Abstract
Cartilage destruction is a hallmark of osteoarthritis (OA) and is characterized by increased protease activity resulting in the degradation of critical extracellular matrix (ECM) proteins essential for maintaining cartilage integrity. Tenascin-C (TN-C) is an ECM glycoprotein, and its expression is upregulated in OA cartilage. We aimed to investigate the presence of TN-C fragments in arthritic cartilage and establish whether they promote cartilage degradation. Expression of TN-C and its fragments was evaluated in cartilage from subjects undergoing joint replacement surgery for OA and RA compared with normal subjects by western blotting. The localization of TN-C in arthritic cartilage was also established by immunohistochemistry. Recombinant TN-C fragments were then tested to evaluate which regions of TN-C are responsible for cartilage-degrading activity in an ex vivo cartilage explant assay measuring glycosaminoglycan (GAG) release, aggrecanase and matrix metalloproteinase (MMP) activity. We found that specific TN-C fragments are highly upregulated in arthritic cartilage. Recombinant TN-C fragments containing the same regions as those identified from OA cartilage mediate cartilage degradation by the induction of aggrecanase activity. TN-C fragments mapping to the EGF-L and FN type III domains 3–8 of TN-C had the highest levels of aggrecan-degrading ability that was not observed either with full-length TN-C or with other domains of TN-C. TN-C fragments represent a novel mechanism for cartilage degradation in arthritis and may present new therapeutic targets for the inhibition of cartilage degradation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common joint disorder affecting increasing numbers of our ageing populations [1, 2]. Factors contributing to tissue damage include cytokine release, superoxide production and protease activation ultimately leading to loss of joint function [3–6]. Current treatments are largely focused around control of pain and maintenance of function, since there are no effective disease-modifying treatments for OA [7]. There is therefore an unmet need to gain a deeper understanding of the mechanisms underlying joint destruction in OA.
A number of factors influence ongoing cartilage damage in OA, including injurious mechanical compression of cartilage that alters gene transcription of degradative enzymes including MMPs and aggrecanases (ADAMTSs) [8, 9]. Such proteases degrade the key extracellular matrix (ECM) components of cartilage including type II collagen and aggrecan [10, 11]. Several studies have shown increased production of ECM molecules during the early stages of OA [12–14]. Type II collagen, cartilage oligomeric matrix protein (COMP), fibronectin, fibromodulin and tenascin-C are among the ECM proteins that are altered in OA cartilage both at the messenger RNA and protein level. As ongoing protease-mediated cartilage destruction ensues, fragments of ECM proteins are generated, which accumulate during ongoing disease progression.
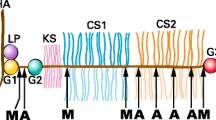
Recent reports suggest that specific ECM proteins become endogenous catabolic factors potentiating further joint damage in OA. Activation of pro-inflammatory pathways by such ECM proteins has led to their description as damage-associated molecular patterns (DAMPs). Several groups have shown that fragments of ECM proteins acquire novel proteolytic activity upon fragmentation that was hitherto absent in the full-length molecule. For example, a fragment of type II collagen localizing to the N-terminus of the molecule upregulates mRNA and protein levels of MMP-2, MMP-3, MMP-9 and MMP-13 in bovine chondrocytes and explants [15]. Other ECM molecules showing distinct activity upon fragmentation include fibromodulin, hyaluronan and fibronectin [16–18]. However, it is unclear whether these are the only protein fragments responsible for further cartilage destruction. Tenascin-C (TN-C) is an ECM glycoprotein associated with tissue injury and repair. TN-C is a hexameric protein of 1.5 million Da comprising an assembly domain, epidermal growth factor-like repeats (EGF-L), fibronectin type III repeats (TNIII) and a fibrinogen-like globe (FBG) [19]. Little TN-C is expressed in normal human joints, but expression is increased in cartilage [20, 21], synovial tissue [22, 23] and synovial fluid [24] in OA and RA. TN-C potentiates chronic inflammation in RA by the upregulation of pro-inflammatory cytokines, and this effect is not observed in TN-C knockout mice [25]. In contrast, in a murine model of OA, TN-C knockout mice showed evidence of delayed healing and repair [26]. The increased levels of TN-C reported in OA tissue and the homology of TN-C domains to other known DAMPs in cartilage prompted us to examine whether TN-C fragments exist in arthritic cartilage and whether TN-C fragments possess novel cartilage-degrading ability.
Materials and methods
Preparation of human cartilage extracts
Human cartilage samples from patients undergoing joint replacement surgery for OA of the knee/hip or normal cartilage obtained from patients undergoing amputations for trauma were obtained with full Ethics Approval (REC reference number: 09/H0806/45) from St George’s and Heatherwood Hospitals NHS Trust. All participants donated tissue with full informed consent. All reagents were obtained from Sigma-Aldrich unless otherwise stated. Human cartilage was washed three times in sterile PBS, and a total of 0.1 g was collected per subject. The cartilage was further dissected in 1 ml of 2 × reducing sample buffer containing 0.2 g SDS, 5 ml upper gel buffer consisting of 84 mM ammediol, 62 mM HCl and 0.02% sodium azide, 1 ml bromophenol blue, 4 ml glycerol and 880 μl of 0.5 M EDTA (pH 8.0) to a final volume of 11 ml. The dissected cartilage and sample buffer were carefully transferred to a 1.5-ml Eppendorf tube and boiled at 100°C for 10 min. The samples were stored at −20°C until further use.
Immunohistochemistry of human cartilage
Fresh cartilage for sectioning was obtained at the time of joint surgery from subjects and immediately fixed in 4% paraformaldehyde in 0.1% phosphate-buffered saline (PBS; pH 7.4) and then sectioned using a cryostat into 7 micron slices onto polylysine-coated glass slides (VWR, Leuven, Belgium). To block endogenous peroxidase activity, 3% H2O2 was applied in the dark for 15 min. Sections were then blocked with 2% goat serum for 30 min. Following this, sections were incubated with an anti-TN-C monoclonal antibody raised against the N-terminal heptad region of TN-C (MAB 1908, Millipore, Watford, UK) at 1:1,000 for 1 h at room temperature, followed by incubation with Dako REAL EnVision detection system/HRP for rabbit/mouse secondary antibodies for 30 min (Dako, Denmark). For control experiments, a mouse IgG primary antibody (SC-2025) (Santa Cruz, Heidelburg, Germany) was used. Signal was developed with the Dako REAL DAB + chromogen substrate system according to the manufacturers’ instructions. Slides were counterstained with haematoxylin and mounted with Histomount (National Diagnostics, Atlanta, USA). All slides were viewed with a Zeiss AXIOPLAN 2 light microscope running on Axiovision system 4.7.
SDS–PAGE and western blotting
Proteins were resolved by SDS/PAGE with reduction using the ammediol/glycine/HCl buffer system of Wyckoff et al. [27] for the Tris–glycine buffer method according to Laemmli [28]. Gels were typically run for 60 min at 200 V.
Staining with Coomassie Brilliant Blue R-250 and silver was performed as previously described [29, 30]. For western blotting, gels were electrotransferred onto a PVDF membrane at 25 V (constant voltage) for 240 min in 200 ml transfer buffer containing 20% v/v methanol, 7.2 g glycine and 1.512 g Tris base. Five percentage BSA was used for blocking, for 30 min following which the primary anti-TN-C antibody in 1% BSA/TBS for 1 h (dilution 1:1,000). The membrane was washed three times with TBS/0.05% Tween. After washing, a 1:5,000 dilution of an AP-linked secondary antibody (Promega, Southampton, UK) in 1% BSA/TBS was added and incubated for 1 h. Membranes were washed three times in TBS/0.05% Tween and incubated with AP substrate for development for up to 30 min.
Tenascin-C and recombinant TN-C proteins
Full-length tenascin-C (Millipore, Watford, UK) was dialysed into TBS buffer (50 mM Tris–HCl, 150 mM NaCl, pH 7.5) before use in cartilage explant cultures. Recombinant TN-C domains were produced as previously described [25]. The Limulus amoebocyte lysate (LAL) assay (Cambrex, Wiesbaden, Germany) was used to test the amount of LPS in all purified and recombinant TN-C proteins as previously described [25]. A standard curve was performed for each experiment using E.coli-derived LPS that was provided in the kit. Detection levels for purified proteins were undetectable in the 1–100 pg/ml range, which is well below the levels required to stimulate cartilage degradation.
Measurement of glycosaminoglycan release, aggrecanase and MMP activity
Fresh porcine metacarpophalangeal joints of 3- to 9-month-old pigs (Turners’, Hampshire, UK) or human tissue were obtained with full Ethical Approval (REC reference number: 09/H0806/45) and dissected into pieces 3 mm × 2–3 mm wide (about 10 mg) as we have previously described [31, 33]. After dissection, cartilage was rested for 48 h at 37°C under 5% CO2 in DMEM containing 5% foetal calf serum, penicillin/streptomycin (100 units/ml), amphotericin B (100 units/ml) and 10 mM HEPES. Each cartilage piece was placed in one well of a round bottom 96-well plate with 200 μl of serum-free medium with full-length TN-C, recombinant TN-C fragments, IL-1α (a gift from Prof J Saklatvala, Imperial College London) as a positive control. Each treatment was performed in triplicate. After 48 h, media and cartilage were harvested and stored at −20°C until use. Each experiment was performed at least 3 times on separate porcine trotters.
The total GAG released into media by cartilage was measured using a modification of the DMMB assay [32]. A volume of 250 μl of the DMMB assay reagent (16 mg/ml DMMB, 41 mM sodium chloride, 40 mM glycine, 9.5 mM HCl) was added to 2.5 μl of culture medium in a 96-well plate, and then the absorbance was read immediately at 540 nm. Each sample was assayed in duplicate. The optical density from the experimental samples was converted into μg of chondroitin from the standard curve.
Aggrecanase and MMP activity in the conditioned medium of treated cartilage was determined using neoepitope assays as previously described [31, 33]. Aggrecanase and MMP-specific neoepitope antibodies anti-ARGSV (BC-3) and anti-FFGVG (BC-14), respectively, were kindly provided by Professor Bruce Caterson and Dr Clare Hughes (University of Wales, Cardiff).
Statistics
The GAG release assay in cartilage explants was evaluated using Graphpad Prism software (San Diego, California). Mean values were calculated for each treatment in triplicate and expressed as mean ± standard error of mean. Significance was analysed with two-tailed Student’s t tests and defined as P < 0.05.
Results
Full-length TN-C and TN-C fragments are upregulated in arthritic cartilage
We analysed the expression of full-length TN-C and its fragments in normal human and arthritic cartilage. TN-C protein was detected in its full-length form at ~170 and ~240 kDa, representing the known short and long forms of TN-C (Fig. 1a). In contrast to normal cartilage, levels of full-length TN-C expression were highly upregulated in cartilage extracts from OA and RA cartilage (lanes 4–12, Fig. 1a). Two additional forms of TN-C were increased in OA and RA samples and detected at ~100 and ~150 kDa. The results represent true comparisons of equal amounts of protein since equivalent gels as those used for western blotting were stained with Coomassie Brilliant Blue and showed equal protein loading in the specimens (Fig. 1b). These combined results show that increased expression of full-length TN-C and specific TN-C fragments is found in human arthritic cartilage compared with normal tissue.
Western blot analysis of cartilage extracts from patients using an anti-TN-C antibody. A total of 1 μg protein was run per well and membranes developed with alkaline phosphatase (AP) substrate for 1 min each. Sample identification: 1 29 (F), lower leg, amputation; 2 17 (F), lower limb, osteosarcoma; 3 45 (M), lower limb, amputation; 4 72 (M), hip OA; 5 68 (M), hip OA; 6 72 (M), knee OA; 7 75 (F), knee OA; 8 71 (M), hip OA; 9 70 (F), knee OA; 10 66 (F), knee OA; 11 45 (M), hip, RA; 12 69 (F), hip, RA. b Equivalent samples used as in (a) with 1 μg protein per well stained with Coomassie Brilliant Blue
Since the anti-TN-C antibody we used recognizes the N-terminal attachment region of TN-C, we could predict the composition of the TN-C fragments detected in our studies of human arthritic cartilage (Fig. 2). Results show that since the main TN-C fragments we found in cartilage are of molecular weight 100 and 150 kDa, the fragments detected are most likely to comprise of TN-C fragments mapping to the TA + EGF-L + FN type III repeats 1–3 (theoretical molecular mass 97 kDa) and the TA + EGF-L + FN type III repeats 1–8 (theoretical molecular mass 147 kDa).
Domain composition of TN-C fragments identified from arthritic cartilage. Human TN-C has a modular structure with repeating units: the TA attachment (heptad) domain at the N-terminus, 14.5 EGF-L repeats, 8–17 FN type III repeats (conserved type III repeats numbered 1–8 are present in all isoforms with splice variants labelled by their designated letter format) and a fibrinogen (FBG) globe at the C-terminus. The table shows the composition of TN-C fragments isolated from arthritic cartilage in our study
We next confirmed TN-C localization in arthritic cartilage by immunohistochemistry. Our results for TN-C staining in OA cartilage show that TN-C expression was predominantly focused around the superficial and midzones of arthritic human cartilage (Fig. 3). The highest intensity of TN-C staining was detected primarily within chondrocytes and the pericellular matrix of OA cartilage. An isotype control IgG antibody did not show any positive staining, showing that the staining observed in OA cartilage was specific for TN-C.
Distribution of TN-C in human OA cartilage. a–d are images from 2 OA subjects stained with anti-TN-C antibody. e–h are the same OA subjects stained with an isotype control IgG mouse antibody. Zones of cartilage are delineated using the following abbreviations—S superficial, M midzone, D deep zone. Bars indicate section size of 10 μM or 50 μM
Recombinant TN-C fragments induce glycosaminoglycan release and aggrecanase activity in cartilage
Since we detected TN-C fragments in arthritic cartilage, we then evaluated the potential for TN-C fragments to induce cartilage degradation. Recombinant fragments comprising the TN-C attachment (TA) domain, the EGF-like (EGF-L) repeats, TN1-5, TN1-3, TN3-5, TN5-7, TN6-8 and the fibrinogen globe (FBG) were cultured with normal porcine articular cartilage (Fig. 4). Experiments were initially conducted at 1 μM TN-C fragments since this is the active concentration of other ECM DAMPs such as fibronectin fragments that share domain homology with TN-C. The TN-C fragments with greatest statistically significant GAG-releasing activity in porcine articular cartilage were EGF-L, TN3-5, TN5-7, TN6-8 as measured by the DMMB assay (Fig. 4). The TN-C attachment domain, TN1-3 and the FBG globe did not have statistically significant levels of GAG release. In addition, full-length TN-C also showed no evidence of cartilage degradation. We analysed which enzymes were mediating the GAG release observed by the active TN-C fragments. Figure 4 shows that aggrecanase neoepitope activity was induced by TN-C fragments TN6-8, TN5-7, EGF-like repeats and TN3-5 using the anti-ARGSV antibody that was similar to levels induced by IL-1α. These TN-C fragments showed significant aggrecanase activity compared with medium alone and full-length TN-C. The other TN-C fragments showed no significant increase in aggrecanase activity compared with negative controls. When conditioned medium was tested for cleavage by MMPs using the MMP-cleavage-specific antibody anti-FFGVG, no neoepitope signal was detected in TN-C fragment-treated explants, although cleavage was observed in IL-1α-treated conditioned medium.
TN-C fragments induce cartilage degradation in normal articular cartilage. a Recombinant TN-C fragments used for cartilage stimulation were run on SDS–PAGE. All proteins were loaded at 1 μg each and stained with silver. b TN-C fragments at 1 μM were used to stimulate porcine cartilage explants for 2 days. The culture medium was harvested and tested for the presence of GAG using the DMMB dye assay (n = 3). c, d Equal volumes of conditioned media (50 μl) from the experiment shown in b were deglycosylated and western blots performed for aggrecanase-cleaved neoepitopes using the BC-3 antibody (c) and the BC-14 antibody (d). Loading controls were medium alone, c, used as a negative control and IL-1α, which served as a positive control
We then tested the dose–response effect of active recombinant TN-C fragments in normal porcine and human articular cartilage. We found that the active fragments maintained their GAG-releasing activity over the micromolar range, with the most significant activity observed at 0.1 and 1 μM concentrations (Fig. 5a). The GAG release assay showed that the highest levels of cartilage degradation were induced by the EGF-L repeats and TN6-8 in the 0.01–1 μM range. In experiments with normal human articular cartilage (obtained from a 69-year-old subject who underwent joint replacement for a fractured neck of femur), we found that the same TN-C fragments that were active in porcine articular cartilage also had GAG-releasing activity in the micromolar range in normal cartilage (Fig. 5b). It was also noted that differences in total GAG release between experiments in Figs. 4 and 5 were found, which are most likely due to natural variation in glycosaminoglycan release between different cartilage explants.
a Porcine cartilage was stimulated with recombinant TN-C fragments with a concentration range of 0.01–1 μM. After 2 days, conditioned medium was harvested and GAG release measured using the DMMB assay (n = 3). b Normal human cartilage (obtained from a 69-year-old subject with a femoral neck fracture) was stimulated with recombinant TN-C fragments at 1 μM each. Conditioned medium was harvested after 2 days and GAG release measured using the DMMB assay (n = 3)
Discussion
In this study, we have shown that two main forms of fragmented TN-C of 100 kDa and 150 kDa are detectable in arthritic cartilage but not in normal subjects. The TN-C fragments we have detected map to the EGF-L and FN type III 3–8 domains in arthritic human cartilage. Recombinant TN-C fragments comprising the same domains induce GAG release and aggrecanase activity in cartilage in a dose-dependent manner. Although increased TN-C expression has previously been described in arthritic cartilage [20, 21, 34], our study is the first to describe and characterize TN-C fragments in cartilage. Zhen et al. [35] recently showed that human cartilage subjected to digestion with ADAMTS-5 cleaves TN-C peptides that map to the N-terminal TA domain when digested cartilage was analysed by mass spectrometry. It is therefore plausible that the generation of TN-C fragments by proteases such as ADAMTS-5 generates TN-C fragments which then stimulate a positive feedback loop of further cartilage matrix degradation mediated by protease activation including aggrecanases as found in our study.
Work conducted in other tissues has shown that leg ulcer exudates have high levels of TN-C fragments [36] and the EGF-L repeats are increased in blood vessels of subjects undergoing carotid endarterectomy [37]. Specific TN-C fragments have distinct functions: the EGF-L domains influence neuronal migration in development [38, 39] and induce apoptosis in smooth muscle cells [36]. The FN III domains of TN-C are susceptible to proteolytic cleavage [40] and interact with ligands including integrins [41], heparin binding [42] and binding to other ECM molecules including fibronectin [43]. Whereas previous work has shown that full-length TN-C is involved in wound repair in OA [26, 34], our work has shown that when TN-C is cleaved to generate fragmented forms, such TN-C fragments acquire novel proteolytic activity that mediates catabolic pathways in articular cartilage. There are therefore differences between the full-length and fragmented forms of TN-C, which mediate anabolic and catabolic pathways, respectively, in OA models.
Based on our findings and those of other groups, we propose a scheme whereby a balance between anabolic effects and catabolic effects mediated by TN-C fragments and other ECM protein fragments occur in the OA joint (Fig. 6). Future work will be required to establish pathways of activation induced by the active TN-C fragments we have identified. It is possible that TN-C fragments such as those we have identified engage with existing receptors in the OA joint, including syndecans [44], integrins [45] or toll-like receptors [46]. Alternatively, it is possible that specific forms of TN-C may inhibit aggrecanase activity, as described in the case of the C-terminal region of fibronectin with ADAMTS-4 [47].
Abbreviations
- ADAMTS:
-
A disintegrin and metalloproteinase with Thrombospondin-like motifs
- DMMB:
-
Dimethylmethylene blue
- GAG:
-
Glycosaminoglycans
- ECM:
-
Extracellular matrix
- EGF-L:
-
Epidermal growth factor
- FN:
-
Fibronectin
- HGF:
-
Hepatocyte growth factor
- IL-1α:
-
Interleukin-1 alpha
- MMP:
-
Matrix metalloproteinase
- OA:
-
Osteoarthritis
- RA:
-
Rheumatoid arthritis
- TN-C:
-
Tenascin-C
- TNF:
-
Tumour necrosis factor
References
Altman RD (1991) Classification of disease: osteoarthritis. Semin Arthritis Rheum 20:40–47
Nuki G (1999) Osteoarthritis: a problem of joint failure. Z Rheumatol 58:142–147
Mankin HJ, Lippiello L (1971) Biochemical and metabolic abnormalities in articular cartilage from osteoarthritic human hips. J Bone Joint Surg Am 52:424–434
Goldring SR, Goldring MB (2004) The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin Orthop Relat Res 427:S27–S36
Nagase H, Kashiwagi M (2003) Aggrecanases and cartilage matrix degradation. Arthritis Res Ther 5:94–103
Kurz B, Jin M, Patwari P, Cheng DM, Lark MW, Grodzinsky AJ (2001) Biosynthetic response and mechanical properties of articular cartilage after injurious compression. J Orthop Res 19:1140–1146
Hunter DJ (2011) Pharmacologic therapy for osteoarthritis—the era of disease modification. Nat Rev Rheumatol 7(1):13–22
Okada Y (2001) Proteinases and matrix degradation. In: Ruddy S, Harris ED, Sledge C (eds) Kelley’s textbook of rheumatology. Saunders, Philadelphia, pp 55–73
Stanton H, Rogerson FM, East CJ, Golub SB, Lawlor KE, Meeker CT, Little CB, Last K, Farmer PJ, Campbell IK, Fourie AM, Fosang AJ (2005) ADAMTS5 is the major aggrecanase in mouse cartilage in vivo and in vitro. Nature 434:648–652
Lark MW, Bayne EK, Flanagan J, Harper CF, Hoerrner LA, Hutchinson NI, Singer I, Donatelli SA, Weidner JR, Williams HR, Mumford RA, Lohmander LS (1997) Aggrecan degradation in human cartilage. Evidence for both matrix metalloproteinase and aggrecanase activity in normal, osteoarthritic, and rheumatoid joints. J Clin Invest 100:93–106
Dodge GR, Poole AR (1989) Immunohistochemical detection and immunochemical analysis of type II collagen degradation in human normal, rheumatoid, and osteoarthritic articular cartilages and in explants of bovine articular cartilage cultured with interleukin 1. J Clin Invest 83:647–661
Aigner T, Zien A, Gehrsitz A, Gebhard PM, Mckenna L (2001) Anabolic and catabolic gene expression pattern analysis in normal versus osteoarthritic cartilage using complementary DNA-array technology. Arthritis Rheum 44:2777–2789
Lee JH, Fitzgerald JB, Dimicco MA, Grodzinsky AJ (2005) Mechanical injury of cartilage explants causes specific time-dependent changes in chondrocyte gene expression. Arthritis Rheum 52:2386–2395
Loening AM, James IE, Levenston ME, Badger AM, Frank EH, Kurz B, Nuttall ME, Hung HH, Blake SM, Grodzinsky AJ, Lark MW (2000) Injurious mechanical compression of bovine articular cartilage induces chondrocyte apoptosis. Arch Biochem Biophys 381:205–212
Fichter M, Korner U, Schomburg J, Jennings L, Cole AA, Mollenhauer J (2006) Collagen degradation products modulate matrix metalloproteinase expression in cultured articular chondrocytes. J Orthop Res 24(1):63–70
Heathfield TF, Onnerfjord P, Dahlberg L, Heinegard D (2004) Cleavage of fibromodulin in cartilage explants involves removal of the N-terminal tyrosine sulfate-rich region by proteolysis at a site that is sensitive to matrix metalloproteinase-13. J Biol Chem 279(8):6286–6295
Homandberg GA, Meyers R, Xie DL (1992) Fibronectin fragments cause chondrolysis of bovine articular cartilage slices in culture. J Biol Chem 267:3597–3604
Knudson W, Casey B, Nishida Y, Eger W, Kuettner KE, Knudson CB (2000) Hyaluronan oligosaccharides perturb cartilage matrix homeostasis and induce chondrocytic chondrolysis. Arthritis Rheum 43:1165–1174
Jones PL, Jones FS (2000) Tenascin-C in development and disease: gene regulation and cell function. Matrix Biol 19:581–596
Salter DM (1993) Tenascin is increased in cartilage and synovium from arthritic knees. Br J Rheumatol 32:780–786
Chevalier X, Groult N, Larget Piet B, Zardi L, Hornebeck W (1994) Tenascin distribution in articular cartilage from normal subjects and from patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum 37(7):1013–1022
Cutolo M, Picasso M, Ponassi M, Sun MZ, Balza E (1992) Tenascin and fibronectin distribution in human normal and pathologic synovium. J Rheumatol 19:1439–1447
McCachren SS, Lightner VA (1992) Expression of human tenascin in synovitis and its regulation by interleukin-1. Arthritis Rheumatism 35:1185–1196
Hasegawa M, Nakoshi Y, Muraki M, Sudo A, Kinoshita N, Yoshida T, Uchida A (2007) Expression of large tenascin-c splice variants in synovial fluid of patients with rheumatoid arthritis. J Orthop Res 25:563–568
Midwood K, Sacre S, Piccinini AM, Inglis J, Trebaul A, Chan E, Drexler S, Sofat N, Kashiwagi M, Orend G, Brennan F, Foxwell B (2009) Tenascin-C is an endogenous activator of Toll-like receptor 4 that is essential for maintaining inflammation in arthritic joint disease. Nat Med 15(7):774–781
Okamura N, Hasegawa M, Nakoshi Y, Iino T, Sudo A, Imanaka-Yoshida K, Yoshida T, Uchida A (2010) Deficiency of tenascin-C delays articular cartilage repair in mice. Osteoarthr Cartilage 18(6):839–848
Wykcoff D, Rodbard A, Chrambach A (1977) Polyacrylamide gel electrophoresis in sodium dodecyl sulfate-containing buffers using multiphasic buffer systems: properties of the stack, valid Rf-measurement, and optimized procedure. Anal Biochem 78:459–482
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680–685
Meyer TS, Lambert BL (1965) Use of Coomassie brilliant blue R250 for the electrophoresis of microgram quantities of parotid saliva proteins on acrylamide-gel strips. Biochim Biophys Acta 107:144–145
Shevchenko A, Wilm M, Vorm O, Mann M (1980) Mass spectrometric sequencing of proteins silver stained polyacrylamide gels. Anal Chem 68:850–858
Gendron C, Kashiwagi M, Hughes C, Caterson B, Nagase H (2003) TIMP-3 inhibits aggrecanase-mediated glycosaminoglycan release from cartilage explants stimulated by catabolic factors. FEBS Lett 555:431–436
Farndale RW, Buttle DJ, Barrett AJ (1986) Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta 883:173–177
Sofat N (2009) Analysing the role of endogenous matrix molecules in the development of osteoarthritis. Int J Exp Pathol 90:463–479
Nakoshi Y, Hasegawa M, Akeda K, Iino T, Sudo A, Yoshida T, Uchida A (2010) Distribution and role of tenascin-C in human osteoarthritic cartilage. J Orthop Sci 15(5):666–673
Zhen EY, Brittain IJ, Laska DA, Mitchell PG, Sumer EU, Karsdal MA, Duffen KL (2008) Characterization of metalloproteinase cleavage products of human articular cartilage. Arthritis Rheum 58(8):2420–2431
Latijnhouwers MAHE, Bergers M, Veenhuis RT, Beekman B, Ankersmit-Ter Horst MFP, Schalkwijk J (1998) Tenascin-C degradation in chronic wounds is dependent on serine proteinase activity. Arch Dermatol Res 290:490–496
Wallner K, Li C, Shah PK, Wu K-J, Schwartz SM, Sharifi BG (2004) EGF-like domain of tenascin-C is proapoptotic for cultured smooth muscle cells. Arterioscler Thromb Vasc Biol 24:1416–1421
Prieto AL, Andersson-Fissone C, Crossin KL (1992) Characterization of multiple adhesive and counteradhesive domains in the extracellular matrix protein cytotactin. J Cell Biol 111:685–698
Spring J, Beck K, Chiquet-Ehrisman R (1989) Two contrary functions of tenascin: dissection of the active sites by recombinant tenascin fragments. Cell 59:325–334
Siri A, Knauper V, Veirana N, Caocci F, Murphy G, Zardi L (1995) Different susceptibility of small and large human tenascin-C isoforms to degradation by matrix metalloproteinases. J Biol Chem 270:8650–8654
Spring J, Beck K, Chiquet-Ehrisman R (1989) Two contrary functions of tenascin: dissection of the active sites by recombinant tenascin fragments. Cell 59:325–334
Weber P, Zimmerman DR, Winterhalter KH, Vaughan L (1995) Tenascin-C binds heparin by its fibronectin type III domain five. J Biol Chem 270:4619–4623
Day JM, Olin AI, Murdoch AD, Canfield A, Sasaki T, Timpl R, Hardingham TE, Aspberg A (2004) Alternative splicing in the aggrecan G3 domain influences binding interactions with tenascin-C and other extracellular matrix proteins. J Biol Chem 279:12511–12518
Echtermeyer F, Betrand J, Dreier R et al (2009) Syndecan-4 regulates ADAMTS-5 activation and cartilage breakdown in osteoarthritis. Nat Med 15(9):1072–1076
Salter DM, Hughes DE, Simpson R, Gardner DL (1992) Integrin expression by human articular chondrocytes. Br J Rheumatol 31:231–234
Zhang Q, Hui W, Litherland GJ et al (2008) Differential Toll-like receptor-dependent collagenase expression in chondrocytes. Ann Rheum Dis 67(11):1633–1641
Hashimoto G, Shimoda M, Okada Y (2004) ADAMTS4 (aggrecanase-1) interaction with the COOH-terminal domain of fibronectin inhibits proteolysis of aggrecan. J Biol Chem 279:32483–32491
Acknowledgments
This work was funded by a Clinical Research Training Fellowship from The Wellcome Trust to Dr Nidhi Sofat, grant code 070848 and an Enterprise Award from St George’s, University of London. We thank Professor Bruce Caterson and Dr Clare Hughes (Cardiff University) for BC-3 and BC-14 antibodies. We thank Dr Kim Midwood (Imperial College London) for recombinant tenascin-C proteins and Professor Hideaki Nagase for useful discussions. We thank Miss Kinga Anita Szewczyk, Mr Ray Moss and Miss Kay Elderfield for assistance with immunohistochemistry (St George’s, University of London).
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Sofat, N., Robertson, S.D., Hermansson, M. et al. Tenascin-C fragments are endogenous inducers of cartilage matrix degradation. Rheumatol Int 32, 2809–2817 (2012). https://doi.org/10.1007/s00296-011-2067-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-011-2067-8