Abstract
Objective
The aim of this study was to evaluate demographic, clinical, laboratory, imaging, histopathology characteristics, and treatment responses of children with Chronic nonbacterial osteomyelitis (CNO).
Methods
Retrospective multi-center case series study of pediatric patients diagnosed with CNO treated at five tertiary centers in south China.
Results
Totally there were 18 patients diagnosed as CNO between 2014 and 2020. The median age of onset was 9.2 years (range 3.7–13.1) and 55.6% were female. Median delay in diagnosis was 10.9 months (range 1.0–72.0). The most frequent presenting symptoms were bone pain (100%) and fever (44.4%). Most patients had more than one lesion (median of 5, range 1–7). Most frequently affected bones were tibiofibula (88.9%) and femur (77.8%). The MRI characteristics mainly presented as bone edema and hyperintensity in bone marrow. Bone biopsy was conducted in 11 patients (61.1%) with inflammatory cells infiltration manifested as chronic osteomyelitis, and none showed bacterial infection or tumor. In treatment, non-steroid anti-inflamatory drugs (NSAIDs) is used as the first-line drug followed by steriods, methotexate (MTX), salazosulfadimidine (SASP), Bisphosphonates and TNF-α inhibitor. Two refractory cases received combination therapy with Bisphosphonates and TNF-α inhibitor, and achieved good therapeutic effect.
Conclusions
The present study described a multicenter series of CNO from south China and highlighted the clinical features, laboratory tests, imaging characteristics and treatment outcomes. Increasing awareness of this disease is important to decrease time to diagnosis, improve access to treatment, and reduce complications.
Similar content being viewed by others
Introduction
Chronic nonbacterial osteomyelitis (CNO) is a benign and noninfectious autoinflammatory bone disease that mostly affects children and adolescents [1,2,3]. In 1972, Giedion et al. first described four patients with subacute or chronic multifocal symmetrical osteomyelitis, which mostly affects the growth plates of long bones [4]. Some scholars subsequently described similar cases and gave the diagnostic term “chronic recurrent multifocal osteomyelitis (CRMO)” [5]. Recurrent flares of inflammatory bone pain related to aseptic osteomyelitis are the major symptoms of the disease. The clinical presentation varies widely, from mild, unifocal, and time-limited bone involvement to severe, chronically active, or recurrent disease with multifocal bone lesions [5,6,7,8]. Thus, the name “CNO” has been proposed to encompass them all [9]. In adults, the term SAPHO syndrome is commonly used when referring to manifestations of the disease, which include synovitis, acne, pustulosis, hyperostosis, and osteitis [10]. To date, whether CNO and SAPHO syndrome are different manifestations of the same disease at different ages of onset or different outcomes of different clinical manifestations of the same disease remains unresolved [11].
Epidemiological data on CNO from Chinese population are limited. The average age at onset of the disease is 7–12 years, but the delay in diagnosis from the onset of symptoms is usually around 1 year [12]. A study conducted in Germany reported an incidence of 0.4 per 100,000 children [13]. The current incidence of the disease in other regions is unknown. The true incidence of CNO has likely been underestimated in past studies [14]. In most multicenter studies from North America and Europe, there is a female predominance with a female:male ratio of approximately 2:1. However, in similar studies from India and Japan, a male predominance is observed [8, 12]. To date, CNO is usually diagnosed by exclusion with magnetic resonance imaging (MRI) and/or through bone biopsy, which reveals chronic inflammation without infectious and oncological agents. The treatment protocol for CNO includes NSAIDs, steroids, MTX, SASP, TNF-α inhibitors, and bisphosphonates.
Although the awareness of CNO has increased over the past decade, misdiagnosis and delays in treatment still persist. Reliable diagnostic criteria and treatment protocols are lacking, and more multicenter studies on CNO are needed. To improve our understanding of the disease, we sought to evaluate the demographic and clinical characteristics, radiological findings, as well as treatment responses in pediatric patients with CNO at five tertiary centers in South China.
Methods
Patients under 18 years old diagnosed with CNO between 2014 and 2021 were enrolled at five tertiary centers in South China: Children’s Hospital of Nanjing Medical University, Children’s Hospital of Fudan University, Children’s Hospital of Soochow University, Children’s Hospital of Zhejiang University School of Medicine, and Children’s Hospital of Chongqing Medical University. The study was approved by local Ethics Review Board, and granted exemption of informed consent. Clinical characteristics, such as age, sex, family history, age at onset of symptoms, delay in diagnosis, symptoms, comorbidities, and treatments, were recorded. Available laboratory evaluation images, including plain radiographs, computed tomography (CT), Tc99 bone scan, MRI, and histology from bone biopsy were collected. Literature review was conducted on the case series of CNO reported abroad, and clinical comparison was made among our study and foreign CNO cohorts.
The diagnosis of CNO was defined as the presence of unifocal or multifocal inflammatory bone lesions with radiological and/or histopathological characteristics compatible with this diagnosis [15]. Infectious, oncological, or other inflammatory diseases were excluded. Response to treatment was assessed by improvement in pain and serologic markers of inflammation as well as radiographic proof of bone healing. The pain was evaluated by Visual Analogue Scale/Score. “No response” was defined as persistent pain with elevated inflammatory markers and abnormal signal on MRI.“Complete response/Remission” was defined as an 80% or more remission of clinical symptoms and imaging manifestation as well as normal inflammatory markers. The remission of 20% ~ 80% is “partial response”.
Statistical analyses
All statistical analyses were performed using SPSS 17.0. Continuous variables with normal distribution were presented as mean ± SD or median (IQR or range).
Results
General
Between 2014 and 2021, 18 patients were enrolled. Main demographic and clinical characteristics are described in Table 1. The median age at onset of the disease was 9.2 years (range 3.66–13.08) and 55.6% (n = 10) were female. The median time from onset to diagnosis was 10.9 months with a range of 1–72 months. The median follow-up was 16 months.
Clinical presentation
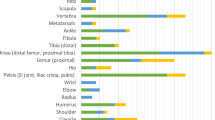
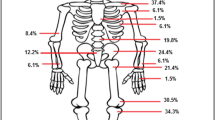
Most of the patients had a recurrent multifocal disease pattern, and a median of 5 bone lesions (range 1–7). Bone lesions affecting the appendicular skeleton were seen in 100%, including 38.9% (n = 7) in the upper limbs and 88.9% (n = 16) in lower extremities; while 38.9% (n = 7) had axial skeleton involvement. Most frequently affected bones were femur (77.8%), tibiofibula (88.9%), radius and ulna (33.3%), humerus (22.2%) and calcaneus (22.2%). Two patients had clavicle involvement. In one of these patients, CNO only affected the left clavicle, while in another one also affected mandible, sternum and lower extremity bones. One patient (case 18) had Right 12th rib and cervical spine involvement.
The initial symptom was bone pain in all patients. 22.2% presented local swelling, 27.8% limp, and 44.4% fever. Of the 18 patients, 8 (44.4%) had comorbid inflammatory arthritis. Case 18, who had rib and cervical spine involvement, also had mild acne, enthesitis and a appendix ulcer, which didn’t meet the diagnostic criteria of inflammatory bowel disease or Behcet’s disease. No patients in this series had psoriasis, inflammatory bowel disease, palmoplantar pustulosis, uveitis or severe acne. No patients had a first- or second-degree relative with history of autoimmunity.
The clinical scores for Nonbacterial Osteitis (NBO scores) was used to help diagnosis, which provided by Annette F. Jansson et al. [16]. The average score of our patients was 39 points, ranged from 30 points to 53 points.
Laboratory tests
In terms of laboratory studies, normal white blood counts were observed at onset in most patients, except for two patients with mild leukocytosis. Mean erythrocyte sedimentation rate (ESR) was 57.5 ± 42.2 mm/h, and 12 patients (66.7%) had elevated ESR over 20 mm/h. Mean C-reactive protein (CRP) was 48.8 ± 48.8 mg/L, 11 patients (61.1%) had CRP over the normal value of 8 mg/L. In 9 patients, both CRP and ESR were elevated simultaneously. No patients had positive ANA or positive HLA-B27. In all cases, bacterial cultures were negative. Four patients accepted genetic testing. Except for several known polymorphisms, no mutations were detected.
Imaging findings and bone biopsy
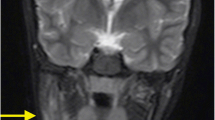
Results from imaging studies are detailed in Table 2. Among eight patients for whom plain radiographs were available for review, three showed Bony roughness, one showed bone enlargement and pathologic fracture and the others showed no abnormalities. Ten patients underwent computerized tomography, seven showed bone destruction, three showed uneven density of bone marrow, and one showed bony expansion. Seventeen patients underwent MRI of the main sites of localized pain, revealing abnormal bone findings in all cases: 82.3% showed increased signal in STIR, 11.7% bone edema, and 11.7% periostitis (Figs. 1 and 2 showed increased signal in STIR before and after treatment respectively). Twelve patients underwent three-phase Tc99 bone scintigraphy; in all of them, there was increased tracer uptake in the affected region (Fig. 3). Bone biopsy was performed in 11 patients (61.1%), showing adipose tissue and proliferating fibrous tissue and blood vessels were seen between bone trabeculae; scattered lymphocytes and plasma cells were observed, without evidence of infection, malignancy, or histiocytosis (Fig. 4).
Pathological findings in patients with chronic nonbacterial osteomyelitis (400×). Adipose tissue and proliferating fibrous tissue (black arrow) were seen between bone trabeculae, scattered lymphocytes (red arrow) and plasma cells (blue arrow) were observed, without evidence of infection, malignancy, or histiocytosis
Treatment
In terms of treatment, patients received NSAIDs (n = 16), methotrexate (n = 7), corticosteroids (n = 8), sulfasalazine (n = 2), bisphosphonates (n = 8), TNF-α inhibitor (n = 5), and thalidomide (n = 1). Decision of which therapeutic agent to use and in which order relied on the treating physician’s criteria. NSAIDs were used as the first-line therapy, followed by disease-modifying anti-rheumatic agents such as methotrexate or sulfasalazine. Patients who failed above treatments were placed on TNF inhibitors or bisphosphonates. The treatment protocols and outcomes of all patients were shown in Table 3. Three patients (case 3, case 13 and case 16) relapsed, two of whom (case3 and case 13) stopped taking drugs on their own. Case 15 and 16 received both TNF inhibitors and bisphosphonates therapy after NSAIDs, steroids and MTX therapy failed, which achieved good results. Three patients (case 1, case 12 and case 18) had spine involvement. Case 1 was treated with NSAIDs, SASP and steroids, achieved remission on medication. Case 12 was lost to follow up. Case 18 was treated with NSAIDs, MTX and pamidophosphate for 3 months with partial response. We had 11.1% remission without medicines in a median follow-up of 16 months.
Discussion
The present study was a multicenter series of CNO patients from five medical centers in South China. Compared with previous reports, the clinical characteristics of our patients were a little different. (details in Table 4) [8, 12, 15, 17,18,19,20,21,22,23,24,25] The female advantage in China is not such obvious as European countries [8, 12, 15, 18, 22,23,24,25]. The median age at diagnosis and diagnostic delays were 9.2 years and 10.2 months, respectively. The diagnostic delay ranged from 1 to 72 months, suggesting that CNO is still sometimes not well recognized in our country. In term of clinical manifestation, bone pain is still the most frequency symptom, but the fever rate in our study, which up to 44.4%, is more higher than that in other studies [17, 18, 20, 22, 24]. This may be related to bone inflammation. The most common bones involved in our study is the long bones of the limbs, especially the lower bones. In cases of Europe and USA, the clavicle, pelvis and spine are more frequently involved [8]. The comorbidities of our patients are mainly arthritis, only one patient has acne and gastrointestinal ulcer. The gastrointestinal symptoms, palmoplantar pustulosis, psoriasis and acne are more frequently in European cases [8, 12, 20]. It is also different from other studies, our CNO patients had no family history, no HLA-B27 positivity and no ANA positivity, suggesting a different genetic background.
On physical examination, swelling is infrequently observed, but when the disease is active, it is a sign of specific points of bone sensitivity [9]. CNO most frequently involves the long bones, followed by the pelvic bones, the vertebral column or the shoulder girdle/clavicle [3, 26]. The bones involved tend to be symmetrical, except the clavicle. Unifocal long bone involvement needs to be distinguished from culture-negative bacterial osteomyelitis by blood bacterial culture or bone marrow [27].
Laboratory tests of CRMO are not specific. Routine inflammatory parameters (WBC, white blood cell count; CRP, C reactive protein; ESR, erythrocyte sedimentation rate) are usually normal or mildly elevated. Imaging techniques are vital for diagnosing CNO and for excluding differential diagnoses [28]. Of our patients, 94.5% were evaluated with MRI, 52.9% with X-ray, and 58.5% with CT, while 64.7% had a bone scintigraphy. Compared with X-ray and CT, MRI is the most sensitive imaging technique to determine the extent and severity of bone involvement, particularly in the early stage. They can detect bone edema even before bone erosions and sclerosis develop and help assess the inflammation of surrounding tissues [29, 30]. More recently, whole-body MRI has been reported to be useful to screen the entire skeleton for bone lesions [31]. Bone scintigraphy is also useful for this purpose. It provides a global skeletal assessment at a lower cost [32], which can show abnormal concentrations of radionuclides, indicating the site of lesions, but cannot distinguish between inflammation and bone marrow metabolic hyperplasia. The radiation is also harmful to the body.
Bone biopsies are usually performed to exclude chronic infections, malignancies, or other systemic diseases, especially in patients with unifocal lesions [33]. In the present study, 47.1% of our patients underwent a bone biopsy. The histopathological findings of CNO are nonspecific inflammatory changes. A bone biopsy followed by pathological and pathogenic examination is very helpful for differential diagnosis.
To help diagnosis, we used the clinical NBO scores provided by Annette F. Jansson et al. [16] Although the score provides a reference standard for the diagnosis of the disease, CNO continues to be a diagnosis of exclusion. Important differential diagnoses include malignancies, infections, immunodeficiency, Langerhans cell histiocytosis (LCH), and other autoinflammatory disorders [33].
Although three consensus treatment plans (CTPs) were developed for CNO patients refractory to NSAID monotherapy by the Childhood Arthritis and Rheumatology Research Alliance (CARRA) [34], therapy protocols of CNO are not yet standardized. In general, first-line treatment is NSAIDs, which may reduce the pain and, in some cases, decrease the number of bone lesions in 3 months [35]. Second-line treatments usually includes methotrexate, corticosteroids, biologic drugs (mainly TNF-α inhibitors), and bisphosphonates depending on the severity of the disease and the presence of comorbidity and/or complications [36]. Almost all of our patients started treatment with NSAIDs but had to switch to other treatments because of partial response and relapse. Methotrexate was the second most frequent treatment, but six of these seven patients received steroids, bisphosphonates, or biologic drugs at the same time. Thus, it is difficult to assess the real impact of methotrexate. Different biologicals have been used to treat CNO, most commonly TNF-α inhibitors [25]. In our study, remission was achieved more frequently with TNF-α inhibitors, including adalimumab and etanercept. Bisphosphonates given to seven patients, resulted in remission in six patients. One patient experienced worsened bone pain after bisphosphonates, subsequently remitting on an adalimumab and bisphosphonate combination, which achieved a good result. Based on our clinical experiences, long bone lesions in diaphyses are more easily improved than those in epiphyses. It is worth noting that, spinal involvement can lead to fractures and secondary bone deformity [37]. This emphasizes the need for early diagnosis and aggressive treatment to prevent complications. Despite recent advances, there is no information on the optimal duration of treatment. Further studies about treatmnt are needed.
The long-term prognosis of CNO is generally favorable, with remission observed in 40% of patients after 1–5 years of follow-up [38]. In our study, we had a remission rate of 11.7% without medicines in a median follow-up of 16 months. The recurrence of the disease is very common. In a US cohort, a recurrence rate of 83% was observed after a follow-up of 1.8 years [21]. In our study, the recurrent rate was 17.6%. This may be related to the small sample size. It has been reported that patients can present a flare even 15 years after the onset of the disease, so it requires monitoring and long-term follow-up [38].
Conclusion
This study is the first case series of CNO from South China to describe the features and outcomes of such an autoinflammatory bone disease. The diagnosis should include clinical history, laboratory and imaging examination, and histopathological examination. Other causes of chronic bone pain should be ruled out. For treatment, NSAIDs are used as first-line drugs followed by steroids, MTX, SASP, bisphosphonates, and TNF-α inhibitors. Combination therapy with bisphosphonates and TNF-α inhibitors may be an option for refractory CNO. The limitation of this study is its small sample size. Thus, further studies including more patients from other tertiary centers are required to formulate diagnostic and treatment strategies for CNO.
Availability of data and materials
The data and materials used in this study can be made available on request.
Abbreviations
- CNO:
-
Chronic nonbacterial osteomyelitis
- NSAIDs:
-
Non-steroid anti-inflamatory drugs
- MTX:
-
Methotexate
- SASP:
-
Salazosulfadimidine
- CRMO:
-
Chronic recurrent multifocal osteomyelitis
- SAPHO:
-
Synovitis, acne, pustulosis, hyperostosis, and osteitis
- CT:
-
Computed tomography
- ESR:
-
Erythrocyte sedimentation rate
- CRP:
-
C-reactive protein
- HLA:
-
Human leukocyte antigen
- ANA:
-
Antinuclear antibodies
- SSZ:
-
Sulfasalazine
- TNF:
-
Tumor necrosis factor
References
Hedrich CM, Hahn G, Girschick HJ, Morbach H. A clinical and pathomechanistic profile of chronic nonbacterial osteomyelitis/chronic recurrent multifocal osteomyelitis and challenges facing the field. Expert Rev Clin Immunol. 2013;9:845–54.
Stern SM, Ferguson PJ. Autoinflammatory bone diseases. Rheum Dis Clin N Am. 2013;39:735–49.
Borzutzky A, Stern S, Reiff A, et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012;130:e1190–e7.
Giedion A, Holthusen W, Masel L, Vischer D. Subacute and chronic “symmetrical” osteomyelitis. Ann Radiol. 1972;15:329–42.
Bjorksten B, Gustavson KH, Eriksson B, Lindholm A, Nordstrom S. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. J Pediatr. 1978;93:227–31.
Bousvaros A, Marcon M, Treem W, et al. Chronic recurrent multifocal osteomyelitis associated with chronic inflammatory bowel disease in children. Dig Dis Sci. 1999;44:2500–7.
Morbach H, Dick A, Beck C, et al. Association of chronic non-bacterial osteomyelitis with crohn's disease but not with card 15 gene variants. Rheumatol Int. 2010;30:617–21.
Girschick H, Finetti M, Orlando F, et al. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Rheumatology (Oxford). 2018;57:1203–11.
Zhao Y, Ferguson PJ. Chronic nonbacterial osteomyelitis and chronic recurrent multifocal osteomyelitis in children. Pediatr Clin N Am. 2018;65:783–800.
Chamot AM, Benhamou CL, Kahn MF, Beraneck L, Kaplan G, Prost A. Acne pustulosis-hyperostosis- osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic. 1987;54:187–96.
Greenwood S, Leone A, Cassar-Pullicino VN. Sapho and recurrent multifocal osteomyelitis. Radiol Clin N Am. 2017;55:1035–53.
Wipff J, Costantino F, Lemelle I, et al. A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis Rheum. 2015;67:1128–37.
Jansson AF, Grote V. Nonbacterial osteitis in children: data of a German incidence surveillance study. Acta Paediatr. 2011;100:1150–7.
Schnabel A, Range U, Hahn G, Siepmann T, Berner R, Hedrich CM. Unexpectedly high incidences of chronic non-bacterial as compared to bacterial osteomyelitis in children. Rheumatol Int. 2016;36:1737–45.
Jansson A, Renner ED, Ramser J, et al. Classification of non-bacterial osteitis retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology. 2007;46:154–60.
Jansson AF, Müller TH, Leonhard Gliera D. Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum. 2009;60:1152–9.
Rao A, Mallya P, Ranjani S, Raghuram J. Chronic recurrent multifocal osteomyeliti a case series from India. Indian J Orthop. 2018;52:672–7.
Silier CCG, Greschik J, Gesell S, et al. Chronic nonbacterial osteitis from the patient perspective: a health services research through data collected from patient conferences. BMJ Open. 2017;7:e017599.
Concha S, Hernández-Ojeda A, Contreras O, et al. Chronic nonbacterial osteomyelitis in children: a multicenter case series. Rheumatol Int. 2020;40:115–20.
Schnabel A, Range U, Hahn G, et al. Treatment response and long term outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44:1058–65.
Gaal A, Basiaga ML, Zhao Y, Egbert M. Pediatric chronic nonbacterial osteomyelitis of the mandible: Seattle Children’s hospital 22-patient experience. Pediatr Rheumatol. 2020;18:4.
Catalano-Pons C, Comte A, Wipff J, et al. Clinical outcome in children with chronic recurrent multifocal osteomyelitis. Rheumatology (Oxford). 2008;47:1397–9.
Beck C, Morbach H, Beer M, et al. Chronic nonbacterial osteomyelitis in childhood: prospective followup during the first year of anti-inflammatory treatment. Arthritis Res Ther. 2010;12:R74.
Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV. Chronic recurrent multifocal osteomyelitis (CRMO) – advancing the diagnosis. Pediatr Rheumatol Online J. 2016;14:47.
Walsh P, Manners PJ, Vercoe J, Burgner D, Murray KJ. Chronic recurrent multifocal osteomyelitis in children: nine years’ experience at a statewide tertiary paediatric rheumatology referral centre. Rheumatology (Oxford). 2015;54:1688–91.
Girschick HJ, Zimmer C, Klaus G, Darge K, Dick A, Morbach H. Chronic recurrent multifocal osteomyelitis: what is it and how should it be treated? Nat Clin Pract Rheumatol. 2007;3:733–8.
Vittecoq O, Said LA, Michot C, et al. Evolution of chronic recurrent multifocal osteitis toward spondylarthropathy over the long term. Arthritis Rheum. 2000;43:109–19.
Probst FP, Bjorksten B, Gustavson KH. Radiological aspect of chronic recurrent multifocal osteomyelitis. Ann Radiol (Paris). 1978;21:115–25.
Khanna G, Sato TS, Ferguson P. Imaging of chronic recurrent multifocal osteomyelitis. Radiographics. 2009;29:1159–77.
Jurik AG, Egund N. MRI in chronic recurrent multifocal osteomyelitis. Skelet Radiol. 1997;26:230–8.
Ording Müller LS, Humphries P. Commentary on: radiological diagnosis of chronic recurrent multifocal osteomyelitis using whole-body MRI-based lesion distribution patterns. Clin Radiol. 2019;74:737.e1–2.
Morbach H, Schneider P, Schwarz T, et al. Comparison of magnetic resonance imaging and 99mTechnetium-labelled methylene diphosphonate bone scintigraphy in the initial assessment of chronic non-bacterial osteomyelitis of childhood and adolescents. Clin Exp Rheumatol. 2012;30:578–82.
Hofmann SR, Kapplusch F, Girschick HJ. Chronic recurrent multifocal osteomyelitis (CRMO): presentation, pathogenesis, and treatment. Curr Osteoporos Rep. 2017;15:542–54.
Zhao YD, Wu EY, Oliver MS, et al. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal anti-inflammatory drugs and/or with active spinal lesions. Arthritis Care Res. 2018;70:1228–37.
Sułko J, Ebisz M, Bień S, et al. Treatment of chronic recurrent multifocal osteomyelitis with bisphosphonates in children. Jt Bone Spine. 2019;86:783–8.
Kostik Mikhail M, Kopchak O, Chikova I, Isupova EMA. Comparison of diferent treatment approaches of pediatric chronic non-bacterial osteomyelitis. Rheumatol Int. 2019;39:89–96.
Yamashita K, Calderaro C, Labianca L, et al. Chronic recurrent multifocal osteomyelitis (CRMO) involving spine: a case report and literature review. J Orthop Sci. 2021;26:300–5.
Voit AM, Arnoldi AP, Douis H, et al. Whole-body magnetic resonance imaging in chronic recurrent multifocal osteomyelitis: clinical long term assessment may underestimate activity. J Rheumatol. 2015;42:1455–62.
Acknowledgements
We thank Wordvice (www.wordvice.cn) for its linguistic assistance and professor Yongdong Zhao for revise during the preparation of this manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by two National Natural Science Foundations of China (No. 81800438 and 81771762).
Author information
Authors and Affiliations
Contributions
Ma Le, Liu Haimei, Tang Hanyun, Zhang Zhiyong and Zou Lixia are co-first authors and contributed to collect, analysis and interpret the data. Ma Le wrote the manuscript and prepared the figures and tables. Yu Haiguo is corresponding author, and contributed to study conception and design. Yu Haiguo, Sun Li, Li Xiaozhong, Tang Xuemei and Lu Meiping critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a retrospective study, first approved by the Ethics Review Board of Children’s Hospital of Nanjing medical university, the main study center, and then approval was obtained from additional medical centers.
Consent for publication
The authors assign all rights and privileges and give consent for publication of this work to Pediatric Rheumatology.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, L., Liu, H., Tang, H. et al. Clinical characteristics and outcomes of chronic nonbacterial osteomyelitis in children: a multicenter case series. Pediatr Rheumatol 20, 1 (2022). https://doi.org/10.1186/s12969-021-00657-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-021-00657-4