Abstract
The objective is to describe the spectrum of the health professional (HP) treatment approach for systemic sclerosis (SSc) from the perspective of Dutch HPs, including alignment of treatment goals set by HPs with self-reported referral reasons, coverage of patient-reported unmet care needs, and quality of communication between HPs and rheumatologists. Dutch HPs were invited through their patients with SSc to complete an anonymous online survey. The survey covered referral reasons, treatment goals, and interventions of the last patient treated, as well as the perceived quality of communication between HPs and rheumatologists. Referral reasons and treatment targets were linked to the International Classification of Functioning, Disability and Health following the refined ICF Linking Rules. Seventy-nine HPs from 8 professions (including 58 physiotherapists, 73%) completed the survey. One hundred and thirty-three different referral reasons were reported, yielding 58 different ICF codes, with 41 (70.7%) being linked to the ICF domain “body structures and functions.” The reported interventions focused on body functions/structures (27.9%), training of daily activities (25.6%), education and advice (26.3%), and psychosocial interventions (20.2%). The quality of communication between HPs and rheumatologists was perceived as low. Our findings revealed numerous treatment options offered by Dutch HPs addressing the unmet care needs of patients with SSc. There is an overlap in the content of the various HP disciplines, and HP treatment goals are not sufficiently aligned with referrals of rheumatologists. HP treatment offer seemed inefficiently organized, possibly precluding rheumatologists from making targeted referrals. Communication between rheumatologists and HPs should be improved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Systemic sclerosis (SSc) is a rare and complex autoimmune disease with large differences in severity and extent. Its worldwide incidence is an estimated 13 people per million per year, and its prevalence is approximately 200 people per million [1]. SSc has a heterogeneous and often progressive nature that involves skin, vessels, joints, and internal organs, and it significantly impairs patients’ daily functioning and quality of life [2, 3]. There is no effective treatment or cure for SSc yet, meaning that treatment is primarily aimed at controlling symptoms and maintaining quality of life [4]. As treatment options for life-threatening, organ-based complications improve, treatment approaches for nonfatal SSc complications require increased attention [5,6,7].
Due to the direct impact of SSc on daily functioning and psychosocial well-being of patients, non-pharmacological management and treatments are a key element of SSc care [8]. Health professionals in rheumatology (HPs), including occupational therapists, physiotherapists, psychologists, and social workers, play a vital role in the support of individuals with SSc manage their nonfatal SSc complications [9]. So far, no recommendations for the non-pharmacological care for SSc are formulated, but several high-quality randomized trials support the use of non-pharmacological treatment options to reduce the clinical burden of a variety of symptoms [6, 10, 11]. In addition, care by health professionals is also based on treatments proven to be effective in other rheumatic diseases. For instance, promising approaches to address fatigue in patients with RA and SLE are also applicable for patients with SSc [12,13,14].
In the past decades, owing to changes in the Dutch health care system, HP treatment has been transferred from hospital-based team care to a primary care setting. As a result, patients with SSc have more often been referred to HPs working in monodisciplinary primary care settings. Considering that, rheumatologists have more confidence in HP colleagues with whom they work on a daily basis in the same institution [15]. This development may have negatively affected rheumatologists’ knowledge of HP treatment options, adequate coordination of treatment, and the quality of communication between rheumatologists and HPs.
SSc patients consider non-pharmacological care as one of the five main issues affecting the quality of SSc care in need of improvement [9, 16, 17]. Spierings et al. identified the following the top five unmet care needs of patients with SSc: fatigue, Raynaud’s phenomenon, physical limitations, and impaired hand and joint function [17]. It remains unknown to what extent these five unmet care needs are addressed by HPs in the treatment of patients with SSc.
Therefore, the aim of our study was to examine the content and alignment of care delivered by Dutch HPs with patients’ most important needs.
Methods
Design
A cross-sectional study using a web-based survey (SurveyMonkey®.com) was conducted to make an inventory of perceptions of Dutch HP treating patients with SSc. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and using the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [18, 19].
Survey
The survey questions were based on several preliminary investigations conducted by the Arthritis Research and Collaboration Hub (ARCH) working group: a literature review, three semi-structured multicenter focus group interviews, and individual interviews among patients, HPs, and rheumatologists [17].
The 23 survey questions were distributed over 14 webpages and divided into 4 domains: socio-demographic and work setting-related characteristics (12), referral to non-pharmacological care (2), treatment (5), and perceived quality of communication (4). The survey included both open-ended questions, asking the participants to answer in their own words, and closed questions, providing multiple-choice and multiple-response questions.
Socio-demographic and work setting-related questions
The survey started with 12 socio-demographic and work setting-related questions: sex (woman, man); age (free text); educational level (bachelor, master, Ph.D., and others); work experience (free text); profession (dietitian, occupational therapist, physiotherapist, hand therapist, speech therapists, social worker, dental hygienist, exercise therapist, podiatrist, psychologist, and others); caseload of SSc patients in the past year (0–2, 3–6, 7 or more); SSc specialization (yes/no); working hours per week (32 or more, 20–31, 12–19, others); work domains of the past 5 years (patient care, research, education, management, and others); current work setting (academic hospital, regional hospital, health center, private practice, nursing home, rehabilitation center, and others); SSc specialization of work setting (yes, no); and participation in multidisciplinary SSc consultations (yes, no, and others).
Referral to non-pharmacological care
Types of referrer were assessed by means of a list of seven medical disciplines and an option to add new items. With the following answering format: never, sometimes, and always. Most common reasons for SSc referrals, as reported by HPs, were assessed by an open-ended question with three options for free text responses.
Treatment
Five questions assessed the HP treatments. HPs were asked to consider the last SSc patient treated to assess the following items: type of SSc (limited SSc, diffuse SSc, I do not know, others), main treatment goals (open-ended question with 3 options for free text responses), main interventions (multiresponse question divided into 4 domains, body structure and functions (20 items), activity and participation (9 items), education and advice (20 items), and psychosocial interventions (12 items). These multiresponse questions were used to prioritize items, participants could choose a maximum of three options, including an option to add a new item. Duration of HP treatment was assessed with two free text questions: duration in weeks and number of treatment contacts.
Perceived quality of communication
Perceived quality of communication was assessed by adapting four items of the Dutch version of the Consumer Quality Index Rheumatoid Arthritis (CQI-RA) (version 2.0), subscale ‘Communication’. The CQI-RA was found to be a reliable measure for patients’ experiences with the quality of rheumatic care [20]. For our study, we used the items ‘Parallel treatments were adjusted to one another’, ‘Various advises were integrated’, ‘Caregivers kept their appointments’ and ‘Caregivers were aware of other activities of caregivers’ and adapted them to measure the experiences of HP (see Table 4). The answering format of the items was: never, sometimes, usually, and always.
The survey was evaluated by members of the ARCH SSc working group and a patient panel of five patients. Only an individual code and Internet Protocol (IP) address was registered to guarantee the anonymity of the participants. Pilot testing of the questionnaire was undertaken in five HPs to ensure the relevance of the questions [17].
Sampling strategy
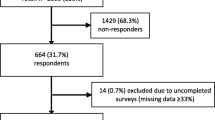
Sampling followed a targeted snowball sampling strategy [21]. Dutch HPs from different disciplines (including physiotherapists, occupational therapists, podiatrists, hand therapists, dietitians, dental hygienists, speech therapists, psychologists, and social workers) were eligible to participate in the study, if they were currently treating or had previously treated patients with SSc. There were no participation restrictions on the workplace, the case load, or the working environment. HPs were invited by their own patients with SSc who participated in a large-scale survey among 650 Dutch patients with SSc set up by the ARCH working group. Patients with SSc who participated in the study were asked to ‘snowball’ their treating HPs by providing them with an internet link we offered, or by writing down the name and address of the workplace of the HP, enabling us to invite the HP to take part in the study. An estimation of the sample size was not possible due to snowballing as sampling strategy and the unknown number of HPs working with SSc patients in the Netherlands. Eligible participants had 4 months to voluntarily complete the survey (December 2017 to March 2018). The survey link was open from the time the participants were first informed about the study. The cover letter, displayed on the first page of the survey, provided details about the background and purpose of the survey, along with the estimated duration of the survey (15 min). Informed consent was taken at the beginning of the survey.
Data handling and confidentiality
IP address checks have been performed to avoid duplicate answers from one respondent. The data processing was completely anonymous, with the IP addresses remaining with the first and corresponding author. A second author (CHME) had access to the individual codes and synthesized data without associated IDs. Only completed surveys were included in the analyses.
Ethical approval was obtained from the Institutional Review Board of the Radboudumc Nijmegen, the Netherlands, protocol (2017: 3621).
Data analysis
Statistical analysis
Socio-demographic and work setting-related data, HP interventions and perceived quality of communication were analyzed descriptively. Continuous variables, following a normal distribution, were reported as means and SD and categorical variables as absolute numbers and percentages. Statistical analyses were conducted using Stata/IC 13.1 (StataCorp LP, College Station, TX).
Analysis of open-ended questions
The qualitative data analysis of the answers to open-ended questions followed an adapted form of “meaning condensation” [22]. First, all answers to the open questions about referral reasons and treatment goals were read through by the principal investigator (JS) to obtain an overview of the collected data. Second, all data were divided in ‘meaning units’, defined as specific text units, either a few words or a part of a sentence with a common meaning. Third, concepts within each meaning unit were identified. Sometimes one meaning unit could contain several concepts. For instance, the meaning unit, “Staying fit so that my client can keep walking > 5 km.” contains the concepts ‘maintaining physical fitness’ and ‘walking longer distances’. All resulting concepts were linked to the most appropriate ICF category according to established linking rules [23, 24]. The purpose of the matching process was to translate the concepts from the HPs’ answers into the most appropriate ICF categories. The ICF classification uses a hierarchical structure organized in chapters, or ‘first level’ categories, which subdivide the four separate concepts of body functions, Body structures, activities and participation and environmental factors. Each chapter contains numerous categories (second, third, and fourth levels), which form the classification unit. The specificity increases from the first to the fourth level. As an example, the concept ‘walking longer distances’ was linked to d450 Walking. ‘Maintaining physical fitness’ was linked to d5701 Managing diet and fitness.
In accordance with the linking rules, interactive discussions were held to resolve coding discrepancies (JS and CHME). Finally, all assigned ICF codes were re-read repeatedly by the main coder (JS) to ensure that the linked ICF codes reflected the meaningfulness of the concept.
Through this process, the large number of answers to the open questions on referral reasons and treatment goals were reduced to a smaller amount of clearly defined ICF terms. These were used to compare treatment goals with reasons for referral and unmet care needs.
Results
Participants, origin, and content of referrals
We obtained 81 completed surveys. One duplicate response set was identified and excluded from the analysis, and another set was excluded for not meeting the inclusion criteria; the person was a medical doctor. Thus, data from 79 surveys taken by eight HP professions were analyzed. Table 1 presents the HPs’ socio-demographic and work-related characteristics.
The larger proportion of participants was female (n = 52; 67%). Physiotherapists were the largest group represented (n = 58; 73%), followed by dietitians (n = 6; 8%) and occupational therapists (n = 5; 6%). Nineteen (24%) of the respondents reported to have treated 3 or more patients with SSc in the past year. Most HPs (n = 60, 69%) worked in private practices. In all, 21 (26.6%) HPs felt specialized in SSc care, and 11 (13.9%) found that their workplace was specialized in SSc. Only six HPs (5.6%) regularly participated in multidisciplinary SSc meetings.
HPs reported that rheumatologists were the most frequent referrers (n = 56, 73.7%). Nearly one-third (n = 22, 29.0%) of the reported referrals were patient self-referrals. All other referrals were distributed among general practitioners (n = 14, 18.4%), dermatologists (n = 4, 5.3%), other medical specialists (n = 14, 18.5%) and other HPs (n = 4, 5.3%).
The 129 concepts on referral reasons, collected from open-ended questions, could be linked to 47 unique ICF codes and included 31 ICF codes on Body structures and functions (89 concepts), 13 on Activities and participation (36 concepts), and 3 on Environmental factors (4 concepts). Table 2 presents the ten most frequently mentioned referral reasons together with the reporting disciplines. Seven of the ten most frequently cited referral reasons were aimed at Body structures and functions. In addition, up to four HP disciplines received referrals with identical referral reasons.
Treatment goals and interventions
Analysis of the reported treatment goals revealed 209 concepts that could be coded into 66 unique ICF codes. Most of the treatment goals were aimed at Body structures and functions (n = 35 ICF codes, consisting of 119 concepts), a smaller part focused on Activities and participation (n = 27 ICF codes, consisting of 86 concepts) and only a small amount of the treatment goals aimed at Environmental factors (n = 4 ICF codes, consisting of four concepts). Nine participants did not report any treatment goals. Table 3 shows the ten most frequently mentioned treatment goals, together with the number of disciplines that reported the respective treatment goal.
A total of 605 interventions (8.8 average per participant) were reported, with the treatment focus more or less evenly distributed across the following 4 components: Bodily functions/structures (27.9%), Training of activities (25.6%), Education/advice/instruction (26.3%), and Psychosocial interventions (20.2%). The most frequently mentioned interventions (top four per topic) are presented in Table 4. Within these most frequently mentioned interventions, we found five interventions or strategies that are applied by up to six different HP disciplines: walking/cycling (4), exercise activities/sport (6), household (5), self-management/self-monitoring (4), and motivational interviewing (5) (Table 4).
Alignment of referral reasons and HP treatment goals
In all, 17 of 129 (13.2%) referral reason concepts matched with one of the treatment goal concepts at the patient level. In 10 cases, referral reasons fully matched with treatment goals. The ICF codes d230/2303 (Carrying out daily routine/Managing one’s own activity level) corresponded in four cases, whereas b4551 (Aerobic capacity), and b280 (Sensation of pain) corresponded in two cases. The other corresponding codes were: b4550/b4551 (General physical endurance/Aerobic capacity), b710/b7101 (Mobility of joint functions/Mobility of several joints), b730 (Muscle power functions), d445 (Hand and arm use), s320/s3200 (Structure of mouth/Teeth), and s7502 (Structure of ankle and foot).
Correspondence between treatment goals and unmet care needs
The examined unmet care needs fatigue, Raynaud’s phenomenon, joint problems, physical function, and hand function were covered by 108 out of the total of 209 ICF codes extracted from reported HP treatment goals. Since the unmet care needs described relate to physical symptoms and not to the transcending health information such as situations and daily activities, almost exclusively ICF codes from chapters b (Body functions) and s (Body structures) could be assigned.
In 57 (81.4%) of the 70 cases in which participants provided information about treatment goals, we found ICF codes directly associated with 1 or more of the 5 unmet care needs. In half of all cases, we found agreement with the unmet care need fatigue (n = 16, 22.9%), Raynaud’s phenomenon (n = 12, 17.1%), joint problems (n = 18, 25.7%), physical function (n = 35, 50.0%), and hand function with nine associable cases (12.9%). In 13 cases, we did not find a direct connection with 1 of the 5 unmet care needs; 7 of them concerned the participating dieticians and the 1 of them the only participating oral hygienist.
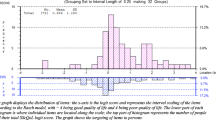
Quality of communication between HP and rheumatologists
Figure 1 illustrates the percentage of participants’ perceptions on the quality of communication. Nearly one-third (29%) of those questioned could not make any statements about the cooperation and/or the quality of communication. Overall, slightly above 40% of the participants had a positive view about the quality of communication. One-quarter of the HPs reported that they are mostly satisfied with the agreements they have with the rheumatologists. Almost 40% of HPs rarely or never inform the rheumatologist about the goals, progress, and outcomes of their treatment.
Discussion
This cross-sectional survey study revealed that HPs use a broad spectrum of treatment goals (unique ICF codes, n = 66) and interventions (n = 51). At the HP group level, the ten most common referral reasons and treatment goals were considerably similar. However, analysis at an individual level indicated discrepancies between the self-reported referral reasons provided by the HPs and the reported treatment goals, suggesting insufficient alignment between referral reasons and treatment goals. On the other hand, we demonstrated that HP treatment goals indeed match the most important unmet care needs of SSc patients reported in the literature. Another critical finding was that relatively few HPs communicated with the rheumatologists and only some HPs reported to have agreements with rheumatologists, implying a poor quality of communication between HPs and rheumatologists.
Missing coherence between referral reasons and HP approach
We found discrepancies between rheumatologists’ referral reasons and the reported HP treatment goals and interventions. HPs report interventions that are not mentioned in the referral reasons such as education, psychosocial interventions, and interventions aimed at social or environmental factors. A possible explanation for this may be insufficiently targeted referrals by rheumatologists. One study among Dutch rheumatologists specialized in SSc, the rheumatologists indicated to be insufficiently aware of the non-pharmacological treatment options [15]. In the absence of available evidence-based guidelines, practice-based evidence recommendations based on consensus could be a good option to share information about existing HP treatment options with referrers and patients. In addition, practice-based or consensus-based non-pharmacological recommendations could also be a good adjunct to the next update of the European League Against Rheumatism (EULAR) recommendations for the treatment of SSc of Kowal-Bielecka et al. [25].
Good correspondence between treatment goals and unmet care needs and SSc-ICF core set
Our results establish that the reported treatment goals covered the five most important unmet care needs of patients with SSc: fatigue, Raynaud’s phenomenon, joint problems, physical function, and hand function described by Spierings et al. (2019). Our findings complement those of a European study by Willems et al. [26] on the content of HP SSc care identifying fatigue, Raynaud’s phenomenon, and hand function as the most important treatment goals. These results suggest that HPs are indeed able to identify the care needs of patients with SSc. Despite these promising results, written consensus- and evidence-based recommendations need to be established to make the possibilities of HP care more visible for patients with SSc and rheumatologists.
Large overlap in interventions
Our results reveal that in some cases up to six disciplines indicate that they focus on the same areas of intervention. Due to the quantitative nature of our study, it is unclear whether they actually offer the same interventions or whether they are working with a different focus and intervention strategy. This overlap of the intervention offer could make it difficult for referrers to refer patients with SSc targeted to the best matching HP discipline because the spectrum of interventions offered is large but without clear distinctions. Studies with a qualitative approach could help to further specify the content of the interventions offered and allow referrers to make more targeted referrals to the most appropriate HP disciplines [27].
Quality communication between HPs and rheumatologists
Our results suggest a suboptimal communication of the HPs with the rheumatologists. Due to transitions of the health care system in the Netherlands, the work setting of HPs delivering care for patients with rheumatic diseases moved from larger hospitals to primary care setting. As a result, possibilities for specialization and multidisciplinary collaboration for HPs in the Netherlands have thinned, thereby reducing direct interaction of HPs with their medical and other HP colleagues. Due to the broad alignment with different target groups in primary care, there is a decrease in specialized HPs for the treatment of rare disorders. This new situation requires new models of care because the complex situation of people with SSc requires specialized care. A digital network, such as ParkinsonNet [28], could be a possible component of such a new care model. ParkinsonNet is a network of more than 3400 specialized health care providers with national coverage in the Netherlands. The model of ParkinsonNet has also been adopted in other countries [29]. Such a network could connect patients and the various health care providers in a targeted manner and thereby increase communication, the quality of multidisciplinary collaboration, and thus the quality of SSc care.
This study had a number of limitations. One limitation was the rather low response rate. We expected that by approaching the HPs through the 650 SSc patients who had participated in the previous survey study, a larger number of HPs would be reached. A possible explanation for the relatively small number of participating HPs is that they, although invited by their patients, subsequently did not participate because they felt insufficiently specialized in SSc. This explanation is supported by the low number of HPs (around 25%) that reported to feel specialized in SSc treatments. The second limitation is the limited use of validated questionnaires, for instance to examine the heterogeneity of interventions. Another limitation might be that our results on referral reasons are based on self-report by HPs, which could lead to recall bias. A content analysis of referral letters would be an option to obtain more reliable information.
Conclusion
We found a broad spectrum of treatment options offered by Dutch HPs that address the unmet care needs of patients with SSc. An overlap in the content of the care delivered by the various HP disciplines was noted, and the referrals of rheumatologists were not sufficiently aligned with HP treatment goals. The HP offer seems to be inefficiently organized, which may prevent rheumatologists from making targeted referrals. Strategies for better communication between rheumatologists and HPs should be developed and implemented.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SSc:
-
Systemic sclerosis
- HPs:
-
Health professionals in rheumatology
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- ARCH:
-
Arthritis Research and Collaboration Hub
- ICF:
-
International Classification of Function and Disability
- EULAR:
-
European League Against Rheumatism
- CQI:
-
Consumer quality index
References
Barnes J, Mayes MD (2012) Epidemiology of systemic sclerosis: incidence, prevalence, survival, risk factors, malignancy, and environmental triggers. Curr Opin Rheumatol 24:165–170
Nakayama A, Tunnicliffe DJ, Thakkar V, Singh-Grewal D, O’Neill S, Craig JC et al (2016) Patients’ perspectives and experiences living with systemic sclerosis: a systematic review and thematic synthesis of qualitative studies. J Rheumatol 43:1363–1375
Papelard A, Daste C, Alami S, Sanchez K, Roren A, Segretin F, et al. (2019) Construction of an ICF core set and ICF-based questionnaire assessing activities and participation in patients with systemic sclerosis. Rheumatology
Almeida C, Almeida I, Vasconcelos C (2015) Quality of life in systemic sclerosis. Autoimmun Rev 14:1087–1096
Peytrignet S, Denton CP, Lunt M, Hesselstrand R, Mouthon L, Silman A et al (2017) Disability, fatigue, pain and their associates in early diffuse cutaneous systemic sclerosis: the European Scleroderma Observational Study. Rheumatology 57:370–381
Rannou F, Boutron I, Mouthon L, Sanchez K, Tiffreau V, Hachulla E et al (2017) Personalized physical therapy versus usual care for patients with systemic sclerosis: a randomized controlled trial. Arthritis Care Res 69:1050–1059
Frantz C, Avouac J, Distler O, Amrouche F, Godard D, Kennedy AT, et al. (2016) Impaired quality of life in systemic sclerosis and patient perception of the disease: a large international survey. 46:115-123
Spierings J (2020) Optimizing outcomes of patients with systemic sclerosis
Mouthon L, Alami S, Boisard A, Chaigne B, Hachulla E, Poiraudeau S (2017) Patients’ views and needs about systemic sclerosis and its management: a qualitative interview study. BMC Musculoskeletal Disorders 18:230
Schouffoer AA, Zirkzee EJ, Henquet SM, Caljouw MA, Steup-Beekman GM, van Laar JM et al (2011) Needs and preferences regarding health care delivery as perceived by patients with systemic sclerosis. Clin Rheumatol 30:815–824
Maddali-Bongi S, Del Rosso A (2016) Systemic sclerosis: rehabilitation as a tool to cope with disability. Burns 14:15
Pope JE (2020) Management of fatigue in rheumatoid arthritis. RMD Open 6:e001084
Shen B, Li Y, Du X, Chen H, Xu Y, Li H et al. (2020) Effects of cognitive behavioral therapy for patients with rheumatoid arthritis: a systematic review and meta-analysis. Psychol Health Med 1–13
del Pino-Sedeño T, Trujillo-Martín MM, Ruiz-Irastorza G, Cuellar-Pompa L, de Pascual-Medina AM, Serrano-Aguilar P et al (2016) Effectiveness of nonpharmacologic interventions for decreasing fatigue in adults with systemic lupus erythematosus: a systematic review. Arthritis Care Res 68:141–148
Stöcker JK, Cup EH, Vonk MC, van den Hoogen FHJ, der Sanden N-V, Maria WG, Staal JB et al (2018) What moves the rheumatologist? Unravelling decision making in the referral of systemic sclerosis patients to health professionals: a qualitative study. Rheumatol Adv Practice 2:rky027
Milette K, Thombs BD, Maiorino K, Nielson WR, Körner A, Peláez S (2018) Challenges and strategies for coping with scleroderma: implications for a scleroderma-specific self-management program. Disabil Rehabil:1–10
Spierings J, van den Ende C, Schriemer R, de Pundert L, Moens HB, van Laar J et al (2019) Optimal care for systemic sclerosis patients: recommendations from a patient-centered and multidisciplinary mixed-method study and working conference. Clin Rheumatol 38:1007–1015
Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 4:e297
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Int Res 6:e34
Zuidgeest M, Sixma H, Rademakers J (2009) Measuring patients’ experiences with rheumatic care: the consumer quality index rheumatoid arthritis. Rheumatol Int 30:159–167
Dusek GA, Yurova YV, Ruppel CP (2015) Using social media and targeted snowball sampling to survey a hard-to-reach population: a case study. Int J Doctoral Studies 10:279–299
InterViews KS (1996) An introduction to qualitative research interviewing
Cieza A, Brockow T, Ewert T, Amman E, Kollerits B, Chatterji S et al (2002) Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med 34:205–210
Cieza A, Fayed N, Bickenbach J, Prodinger B (2019) Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil 41:574–583
Kowal-Bielecka O, Fransen J, Avouac J, Becker M, Kulak A, Allanore Y et al (2017) Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis 76:1327–1339
Willems LM, Redmond AC, Stamm TA, Bostrom C, Decuman S, Kennedy AT et al (2015) Content of non-pharmacological care for systemic sclerosis and educational needs of European health professionals: a EUSHNet survey. Clin Exp Rheumatol 33:S153–S159
Johnson SR, O’Brien KK (2016) Qualitative methods in systemic sclerosis research. J Rheumatol 43:1265–1267
Nijkrake MJ, Keus SH, Overeem S, Oostendorp RA, Vlieland TPV, Mulleners W et al (2010) The ParkinsonNet concept: development, implementation and initial experience. Movement Disorders 25(7):823–829
Specker C, Richter J, Take A, Sangha O, Schneider M (1998) RheumaNet–a novel Internet-based rheumatology information network in Germany. Br J Rheumatol 37:1015–1019
Acknowledgements
The authors would like to thank C. W. Y. Appels, R. Bakker, S. Bazen, F. Bender, H. Berkers, A. E. van der Bijl, E. W. F. Blaas, F. Bonte-Mineur, H. Boerhof, G. W. M. Boerrigter, R. Bos, W. J. W. Bos, C. Bruggink, P. D. M. de Buck, E. van de Burgt, F. S. Catarinella, S. Denktaş, M. Derksen, T. Dhondai, M. Eimers, R. J. Goekoop, E. van Gorp, L. D. M. Gossens, A. Groenendaal-Boender, R. van der Heijden, M.J. Herenius, J. Hofman, J. Huizer, M. Hulsinga, B. Jilderda, R. Jonkers, S.J. de Jong, C.G.M. Kallenberg, M.A.E. de Kanter, M. van Klei, H. Knaapen-Hans, H. Knaken, I. Koopmans, P. Krop, L. Kwakkenbos, R. Langenhuijsen, S. Leroux, I. C. Lether, M. Limper, M. Lohr, L. van Mourik, D. J. Mulder, A. Muns, S. Otter, S Persijn, W. F. Peter, J. Potjewijd, B. Rave, H. de Ruiter, C. G. Schoemaker, T. H. M. Schoonbrood, A. A. Schouffoer, M. Soeters, A. J. Stel, J. Stöcker, Y. K. O. Teng, E. Ton, A. van Veen, S. Verhaar, P. M. J. Verhoeven, E. Voogt, M. Voortman, Y. de Vries, A. E. Voskuyl, and J. E. M. Wijbrans-Roodbergen for attending the working conference.
Funding
This study is supported by the Netherlands Organization for Scientific Research (NWO) Ph.D. program for teachers with project number 023.006.043. The funding organization played no role in the design of the study, collection, analysis, and interpretation of data, nor any role in writing the manuscript. The authors are grateful to the Dutch Society for Lupus, APS, Scleroderma, and MCTD for the collaboration. They acknowledge the Dutch Arthritis Foundation (ReumaNederland) for funding the ARCH initiative.
Author information
Authors and Affiliations
Consortia
Contributions
JS, FH, RNS, JBS, TS and CHME contributed to study design, interpretation of study data, and manuscript drafting. JS and CHME contributed to study design, discussion of coding discrepancies, interpretation of study data, and contributed to manuscript drafting. JS was involved in the recruitment of the participants. MV, SJ, CHME, and JS contributed to data analysis. All the authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no benefits from commercial sources, no other financial interests, and no conflicts of interest.
Ethics approval
Ethical approval was obtained from the Institutional Review Board of the Radboud university medical center, Nijmegen (protocol number: 2017-3621).
Consent to participate
All the participants provided informed consent when starting the web survey and before they were asked substantive questions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of “The ARCH study group” are listed in acknowledgement section.
Appendix
Appendix
See Table 5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stöcker, J.K., Vonk, M.C., van den Hoogen, F.H.J. et al. Opening the black box of non-pharmacological care in systemic sclerosis: a cross-sectional online survey of Dutch health professionals. Rheumatol Int 41, 1299–1310 (2021). https://doi.org/10.1007/s00296-020-04765-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04765-4