clinical Research Ed) 349:g4164-g
Dong Z, Guo S, Yang Y, Wu J, Guan M, Zou H et al (2015) Association between ABCG2 Q141K polymorphism and gout risk affected by ethnicity and gender: a systematic review and meta-analysis. Int J Rheum Dis 18:382–391
Roman Y, Tiirikainen M, Prom-Wormley E (2020) The prevalence of the gout-associated polymorphism rs2231142 G>T in ABCG2 in a pregnant female Filipino cohort. Clin Rheumatol 39:2387–2392
Roman YM, Culhane-Pera KA, Menk J, Straka RJ (2016) Assessment of genetic polymorphisms associated with hyperuricemia or gout in the Hmong. Per Med 13:429–440
Zhang L, Spencer KL, Saroja Voruganti V, Jorgensen NW, Fornage M, Best LG et al (2013) Association of functional polymorphism rs2231142 (Q141K) in the ABCG2 Gene with serum uric acid and gout in 4 US populations: the PAGE study. Am J Epidemiol 177:923–932
Jani BD, Hanlon P, Nicholl BI, McQueenie R, Gallacher KI, Lee D et al (2019) Relationship between multimorbidity, demographic factors and mortality: findings from the UK Biobank cohort. BMC Med 17:74. https://doi.org/10.1186/s12916-019-1305-x
Cadzow M, Merriman TR, Dalbeth N (2017) Performance of gout definitions for genetic epidemiological studies: analysis of UK Biobank. Arthritis Res Ther 19:181. https://doi.org/10.1186/s13075-017-1390-1
Acknowledgements
The authors would like to thank all participants of the UK Biobank.
Funding
Miss Sandoval-Plata’s work is supported by a PhD scholarship from The Mexican National Council for Science and Technology (CONACYT) [Grant number 472298] and a research grant from Rosetrees Trust [Grant number M688].
Author information
Authors and Affiliations
Contributions
GS-P, KM and AA conceived the study. GS-P performed data analysis. GS-P, KM and AA interpreted the data. GS-P wrote first draft of the manuscript. AA and KM supervised the data analysis, reviewed the manuscript and provided intellectual input to the manuscript. GS-P, KM and AA approved the final version to be published. All co-authors take full responsibility for the accuracy and integrity of all aspects of the work. No external editing or writing support was received for this study.
Corresponding author
Ethics declarations
Conflict of interest
Dr Gabriela Sandoval-Plata was funded by a PhD scholarship from The Mexican National Council for Science and Technology (CONACYT). Prof A Abhishek has received departmental research grants from AstraZeneca and Oxford Immunotec, speaker bureau fees from Menarini, scientific meeting support from Pfizer, author royalties from UpToDate and Springer, and has consulted for Inflazome unrelated to this work.
Ethical approval
This research was conducted using the UK Biobank resource (Project ID 45987). The project was approved by the UK Biobank on the 18th of April 2009. UK Biobank itself has approval from the North West Multi-Centre Research Ethics Committee (REC reference 16/NW/0274). This study did not involve recontacting participants and no separate research ethics committee approval was required, apart from approval by the UK Biobank.
Patient and public involvement
Patients or public were not involved in the design, report, or dissemination of our research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sandoval-Plata, G., Morgan, K. & Abhishek, A. Are polymorphisms affecting serum urate, renal urate handling and alcohol intake associated with co-morbidities in gout cases? A case–control study using data from the UK Biobank. Rheumatol Int 42, 1617–1622 (2022). https://doi.org/10.1007/s00296-022-05148-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05148-7