Abstract
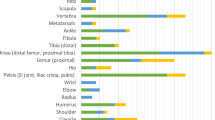
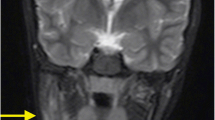
Chronic non-bacterial osteomyelitis (CNO) is a chronic inflammatory bone disease which usually manifests in children and adolescents. There are a few data about pathogenesis and treatment. The aim of the study to compare the efficacy of different treatment approaches in pediatric CNO cohort patient. Fifty two children (25 boys and 27 girls) with CNO with average age at the onset of the disease 8.4 years (5.4; 11.0), number of foci − 3.0 (2.0; 6.0, incl. multifocal cases in 80.8%). Non-steroid anti-inflammatory drugs (NSAID) was the first-line treatment for non-vertebral cases, as well as pamidronate (PAM) for vertebral involvement. Second-line treatment includes sulfasalazine (SSZ), methotrexate (MTX), PAM and tumor necrosis factor-α inhibitors (TNFα-inh). We evaluated the dynamics of pain, patient’s and physician’s (MDVAS) assessment with visual-analog scale (VAS) and ability to each medication to achieve remission of CNO activity. According to the NSAID, MTX, SSZ, PAM and TNFα-inh groups the following data were registered: patient’s VAS: − 14.2% (p = 0.05), − 50.0% (p = 0.04), − 23.1 (p = 0.89), − 83.3% (p = 0.0001), − 73.6% (p = 0.0007); painVAS: − 21.9% (p = 0.01), − 18.6% (p = 0.13), + 36.4 (p = 0.89), − 79.7% (p = 0.00016), − 74.1%, (p = 0.0015); MDVAS: − 13.8% (p = 0.13); − 56.4% (p = 0.09), + 30.8% (p = 0.89), − 74.7%, (p = 0.0001), − 82.1 (p = 0.0015) respectively. The ability of each treatment strategy to achieve the CNO remission was 52.6%, 44.4%, 57,1%, 88.8% and 73.3%, respectively (log-rank test, p = 0.001). The efficacy of treatment approaches for CNO depended on the severity of the disease. NSAID, methotrexate, and sulfasalazine were effective in forms without spine involvement, but pamidronate and TNF-a inhibitors were useful in vertebral forms of CNO. Pamidronate and TNF-a inhibitors more extensively suppressed CNO activity. The randomized controlled trials for assessment of the efficacy and safety of these medications is mandatory to confirm these results.


Similar content being viewed by others
References
Stern SH, Ferguson PJ (2013) Autoinflammatory bone diseases. Rheum Dis Clin North Am 39:735–749
Wipff J, Costantino F, Lemelle I, Pajot C, Duquesne A, Lorrot M, Faye A, Bader-Meunier B, Brochard K, Despert V, Jean S, Grall-Lerosey M, Marot Y, Nouar D, Pagnier A, Quartier P, Job-Deslandre C (2015) A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis Rheumatol 67:1128–1137
Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A, Grote V, Diebold J, Jansson V, Schneider K, Belohradsky BH (2007) Classification of non-bacterial osteitis retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology 46:154–160
Laxer RM, Shore AD, Manson D, King S, Silverman ED, Wilmot DM (1988) Chronic recurrent multifocal osteomyelitis and psoriasis—a report of a new association and review of related disorders. Semin Arthritis Rheum 17:260–270
Schilling F, Marker-Hermann E (2003) Chronic recurrent multifocal osteomyelitis in association with chronic inflammatory bowel disease: entheropathic CRMO. Z Rheumatol 62:527–538
Borzutzky A, Stern S, Reiff A, Zurakowski D, Steinberg EA, Dedeoglu F, Sundel RP (2012) Pediatric chronic nonbacterial osteomyelitis. Pediatrics 130(5):e1190–e1197. https://doi.org/10.1542/peds.2011-3788
Hofmann SR, Schwarz T, Möller JC, Morbach H, Schnabel A, Rösen-Wolff A, Girschick HJ, Hedrich CM (2011) Chronic non-bacterial osteomyelitis is associated with impaired Sp1 signaling, reduced IL10 promoter phosphorylation and reduced myeloid IL-10 expression. Clin Immunol 141:317–327
Hofmann SR, Rösen-Wolff A, Tsokos GC, Hedrich CM (2012) Biological properties and regulation of IL-10 related cytokines and their contribution to autoimmune disease and tissue injury. Clin Immunol 143:116–127
Scianaro R, Insalaco A, Bracci Laudiero L, De Vito R, Pezzullo M, Teti A, De Benedetti F, Prencipe G (2014) Deregulation of the IL-1β axis in chronic recurrent multifocal osteomyelitis. Pediatr Rheumatol 12:30. https://doi.org/10.1186/1546-0096-12-30
Morbach H, Hedrich CM, Beer M, Girschick HJ (2013) Autoinflammatory bone disorders. Clin Immunol 147:185–196
Eleftheriou D, Gerschman T, Sebire N, Woo P, Pilkington CA, Brogan PA (2010) Biologic therapy in refractory chronic non-bacterial osteomyelitis of childhood. Rheumatology 49(8):1505–1512
Tronconi E, Miniaci A, Baldazzi M, Greco L, Pession A (2018) Biologic treatment for chronic recurrent multifocal osteomyelitis: report of four cases and review of the literature. Rheumatol Int 38:153–160
Sato H, Wada Y, Hasegawa E, Nozawa Y, Nakatsue T, Ito T, Kuroda T, Saeki T, Umezu H, Suzuki Y, Nakano M, Narita I (2017) Adult-onset chronic recurrent multifocal osteomyelitis with high intensity of muscles detected by magnetic resonance imaging, successfully controlled with tocilizumab. Intern Med 56:2353–2360
Gabay C, Palmer G (2009) Mutations in the IL1RN locus lead to autoinflammation. Nat Rev Rheumatol 9:480–482
Herlin T, Fiirgaard B, Bjerre M, Kerndrup G, Hasle H, Bing X, Ferguson PJ (2013) Efficacy of anti-IL-1 treatment in Majeed syndrome. Ann Rheum Dis 72:410–413
Aksentijevich I, Masters SL, Ferguson PJ et al (2009) Autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med 360:2426–2437
Girschick H, Finetti M, Orlando F, Schalm S, Insalaco A, Ganser G, Nielsen S, Herlin T, Koné-Paut I, Martino S, Cattalini M, Anton J, Mohammed Al-Mayouf S, Hofer M, Quartier P, Boros C, Kuemmerle-Deschner J, Pires Marafon D, Alessio M, Schwarz T, Ruperto N, Martini A, Jansson A, Gattorno M (2018) The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Paediatric Rheumatology International Trials Organisation (PRINTO) and the Eurofever registry. Rheumatology 57(8):1504. https://doi.org/10.1093/rheumatology/key143
Jansson AF, Müller TH, Gliera L, Ankerst DP, Wintergerst U, Belohradsky BH, Jansson V (2009) Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum 60:1152–1159
Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlöhner S, Hofmann U, Raab P, Girschick HJ (2010) Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther 12(2):R74
Hospach T, Langendoerfer M, von Kalle T, Maier J, Dannecker GE (2010) Spinal involvement in chronic recurrent multifocal osteomyelitis (CRMO) in childhood and effect of pamidronate. Eur J Pediatr 169:1105–1111
Schnabel A, Range U, Hahn G, Berner R, Hedrich CM (2017) Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol 44:1058–1065
Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV (2016) Chronic recurrent multifocal osteomyelitis (CRMO)—advancing the diagnosis. Pediatr Rheumatol 14:47. https://doi.org/10.1186/s12969-016-0109-1
Kaiser D, Bolt I, Hofer M, Relly C, Berthet G, Bolz D, Saurenmann T (2015) Chronic nonbacterial osteomyelitis in children: a retrospective multicenter study. Pediatr Rheumatol Online J 13:25. https://doi.org/10.1186/s12969-015-0023-y
Abril JC, Ramirez A (2007) Successful treatment of chronic recurrent multifocal osteomyelitis with indometacin. J Pediatr Orthop 27:587–591
Bellido T, Plotkin LI (2011) Novel actions of bisphosphonates in bone: preservation of osteoblast and osteocyte viability. Bone 49:50–55
Santra G, Sarkar RN, Phaujdar S, Banerjee S, Siddhanta S (2010) Assessment of the efficacy of pamidronate in ankylosing spondylitis: an open prospective trial. Singap Med J 51:883–887
Miettunen P, Wei X, Kaura D, Reslan WA, Aguirre AN, Kellner JD (2009) Dramatic pain relief and resolution of bone inflammation following pamidronate in 9 pediatric patients with persistent chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol 7:2. https://doi.org/10.1186/1546-0096-7-2
Hofmann C, Wurm M, Schwarz T, Neubauer H, Beer M, Girschick H, Morbach H (2014) A standardized clinical and radiological follow-up of patients with chronic non-bacterial osteomyelitis treated with pamidronate. Clin Exp Rheumatol 32(4):604–609
Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS, Lee TC, Fox E, Amarilyo G, Stern SM, Dvergsten JA, Haines KA, Rouster-Stevens KA, Onel KB, Cherian J, Hausmann JS, Miettunen P, Cellucci T, Nuruzzaman F, Taneja A, Barron KS, Hollander MC, Lapidus SK, Li SC, Ozen S, Girschick H, Laxer RM, Dedeoglu F, Hedrich CM, Ferguson PJ, Chronic Nonbacterial Osteomyelitis/Chronic Recurrent Multifocal Osteomyelitis Study Group and the Childhood Arthritis and Rheumatology Research Alliance Scleroderma, Vasculitis, Autoinflammatory and Rare Diseases Subcommittee (2017) Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.23462
Papapoulos SE, Cremers SC (2007) Prolonged bisphosphonate release after treatment in children. N Engl J Med 356:1075–1076
Patlas N, Golomb G, Yaffe P, Pinto T, Breuer E, Ornoy A (1999) Transplacental effects of bisphosphonates on fetal skeletal ossification and mineralization in rats. Teratology 60:68–73
Minsker DH, Manson JM, Peter CP (1993) Effects of the bisphosphonate, alendronate, on parturition in the rat. Toxicol Appl Pharmacol 121:217–223
Graepel P, Bentley P, Fritz H, Miyamoto M, Slater SR (1992) Reproduction toxicity studies with pamidronate. Arzneimittelforschung 42:654–667
Djokanovic N, Klieger-Grossmann C, Koren G (2008) Does treatment with bisphosphonates endanger the human pregnancy? Obstet Gynaecol Can 30:1146–1148
Green SB, Pappas AL (2014) Effects of maternal bisphosphonate use on fetal and neonatal outcomes. Health Syst Pharm 71:2029–2036
Deutschmann A, Mache CJ, Bodo K, Zebedin D, Ring E (2005) Successful treatment of chronic recurrent multifocal osteomyelitis with tumor necrosis factor alpha blockage. Pediatrics 116:1231–1233
Funding
This work supported by the Russian Foundation for Basic Research (Grant No. 18-515-57001).
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article or revising it critically. All authors approved the final version to be submitted for publication. Dr. Kostik, Dr. Kopchak, and Dr. Mushkin had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: Kostik, Kopchak, Mushkin. Acquisition of data: Kostik, Kopchak, Chikova, Isupova. Analysis and interpretation of data: Kostik, Kopchak, Mushkin.
Corresponding author
Ethics declarations
Informed consent
Informed consent obtained from all parents/guardians of minors participating in the study according to the declaration of Helsinki.
Ethical approval
The study was approved by the local Ethics Committee of St.-Petersburg State Pediatric University (protocol number 10/8 from 23.10.2017).
Conflict of interest
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Kostik, M.M., Kopchak, O.L., Chikova, I.A. et al. Comparison of different treatment approaches of pediatric chronic non-bacterial osteomyelitis. Rheumatol Int 39, 89–96 (2019). https://doi.org/10.1007/s00296-018-4151-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4151-9