Abstract
The occurrence of diffuse large B-cell lymphoma (DLBCL) in the course of Sjogren’s syndrome (SS) is considered to be equally related either to the development of DLBCL de novo or to the transformation from marginal zone lymphoma (MZL). However, the question of possible clonal relationship between MZL and DLBCL in the group of SS patients remains open. Here we present the data concerning 194 patients with lymphoma complicated SS followed up at Nasonova Research Institute of Rheumatology during the last 22 years. Molecular analysis of tumor cells was performed for 6 SS patients who had developed both MZL and DLBCL. To assess clonal relationship between each of the tumor pairs immunoglobulin heavy chain (IGH) gene rearrangements were identified according BIOMED-2 protocol by means of multiplex polymerase chain reaction followed by GeneScan fragment analysis. Despite different localization MZL and DLBCL were clonally related in five tumor pairs. The median time to transformation was 11 months (range 0–78 months). MZL and DLBCL were clonally related in most cases from our cohort of SS patients. No statistically significant difference in survival between patients with DLBCL transformed from MZL and patients with de novo DLBCL was found in the cohort of SS patients investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sjogren’s syndrome (SS) is a systemic autoimmune rheumatic disease (SARD) associated with an increased risk of lymphoma [1, 2]. Among SS-associated lymphomas the most common histological types are the marginal zone lymphoma (MZL), especially the parotid gland mucosa-associated lymphoid tissue (MALT) lymphoma, and the diffuse large B-cell lymphoma (DLBCL) [3,4,5,6,7,8].
Unlike with parotid gland MALT lymphoma the putative mechanisms lying behind the association of DLBCL with SS are still not well understood [9,10,11]. DLBCL can develop de novo or as a result of the transformation from low-grade (indolent) lymphoma. Three types of MZL according to the sites involved are defined according to the latest 2016 World Health Organization (WHO) classification: extranodal MZL of MALT (commonly termed MALT lymphoma), nodal MZL (NMZL), and splenic MZL (SMZL) [12]. Histologic transformation to a DLBCL can occur in all types of MZL [13].
Histological criteria for the transformation of MZL into DLBCL are not well outlined. Most authors noted sheets of large cells or clusters of at least 20 large cells to be the marker of transformation into DLBCL [14,15,16,17]. While others defined transformed cases to have more than 30–50% of diffusely scattered large tumor cells [18, 19].
Two conditions might be regarded as MZL to DLBCL transformation in the routine clinical practice. The first is the appearance of solid or sheet-like proliferation of centroblast-like or immunoblast-like cells in a biopsy sample in addition to the areas that meet standard morphological criteria of MZL. Second applies to DLBCL developing in the patient with previously diagnosed MZL. However, the assumptions about MZL and DLBCL clonal relationship based exclusively on the histological data are rather controversial in general and might have limited probative value for gastric lymphoma only [16, 20,21,22,23,24,25].
This study is aimed to investigate possible clonal relationship between MZL and DLBCL developed in the patients with SS.
Materials and methods
We searched the files of the V.A. Nasonova Research Institute of Rheumatology (Moscow, Russia) from June 01, 1997 until June 01, 2019 for MZL cases with synchronous or metachronous DLBCL complicating SARD at diagnosis or later. Inclusion criteria were: over 18 years of age, availability of medical records confirming the SARD diagnosis, biopsy-proven MZL with synchronous or metachronous biopsy-proven DLBCL, and the availability of paraffin blocks for molecular analysis.
All MZL lymphomas and DLBCLs were identified by the surgical biopsy of a lymph node or extranodal tissue (except for the bone marrow). The tissue specimens were fixed in 10% formalin, routinely processed, and embedded in paraffin. The original hematoxylin and eosin (H&E)-stained slides were prepared for all cases.
Immunohistochemical studies with a panel of B- and T-cell markers were carried out on the formalin-fixed paraffin-embedded (FFPE) tissue. The antibodies used in the immunohistochemical studies, diluted as suggested by the manufacturers, are presented in Table 1. After dewaxing and heat-induced antigen retrieval, sections were stained using Autostainer Link 48 (Dako, Denmark) according to the manufacturer’s instructions.
In one of our cases (Case 6), the morphologically distinct tumor components were microdissected to determine the clonal relationship between the MALT lymphoma and DLBCL components.
DNAs from FFPE samples were extracted as described in [26]. The BIOMED-2 primer set and standardized protocol were used to study immunoglobulin heavy chain (IGH) gene rearrangements [27]. IGH framework (FR) 1, 2, and 3 assays (Tube A, Tube B, and Tube C, respectively) were used to reveal VH-JH rearrangements. The fragments were detected on an ABI PRISM 3130 Genetic Analyzer (Applied Biosystems, Foster City, CA) and the data were analyzed with GeneMapper software version 4.0 (Applied Biosystems, Foster City, CA).
Overall survival was estimated by the Kaplan–Meier method and was calculated as the time from the DLBCL diagnosis until death or the last follow up. Log-rank test was used to compare overall survival between the groups of patients with DLBCL transformed from MZL and de novo DLBCL.
Results
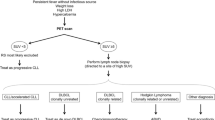
We identified 169 patients with MZL and 25 patients with DLBCL complicating SARD diagnosed in our hospital during the 22-year interval. Six of these patients had two lymphomas: MZL and synchronous or metachronous DLBCL (Table 2). All six patients were women, median age 61 years (range 54–73 years) at the time of MZL diagnosis and had SS alone (Cases 1–4) or in association with limited cutaneous systemic sclerosis (Case 5) or with rheumatoid arthritis (Case 6). Cases 1 and 6 also had Hashimoto’s thyroiditis. Based on the full staging evaluation, in five cases, the diagnosis was established as extranodal MZL of MALT type, and in one case, NMZL (Case 4). MALT lymphoma was found in the salivary gland in four cases and in the bronchial wall in one case. The proliferation fraction was measured by Ki-67 antibodies and was unusually high for MZL in three out of four cases (Cases 3–5) (Fig. 1), ranging from 40 to 50%. In two patients (Cases 3 and 6), DLBCL was diagnosed simultaneously with MZL, and in four cases (Cases 1, 2, 4, and 5), 8–78 months after MZL. In all cases except for Case 6, the location of DLBCL was different from that of MZL. In Case 6, composite lymphoma (MALT lymphoma/DLBCL) of the parotid gland was diagnosed. In three patients (Cases 1, 3, and 4), the DLBCL was confined to extranodal sites, and other three patients (Cases 2, 5, and 6) presented with nodal and extranodal DLBCL.
Cases of MZL with a high proliferative activity index. Case 3. The parotid salivary gland affected by MALT lymphoma. a Hematoxylin and eosin (H&E) stains, b Ki-67; Case 4. The lymph node affected by MZL. c H&E stains, d Ki-67; Case 5. The parotid salivary gland affected by MALT lymphoma. e H&E stains, f Ki-67; All photomicrographs original magnification ×400
Immunohistochemical subtyping of DLBCLs according to the Hans algorithm was performed for all cases [28]. Based on their expression patterns, two cases of DLBCL were allocated to the germinal center of the B-cell (GCB) subtype and four cases into the non-GCB subtype.
Monoclonal rearrangement of the IGH gene was detected in both specimens for all six tumor pairs. The results of the IGH clonality analysis for six paired samples of MZL and DLBCL are presented in Table 3. Identical clonal patterns of MZL and DLBCL were observed in five tumor pairs (Cases 1–5), showing the clonal relationship of the tumors in these cases. In Case 6, fragment analysis of the frame region 3 by polymerase chain reaction (PCR) products from microdissected MALT lymphoma and DLBCL components showed different clonal pattern rearrangements of the IGH gene.
To assess whether patients with SS-related DLBCL transformed from MZL (5 patients) have a worse prognosis compared with patients with de novo SS-related DLBCL (17 patients), we compared overall survival in both groups. We did not find any statistically significant difference in survival between these groups (p = 0.139) (Fig. 2).
Search strategy
We performed a literature search in Medline, Scopus and Web of Science up to March 2019, according to the published guidance [29]. We used the following keywords: “Sjögren's syndrome”, “lymphoma”, “mucosa-associated lymphoid tissue lymphoma”, “diffuse large B-cell lymphoma”, and “transformation” to identify the relevant original articles, letters to the editor, and case reports published in English. There were no exclusion criteria.
Discussion
In this study, we investigated the clonal relationship between low- and high-grade lymphomas in six patients with SS. In all cases, low-grade lymphoma was classified as NMZL or MALT lymphoma. Both MZL subtypes are the most common histological type of lymphoma developing in SS patients. MZLs have the potential to progress into a more aggressive histologic type, predominantly in DLBCL [18, 30,31,32].
Histologic transformation of MALT lymphoma and NMZL is, according to Conconi and colleagues, observed in 4% and in 3% of patients, respectively, with the median time for transformation being 32 months (range 12–144 months) after diagnosis of MZL [31]. Maeshima and colleagues reported the histological transformation of MALT lymphoma into DLBCL in 8% of their patients, with the median time to the transformation of 48 months (range 2–139 months) after the MALT lymphoma diagnosis [18]. In our cohort, the transformation of MZL into DLBCL was observed in 3% of patients and median time to transformation was 11 months (range 0–78 months).
The emergence of DLBCL in the course of SS could be equally attributable either to the development de novo or to the transformation from MZL. After reviewing all the relevant literature, we found 14 cases of SS and DLBCL with morphological signs showing the origin of DLBCL from MZL: 11 cases from MALT lymphoma and 3 cases from NMZ [4, 33,34,35]. In 11 additional cases, DLBCL was diagnosed either concurrently with MZL (but in a different location) or 10–84 months after the MALT lymphoma diagnosis (Table 4) [4, 34,35,36,37,38,39]. Royer and colleagues reported a DLBCL case diagnosed in the retroperitoneal lymph nodes 10 months after the initial bronchial MALT lymphoma in a 60-year-old man with SS [4]. In both lymphomas, t(14;18) was detected, strongly suggesting their clonal relationship. Strunk and colleagues described a case of a rapidly progressing Epstein–Barr virus-driven transformation of parotid gland MALT lymphoma into DLBCL with liver, lung, kidney, bone morrow, and lymph nodes involvement in a 42-year-old female patient with SS [36]. MALT lymphoma and DLBCL in this case had identical IGH rearrangement profiles. However, other cases had not been studied using molecular methods to establish their clonal relationship.
In our group, the fragment analysis showed identical clonal IGH gene rearrangement patterns between the MZL and DLBCL in each of the five tumor pairs (Cases 1–5), indicating the clonal identity of the two lymphomas. In all these cases, low- and high-grade lymphomas had different localization. In only one patient (Case 6), both lymphomas (DLBCL and MALT lymphoma) were detected in the same location, which initially led us to the erroneous conclusion that DLBCL results from MALT lymphoma progression. However, the fragment analysis showed different clonal IGH gene rearrangement patterns from microdissected MALT lymphoma and DLBCL components, showing that these lymphomas are not clonally related.
The Ki-67 proliferation index is low in MZL [40]. Three of our four cases of MZL with the subsequent transformation into DLBCL had a high index of proliferative activity of tumor cells (Table 2). The Ki-67 proliferation index was not used to diagnose the transformation to DLBCL given the lack of an agreed cutoff for this distinction [17]. However, Petit and colleagues showed that the increase in Ki-67 expression in MZL is an independent parameter associated with a worse outcome [41]. Considering the results of our study, we think that further research is needed to decide whether the high proliferative activity index of tumor cells in MZL is a risk factor for MZL transformation. The small number of cases and the retrospective nature of the study did not allow us to identify risk factors for the transformation of MZL into DLBCL in patients with SS.
We suggest that in SS patients with both MZL and DLBCL these tumors are usually clonally related, which most likely shows that high-grade DLBCL emerged from low-grade MZL. Patients with MZL, therefore, need to be closely monitored by a physician for timely diagnosis of the high-grade DLBCL. We are confident that estimates whether DLBCL results from low-grade B-cell lymphoma progression should only be done based on molecular analysis of tumor clones even in the cases with histological features suggesting such transformation.
References
Smedby KE, Baecklund E, Askling J (2006) Malignant lymphomas in autoimmunity and inflammation: a review of risks, risk factors, and lymphoma characteristics. Cancer Epidemiol Biomark Prev 15(11):2069–2077. https://doi.org/10.1158/1055-9965.EPI-06-0300
Smedby KE, Vajdic CM, Falster M, Engels EA, Martínez-Maza O, Turner J, Hjalgrim H, Vineis P, Costantini A, Bracci PM, Holly EA, Willett E, Spinelli JJ, La Vecchia C, Zheng T, Becker N, De Sanjosé S, Chiu BC, Dal Maso L, Cocco P, Maynadié M, Foretova L, Staines A, Brennan P, Davis S, Severson R, Cerhan JR, Breen EC, Birmann B, Grulich AE, Cozen W (2008) Autoimmune disorders and risk of non-Hodgkin lymphoma subtypes: a pooled analysis within the InterLymph Consortium. Blood 111(8):4029–4038. https://doi.org/10.1182/blood-2007-10-119974
Tzioufas AG (1996) B-cell lymphoproliferation in primary Sjogren’s syndrome. Clin Exp Rheumatol 14(Suppl. 14):S65–S70
Royer B, Cazals-Hatem D, Sibilia J, Agbalika F, Cayuela JM, Soussi T, Maloisel F, Clauvel JP, Brouet JC, Mariette X (1997) Lymphomas in patients with Sjogren's syndrome are marginal zone B-cell neoplasms, arise in diverse extranodal and nodal sites, and are not associated with viruses. Blood 90(2):766–775
Voulgarelis M, Dafni UG, Isenberg DA, Moutsopoulos HM (1999) Malignant lymphoma in primary Sjogren’s syndrome: a multicenter, retrospective, clinical study by the European Concerted Action on Sjogren’s Syndrome. Arthritis Rheum 42(8):1765–1772. https://doi.org/10.1002/1529-0131(199908)42:8%3c1765:AID-ANR28%3e3.0.CO;2-V
Baimpa E, Dahabreh IJ, Voulgarelis M, Moutsopoulos HM (2009) Hematologic manifestations and predictors of lymphoma development in primary Sjogren syndrome: clinical and pathophysiologic aspects. Medicine 88(5):284–293. https://doi.org/10.1097/MD.0b013e3181b76ab5
Nocturne G, Mariette X (2015) Sjögren syndrome-associated lymphomas: an update on pathogenesis and management. Br J Haematol 168(3):317–327. https://doi.org/10.1111/bjh.13192
Theander E, Henriksson G, Ljungberg O, Mandl T, Manthorpe R, Jacobsson LTH (2006) Lymphoma and other malignancies in primary Sjogren’s syndrome: a cohort study on cancer incidence and lymphoma predictors. Ann Rheum Dis 65(6):796–803. https://doi.org/10.1136/ard.2005.041186
Dong L, Chen Y, Masaki Y, Okazaki T, Umehara H (2013) Possible mechanisms of lymphoma development in Sjögren’s syndrome. Curr Immunol Rev 9(1):13–22. https://doi.org/10.2174/1573395511309010003
Alunno A, Leone MC, Giacomelli R, Gerli R, Carubbi F (2018) Lymphoma and lymphomagenesis in primary Sjögren’s syndrome. Front Med (Lausanne) 13(5):102. https://doi.org/10.3389/fmed.2018.00102
Routsias JG, Goules JD, Charalampakis G, Tzima S, Papageorgiou A, Voulgarelis M (2013) Malignant lymphoma in primary Sjögren’s syndrome: an update on the pathogenesis and treatment. Semin. Arthritis Rheum 43(2):178–186. https://doi.org/10.1016/j.semarthrit.2013.04.004
Swerdlow S, Campo E, Harris N, Jaffe E, Pileri S, Stein H, Thiele J (2017) WHO classification of tumours of haematopoietic and lymphoid tissues. IARC Press, Lyon (ISBN-13 9789283244943-13 Print Book)
Agbay RL, Loghavi S, Medeiros LJ, Khoury JD (2016) High-grade transformation of low-grade B-cell lymphoma: pathology and molecular pathogenesis. Am J Surg Pathol 40(1):e1–e16. https://doi.org/10.1097/PAS.0000000000000561
Ferreri A, Freschi M, Dell’Oro S, Viale E, Villa E, Ponzoni M (2001) Prognostic significance of the histopathologic recognition of low and high-grade components in stage I-II B-cell gastric lymphomas. Am J Surg Pathol 25(1):95–102
De Jong D, Boot H, Taal B (2000) Histological grading with clinical relevance in gastric mucosa-associated lymphoid tissue (MALT) lymphoma. Cancer Res 156:27–32
Chan JK, Ng CS, Isaacson PG (1990) Relationship between high-grade lymphoma and low-grade B-cell mucosa-associated lymphoid tissue lymphoma (MALToma) of the stomach. Am J Pathol 136(5):1153–1164
Molina TJ, Lin P, Swerdlow SH, Cook JR (2011) Marginal zone lymphomas with plasmacytic differentiation and related disorders. Am J Clin Pathol 136(2):211–225. https://doi.org/10.1309/AJCP63OGXHXCSKSC
Maeshima AM, Taniguchi H, Toyoda K, Yamauchi N, Makita S, Fukuhara S, Munakata W, Maruyama D, Kobayashi Y, Tobinai K (2016) Clinicopathological features of histological transformation from extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue to diffuse large B-cell lymphoma: an analysis of 467 patients. Br J Haematol 174(6):923–931. https://doi.org/10.1111/bjh.14153
Berger F, Felman P, Thieblemont C, Pradier T, Baseggio L, Bryon PA, Salles G, Callet-Bauchu E, Coiffier B (2000) Non-MALT marginal zone B-cell lymphomas: a description of clinical presentation and outcome in 124 patients. Blood 95(6):1950–1956
Matolcsy A, Nagy M, Kisfaludy N, Kelényi G (1999) Distinct clonal origin of low-grade MALT-type and high-grade lesions of a multifocal gastric lymphoma. Histopathology 34(1):6–8
Cabras AD, Candidus S, Fend F, Kremer M, Schulz S, Bordi C, Weirich G, Höfler H, Werner M (2001) Biclonality of gastric lymphomas. Lab Investig 81(7):961–967
Barth TF, Bentz M, Leithäuser F, Stilgenbauer S, Siebert R, Schlotter M, Schlenk RF, Döhner H, Möller P (2001) Molecular-cytogenetic comparison of mucosa-associated marginal zone B-cell lymphoma and large B-cell lymphoma arising in the gastro-intestinal tract. Genes Chromosomes Cancer 31(4):316–325. https://doi.org/10.1002/gcc.1150
Alpen B, Wündisch T, Dierlamm J, Börsch G, Stolte M, Neubauer A (2004) Clonal relationship in multifocal non-Hodgkin’s lymphoma of mucosa-associated lymphoid tissue (MALT). Ann Hematol 83(2):124–126. https://doi.org/10.1007/s00277-003-0763-5
Geurts-Giele WR, Tettero IL, Dinjens WN, Lam KH, Langerak AW (2013) Successive B-cell lymphomas mostly reflect recurrences rather than unrelated primary lymphomas. Am J Clin Pathol 140(1):114–126. https://doi.org/10.1309/AJCPI14GXNWASVUZ
Fujita A, Tajika M, Tanaka T, Ishihara M, Hirayama Y, Mizuno N, Hara K, Hijioka S, Imaoka H, Yoshida T, Okuno N, Hieda N, Hirayama T, Shibuya H, Kondo H, Suzuki H, Toriyama K, Yatabe Y, Yamao K, Niwa Y (2017) A case of API2-MALT1-positive gastric MALT lymphoma with concomitant diffuse large B-cell lymphoma. Nagoya J Med Sci 79(2):251–257. https://doi.org/10.18999/nagjms.79.2.251
Sidorova JV, Biderman BV, Nikulina EE, Sudarikov AB (2012) A simple and efficient method for DNA extraction from skin and paraffin-embedded tissues applicable to T-cell clonality assays. Exp Dermatol 21(1):57–60. https://doi.org/10.1111/j.1600-0625.2011.01375.x
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL, Delabesse E, Davi F, Schuuring E, García-Sanz R, van Krieken JH, Droese J, González D, Bastard C, White HE, Spaargaren M, González M, Parreira A, Smith JL, Morgan GJ, Kneba M, Macintyre EA (2003) Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 17(12):2257–2317. https://doi.org/10.1038/sj.leu.2403202
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan Z, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103(1):275–282. https://doi.org/10.1182/blood-2003-05-1545
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31(11):1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Ghesquieres H, Berger F, Felman P, Callet-Bauchu E, Bryon PA, Glehen A, Thieblemont C, Baseggio L, Michallet AS, Coiffier B, Salles G (2006) Clinicopathologic characteristics and outcome of diffuse large B-cell lymphomas presenting with an associated low-grade component at diagnosis. J Clin Oncol 24(33):5234–5241. https://doi.org/10.1200/JCO.2006.07.5671
Conconi A, Franceschetti S, von Hohenstaufen K, Margiotta-Casaluci G, Stathis A, Moccia AA, Bertoni F, Ramponi A, Mazzucchelli L, Cavalli F, Gaidano G, Zucca E (2015) Histologic transformation in marginal zone lymphomas. Ann Oncol 26(11):2329–2335. https://doi.org/10.1093/annonc/mdv368
Casulo C, Friedberg J (2017) Transformation of marginal zone lymphoma (and association with other lymphomas). Best Pract Res Clin Haematol 30(1–2):131–138. https://doi.org/10.1016/j.beha.2016.08.029
Kojima M, Tsukamoto N, Yokohama A, Suzuki Y, Shimizu K, Nishikawa M, Murayama K, Miyanaga T, Isoda A, Shimizu K, Itoh H, Masawa N, Yoshida K, Inagaki H (2009) B-cell lymphoma associated with Sjogren’s syndrome among Japanese patients: a clinicopathologic and immunohistochemical study of 15 cases. J Clin Exp Hematop 49(2):89–95
Voulgarelis M, Ziakas PD, Papageorgiou A, Baimpa E, Tzioufas AG, Moutsopoulos HM (2012) Prognosis and outcome of non-Hodgkin lymphoma in primary Sjogren syndrome. Medicine (Baltimore) 91(1):1–9. https://doi.org/10.1097/MD.0b013e31824125e4
Vasaitis L (2017) Lymphoma studies in patients with Sjögren's syndrome. Dissertation, Upsaliensis: Acta Universitatis Upsaliensis. ISBN 978-91-554-9912-9
Strunk JE, Schuttler C, Ziebuhr J, Stowasser M, Nöhte M, Mayer K, Bräuninger A, Gattenlöhner S (2013) Epstein–Barr virus-induced secondary high-grade transformation of Sjogren’s syndrome-related mucosa-associated lymphoid tissue lymphoma. J Clin Oncol 31(17):e265–e268. https://doi.org/10.1200/JCO.2012.46.8439
Solans-Laque R, Lopez-Hernandez A, Bosch-Gil JA, Palacios A, Campillo M, Vilardell-Tarres M (2011) Risk, predictors, and clinical characteristics of lymphoma development in primary Sjogren’s syndrome. Semin Arthritis Rheum 41(3):415–423. https://doi.org/10.1016/j.semarthrit.2011.04.006
Biasi D, Caramaschi P, Ambrosetti A, Carletto A, Mocella S, Randon M, Bambara LM (2001) Mucosa-associated lymphoid tissue lymphoma of the salivary glands occurring in patients affected by Sjogren’s syndrome: report of 6 cases. Acta Haematol 105(2):83–88. https://doi.org/10.1159/000046539
Ramos-Casals M, Civita L, de Vita S, Solans R, Luppi M, Medina F, Caramaschi P, Fadda P, Marchi G, Lopez-Guillermo A, Font J, SS-HCV Study Group (2007) Characterization of B cell lymphoma in patients with Sjogren’s syndrome and hepatitis C virus infection. Arthritis Rheum 57(1):161–170. https://doi.org/10.1002/art.22476
Ferry JA (2008) Extranodal lymphoma. Arch Pathol Lab Med 132(4):565–578. https://doi.org/10.1043/1543-2165(2008)132[565:EL]2.0.CO;2
Petit B, Chaury MP, Le Clorennec C, Jaccard A, Gachard N, -Judge S, Labrousse F, Cogné M, Bordessoule D, Feuillard J (2005) Indolent lymphoplasmacytic and marginal zone B-cell lymphomas: absence of both IRF4 and Ki67 expression identifies a better prognosis subgroup. Haematologica 90(2):200–206
Acknowledgements
The manuscript was edited by MDPI (https://www.mdpi.com/authors/english)
Funding
None.
Author information
Authors and Affiliations
Contributions
VRG collected samples, collected clinical patient data, analyzed data, took part in study design, performed the statistical analysis, and wrote, edited, and reviewed the manuscript. NAP and SGR-L performed histopathological and immunohistochemical examinations, took part in study design, substantially contributed to the interpretation of the data, edited and reviewed the manuscript. NVR and YVS collected samples, performed molecular studies, took part in study design, substantially contributed to the interpretation of the data, edited and reviewed the manuscript. ABS: took part in study design, substantially contributed to the interpretation of the data, edited and reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the V.A. Nasonova Research Institute of Rheumatology Ethics Committee, reference number 19/18 on the 29/11/2018.
Informed consent
Informed consent was obtained from the patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Gorodetskiy, V.R., Probatova, N.A., Radenska-Lopovok, S.G. et al. Clonal relationship of marginal zone lymphoma and diffuse large B-cell lymphoma in Sjogren's syndrome patients: case series study and review of the literature. Rheumatol Int 40, 499–506 (2020). https://doi.org/10.1007/s00296-019-04470-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04470-x