Abstract
As a result of the pandemic, many patients with an inflammatory rheumatic disease (IRD) have isolated themselves. The lack of disease management together with fear of infection could lead to changes in physical- and mental health. The aim of this study was to evaluate the social- and health behaviour in patients with an IRD compared with the behaviour of healthy individuals during the COVID-19 pandemic. The study was a questionnaire survey answered by patients with an IRD and healthy individuals (HI). The questionnaire contained seven sections with questions regarding COVID-19 and quality of life including SF-36, EQ-5D-5L, and visual analogue scale (VAS) pain, fatigue and global health. Of 1663 invited participants, 661 patients with IRD and 266 HI were included in the analyses. Patients with an IRD felt more isolated during the COVID-19 pandemic compared with HI (IRD: 9.5% (61/644), HI: 3.1% (8/259), p-value = 0.001). More HI (5.4%) had been infected with COVID-19 than patients with an IRD (1.7%). Among patients with an IRD those with worse self-reported disease activity outcomes (VAS pain, fatigue and global health, all p-value < 0.001), worse social functioning and emotional well-being were more isolated than individuals with low disease activity. Patients with an IRD feel more isolated during the COVID-19 pandemic compared to HI. Isolation seems to be most pronounced in patients with worse disease related patient-reported outcomes and lower quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the Coronavirus disease 2019 (COVID-19) pandemic, there has been great focus on protecting individuals in high-risk groups, including patients with an inflammatory rheumatic disease (IRD) [1]. Patients with an IRD are often at high risk of infection, due to treatment with immunosuppressive drugs, immune dysregulation and comorbidities [2, 3]. Previous studies from Denmark [1, 4] showed that patients with IRD have higher risk of hospitalisation with COVID-19 infection than the general population and that patients with rheumatoid arthritis may be at higher risk of a severe course of illness with COVID-19 than the general population. However, the study by Cordtz et al. showed that treatment with immunosuppressive medication does not force a greater risk [1].
As a result of the pandemic, many patients with an IRD have isolated themselves, making the disease management more difficult [5]. A study by Glintborg et al. investigated self-protection strategies and health behaviour in Danish patients with an IRD and found widespread anxiety and self-isolation among patients with an IRD [5]. The interplay between self-isolation, complex disease management and fear of infection could lead to changes in both physical- and mental health [6]. The aim of this study was to evaluate the difference in self-isolation during the COVID-19 pandemic between patients with an IRD and healthy individuals (HI). Furthermore, the impact of the COVID-19 pandemic on mental health and social functioning in patients with an IRD compared with HI were investigated.
Methods
Study design and participants
The study was designed as a questionnaire survey including patients with an IRD from the Department of Rheumatology, Aalborg University Hospital, and HI. The HI did not have an inflammatory rheumatic disease or any other severe chronic disease; however, individuals with osteoarthritis were eligible. An invite to the questionnaire survey was sent out by letter to patients with an IRD through the patients’ individual electronic mailbox (eBoks) on March 18, 2021, and could be answered until May 1, 2021. The letter contained a link to access the questionnaire in Research Electronic Data Capture (REDCap). Between March 17, 2021 and May 1, 2021 HI were enrolled from a Facebook post from Aalborg University Hospital with information about the trial and a link to access the questionnaire REDCap. The survey was conducted according to Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [7]. All participants accessed the closed survey in REDCap where data were stored in a dedicated electronic case report form (e-CRF) only accessible to research personnel conducting the study in the REDCap system hosted by the North Denmark Region [8, 9]. The participants were informed about the length of time of the survey, which data were stored and where and for how long, who the investigator was, and the purpose of the study. The survey was voluntary and no incentives were offered. The participants were asked to state if they wanted to participate (yes/no). Patients answering “yes” continued the survey. The respondents were able to review and change their answers during the survey before submission. To avoid multiple responses by same participant the civil registration number (Danish Civil Registration System) was required.
The usability and technical functionality of the electronic questionnaire had been tested by all the investigators before fielding the questionnaire. Furthermore, 25 research and health personal and two patients answered the survey and the survey was revised once according to the identified queries.
The questionnaire survey
The questionnaire survey had the following sections: (1) Questionnaire about COVID-19, (2) Participant characteristics, (3) Social and health behaviour during the COVID-19 pandemic, (4) Visual analogue scale (VAS pain, fatigue and global health), (5) Short Form 36 (SF-36), (6) European Quality of life—5 dimension—5 levels (EQ-5D-5L) and (7) Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F). Additionally, patients with an IRD were given some further questions regarding their specific disease and treatment. The questionnaire about COVID-19, and behaviour during the COVID-19 pandemic, has previously been used in studies of COVID-19 in patients with IRD [5] yet not validated. These questions were all statements with tick box categories with general attitude measurement and easy to complete. Adaptive questioning (items only conditionally displayed based on previous responses) was used to reduce number and complexity of the questions. VAS pain, fatigue and global health, SF-36, EQ-5D-5L and FACIT-F have all been validated in previous studies [10,11,12,13,14,15,16,17]. All survey answers were collected and saved in REDCap.
Statistics
Participant characteristics were reported as numbers and percentages for categorical variables. Continuous variables were tested for distribution. To assess if any continuous data were normally distributed, Shapiro–Wilk test for normality was used and histograms were investigated. Data were not normally distributed and hence reported by median and interquartile range (IQR).
Between group differences were analysed using Wilcoxon Mann–Whitney U test if data were continuous variables. For binary data, Chi-square test or Fisher's exact test was used to assess between-group differences.
The null hypotheses were that there is no difference between patients with IRD and HI. In the subgroup analyses for patients with IRD stratified by degree of isolation the null hypotheses were that there is no difference between the groups. When using Chi-square and Fisher’s exact test the null hypothesis is rejected with a p-value lower than 0.05. When the p-value is above 0.05, the null hypothesis is accepted.
Subgroup analyses were performed using Wilcoxon Mann–Whitney U test for patients with IRD stratified by degree of isolation. Additional analyses comparing patients with IRD > 50 years with HI > 50 years was performed. To compare the IRD with similar age group of HI, a sensitivity analysis was performed for < 50 and ≥ 50 years separately.
Protocol violations were pre-defined in the statistical analysis plan (SAP) to ensure validity and reliability. Participants who agreed to participate in the questionnaire by clicking “yes” to enrolment but did not answer any further questions within the questionnaire were excluded. Participants who agreed to participate in the questionnaire by clicking “yes” to enrolment but only completed parts of the questionnaire were considered as having a minor violation. The patients were excluded from analyses of incomplete answered sections. That is, if a patient failed to complete “Results”) but finished all other questionnaire sections, the answers were excluded from analyses involving “Results”) but included in all other analyses. Figure 1 contains a flowchart diagram of included participants. All applicable tests were two-sided and performed with a 5% significance level, p < 0.05. All data were analysed in the statistical software package IBM SPSS Statistics, V. 27.0.
Results
Participant characteristics
Table 1 shows the characteristics of the included participants. A total of 1663 participants answered the questionnaire; among these 927 participants were eligible for inclusion as illustrated in Fig. 1. In total, 661 patients with IRD and 266 HI were included. Most participants were females (IRD: 447 (67.2%), HI: 226 (85.0%)). Hypertension was the most frequent comorbidity in patients with IRD (235 (35.6%)).
The HI were younger (median: 38.0) than patients with IRD (median: 62.5). Most reported diagnosis was rheumatoid arthritis (50.7%), and conventional synthetic disease-modifying anti-rheumatic drugs (csDMARD) were the most applied type of medication (65.7%).
Influence of COVID-19 on social- and health behaviour
Patients with an IRD felt more isolated (p = 0.001) compared to HI, whereas more HI felt life went on with smaller changes (p = 0.55), Table 2. Although the difference between groups were less pronounced when comparing patients and HI > 50 years of age, patients with IRD still felt more isolated (p = 0.05).
Patients with an IRD were extremely worried about being infected with COVID-19 (p < 0.001). HI were more likely to be tested for COVID-19 than patients with an IRD (p = 0.01).
Pain, functioning and quality of life
Patients with an IRD reported higher Visual Analogue Scale (VAS) score for pain, fatigue and global health than HI (all p < 0.001). In all questions asked regarding SF-36, patients with an IRD reported a lower score than HI. Similarly, the EQ-VAS score showed a lower self-rated health among patients with an IRD compared with HI (p < 0.001). The FACIT-Fatigue score showed that patients with an IRD had more fatigue than HI (p < 0.001) (Table 2).
Furthermore, when comparing patients with an IRD who felt isolated during COVID-19 and patients with an IRD who did not feel isolated, a higher score of VAS pain, fatigue and global health was reported (all p < 0.001). Similarly, patients with an IRD who felt isolated also reported lower scores in all questions regarding SF-36 (all p < 0.001), EQ-VAS (p = 0.01) and FACIT-Fatigue (p < 0.001) (Table 3).
The impact of COVID-19 on the disease management in patients with inflammatory rheumatic disease
One hundred and eighteen patients with IRD (28.0%) had dose alterations of their immunosuppressive medication during the COVID-19 pandemic. Most of these patients were recommended the change by the Department of Rheumatology; however, 9.3% changed their medication because of fear of COVID-19.
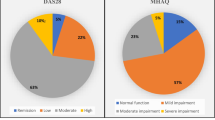
Only 10.7% postponed an outpatient visit for rheumatic disease during the past year as a consequence of COVID-19 and 9.2% actively rejected health-offers. Most patients had an acceptable symptom state (PASS “Yes”, 76.6%) (Table 4).
Discussion
This study represents a large questionnaire survey of patients with an IRD compared with HI investigating the impact of COVID-19 on social- and health behaviour and quality of life. This study demonstrated significantly more isolation in patients with an IRD than HI. While the difference between groups were less pronounced when comparing IRD patients and HI > 50 years of age, patients with IRD > 50 years of age still felt more isolated. Furthermore, isolation seems to be most pronounced in patients with worse disease-related patient-reported outcomes and lower quality of life.
A previous study investigating changes in behaviour, anxiety and self-isolation among patients with an IRD found high levels of anxiety and self-protection [5]. However, the patients were not compared to HI. In the present study the results demonstrated significantly more isolation in patients with an IRD than HI. A possible explanation for the observed difference between patients and HI could be that patients with an IRD are at greater risk of any infection and, therefore, self-isolate to a higher degree [9]. The observed self-isolation could be a possible explanation for the significantly lesser number of patients with an IRD tested for COVID-19 than HI. Moreover, significantly fewer patients with an IRD had been tested positive for COVID-19. Some of the patients with an IRD had one or multiple comorbidities, which could have affected their need of isolation. Therefore, it is not clear whether the comorbidities of the patients with an IRD had an influence on their need to isolate.
This study showed that patients with an IRD were more afraid of being infected with COVID-19 than HI. This result is in agreement with findings of a previous study, where a high degree of fear of COVID-19 was reported by patients with an IRD during the first wave [5]. Thus, it seems that the fear of COVID-19 among patients with an IRD persists, i.e. is nearly the same a year after the start of the pandemic.
Patients with an IRD who felt isolated during COVID-19 pandemic reported worse VAS pain, fatigue and global health compared with patients with an IRD who did not feel isolated. This could indicate more isolation among patients with higher self-reported disease activity. However, patients with an IRD feeling isolated had a worse social functioning, emotional well-being and, therefore, it is not clear whether the patients isolated because of disease activity, affected mental health or both. Furthermore, disease activity and mental health could be interrelated. Our findings concerning social functioning and mental health correlate with results by Cleaton et al. [6], where isolated patients with an IRD had worse mental health than non-isolating patients with an IRD. Furthermore, the present study found that patients with an IRD had worse social functioning compared with HI measured by SF-36. Patients with an IRD also reported a lower emotional wellbeing (sub score in SF-36) compared with HI.
This study revealed that 9.3% of 118 patients with an IRD had a dose alteration due to the fear of the COVID-19 pandemic. Nevertheless, the majority of the patients did not change their medication due to the pandemic.
One out of ten patients with an IRD had postponed an outpatient visit for rheumatic disease during the past year. A study by Michaud et al. [18], found that 20.8% of the rheumatic patients in the United States of America either cancelled or postponed their appointments. The difference in postponements/cancellations could, however, be explained by the difference in health care systems in Denmark versus US. However, this could also be explained by the difference in death numbers caused by COVID-19 in these countries and indicate that patients with an IRD in Denmark do not have the same impact on disease care because of COVID-19 as in the United States of America.
The study does have important limitations. Data were based on a questionnaire and patient-reported outcomes. All the information was provided by the participants including diagnosis and medication and was not verified. However, only patients with a rheumatic diagnosis and an active course in the department of rheumatology were asked to participate. A larger population could also have improved the study.
The difference in age between patients with IRD and HI is another limitation. Since age is an important factor in COVID-19 infection, analysis for patients and HI > 50 years was performed separately. Another limitation was the contact method to the patients. With a single mail through e-Boks the questionnaire was sent to those patients registered at the Department of Rheumatology at Aalborg University Hospital with a possible bias towards patients with more IT-knowledge, greater socioeconomic status and lower disease activity participating. Furthermore, recall bias regarding the initial phase in March 2020 cannot be excluded, because this questionnaire was sent out in the beginning of February 2021.
When conducting a survey-based study, no actual interviewer is present when participants are answering the questionnaire. Therefore, this prevents the investigators from gaining clarification on responses of open-ended questions where the predefined answering options may not be covering all possibilities within the questions. Furthermore, surveys conducted on the internet are also prone to erroneous reporting.
Conclusion
Taking the population size into consideration, this study could indicate that patients with an IRD feel more isolated during the COVID-19 pandemic compared with HI with fear of COVID-19 having the greatest impact on social and health behaviour. Furthermore, the study implies that patients with worse self-reported disease activity, worse social functioning and emotional well-being were more isolated. This preventive strategy is important to recognize when studying patients with IRD and outcome of COVID-19. Furthermore, in the daily clinic more attention is recommended to this vulnerable group.
Data availability
The authors commit to share relevant anonymised data as well as the SAP on reasonable request.
References
Cordtz R, Lindhardsen J, Soussi BG, Vela J, Uhrenholt L, Westermann R et al (2021) Incidence and severeness of COVID-19 hospitalization in patients with inflammatory rheumatic disease: a nationwide cohort study from Denmark. Rheumatology (Oxford) 60:59–67
Listing J, Gerhold K, Zink A (2013) The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology (Oxford) 52:53–61
Falagas ME, Manta KG, Betsi GI, Pappas G (2007) Infection-related morbidity and mortality in patients with connective tissue diseases: a systematic review. Clin Rheumatol 26:663–670
Cordtz R, Kristensen S, Dalgaard LP, Westermann R, Duch K, Lindhardsen J et al (2021) Incidence of COVID-19 hospitalisation in patients with systemic lupus erythematosus: a nationwide cohort study from Denmark. J Clin Med 10:3842
Glintborg B, Jensen DV, Engel S, Terslev L, Pfeiffer Jensen M, Hendricks O et al (2021) Self-protection strategies and health behaviour in patients with inflammatory rheumatic diseases during the COVID-19 pandemic: results and predictors in more than 12,000 patients with inflammatory rheumatic diseases followed in the Danish DANBIO registry. RMD Open 7:e001505
Cleaton N, Raizada S, Barkham N, Venkatachalam S, Sheeran TP, Adizie T et al (2021) The impact of COVID-19 on rheumatology patients in a large UK centre using an innovative data collection technique: prevalence and effect of social shielding. Rheumatol Int 41:707–714
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 6:e34
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Chandran V, Bhella S, Schentag C, Gladman DD (2007) Functional assessment of chronic illness therapy-fatigue scale is valid in patients with psoriatic arthritis. Ann Rheum Dis 66:936–939
Cella D, Yount S, Sorensen M, Chartash E, Sengupta N, Grober J (2005) Validation of the Functional Assessment of Chronic Illness Therapy Fatigue Scale relative to other instrumentation in patients with rheumatoid arthritis. J Rheumatol 32:811–819
Hurst NP, Kind P, Ruta D, Hunter M, Stubbings A (1997) Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol 36:551–559
Tsang HHL, Cheung JPY, Wong CKH, Cheung PWH, Lau CS, Chung HY (2019) Psychometric validation of the EuroQoL 5-dimension (EQ-5D) questionnaire in patients with spondyloarthritis. Arthritis Res Ther 21:41
Van Tubergen A, Black PM, Coteur G (2015) Are patient-reported outcome instruments for ankylosing spondylitis fit for purpose for the axial spondyloarthritis patient? A qualitative and psychometric analysis. Rheumatology 5:1842–1851
Husted J, Gladman D, Farewell V, Long J, Cook R (1997) Validating the SF-36 health survey questionnaire in patients with psoriatic arthritis. J Rheumatol 24:511–517
Linde L, Sørensen J, Østergaard M, Hørslev-Petersen K, Hetland ML (2008) Health-related quality of life: validity reliability, and responsiveness of SF-36, EQ-15D, EQ-5D, RAQoL, and HAQ in patients with rheumatoid arthritis. J Rheumatol 35:1528–1537
Cauli A, Gladman DD, Mathieu A, Olivieri I, Porru G, Tak PP et al (2011) Patient global assessment in psoriatic arthritis: a multicenter GRAPPA and OMERACT study. J Rheumatol 38:898–903
Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR et al (2020) Experiences of patients with rheumatic diseases in the United States during early days of the COVID-19 pandemic. ACR Open Rheumatol 2:335–343
Funding
This research was conducted without any funding.
Author information
Authors and Affiliations
Contributions
The research hypothesis and study conception were developed by TEE, WKHD, LU and SK. TEE, WKHD, LU, SK and KD contributed to data collection and data management. TEE, WKHD, SK and LU wrote the SAP with input from all authors and conducted the statistical analyses. LU, SK and KD have verified the underlying data. TEE and WKHD wrote the first draft of the manuscript under supervision from SK, LU, LD, and KD; thereafter, revised the manuscript after input from all authors. All authors had full access to all the study data, contributed with interpretation of data and approved the final submitted manuscript. Authors take full responsibility for all aspects of the presented work.
Corresponding author
Ethics declarations
Conflict of interest
LD: Grants (BMS), Speakers bureau (Galderma, Eli Lilly, Janssen). TEE, WKHD, LU, KD, and SK: None declared.
Ethics approval
The study was registered in the North Denmark Region internal list of research projects (2020-182) but did not require approval by the regional Ethics Committee. The trial was conducted in compliance with the protocol and the Declaration of Helsinki. Written informed consent was obtained from all patients before enrolment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eriksen, T.E., Dinesen, W.K.H., Uhrenholt, L. et al. Isolation in patients with inflammatory rheumatic diseases during COVID-19 pandemic compared to healthy individuals: a questionnaire survey. Rheumatol Int 42, 783–790 (2022). https://doi.org/10.1007/s00296-022-05111-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05111-6