Abstract
To determine the significance of CD13/aminopeptidase N in collagen vascular diseases (CVD), we examined its activity and expression in sera and disease sites of patients with CVD. Significantly higher aminopeptidase activity was detected in bronchoalveolar lavage fluid from patients with interstitial lung diseases due to rheumatoid arthritis (RA), polymyositis/dermatomyositis (PM/DM), systemic sclerosis (SSc), and Sjögren's syndrome than from control subjects. Increased aminopeptidase activity and increased expression of CD13/aminopeptidase N protein were found in alveolar macrophages from CVD patients with interstitial lung diseases. Significantly higher aminopeptidase activity was detected in pleural effusions from patients with systemic lupus erythematosus (SLE) than in transudate effusions. The mean aminopeptidase activity in synovial fluids from RA patients was significantly higher than from patients with osteoarthritis. The mean value of serum aminopeptidase activity was significantly higher in patients with SLE, RA, SSc, and PM/DM than in normal subjects. This study suggests that the activity of CD13/aminopeptidase N, locally produced in the disease site, is a useful marker for CVD and that CD13/aminopeptidase N may have an important role in the pathogenesis of CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aminopeptidase N is a membrane-bound metalloprotease shown to be identical to CD13 [1], a 150-kDa cell surface glycoprotein which was originally used as a marker for subpopulations of hematopoietic cells [2]. CD13/aminopeptidase N is widely distributed in a variety of mammalian cells such as monocytes/macrophages, fibroblasts, neutrophils, endothelial cells, and epithelial cells [3, 4, 5, 6]. CD13/aminopeptidase N is the major receptor for human coronavirus [7] and gastroenteritis virus [8] and has an important role in HIV entry [9]. This peptidase was shown to be involved in the degradation of extracellular matrix in tumor invasions [10, 11] and the processing of peptide for presentation by antigen-presenting cells [12]. Recently we reported that CD13/aminopeptidase N has the chemotactic activity of T lymphocytes in vitro [13].
Collagen vascular diseases (CVD) are inflammatory, autoimmune disorders which affect skin, joints, serous membranes, and a variety of internal organs such as lungs, kidneys, and heart [14]. Although their origin has been shown to be multifactorial and involves complex interactions between genetic, environmental, and hormonal factors [15, 16, 17], the precise mechanism of organ inflammations in CVD is still unclear. In this study, we examined the activity of CD13/aminopeptidase N in patients with CVD and found increased activity and expression of it at the disease site and in serum, suggesting an important role in the pathogenesis of CVD.
Materials and methods
Reagents
L-leucine-7-amido-4-methyl-coumarine (L-leucine-AMC) was purchased from the Peptide Institute (Osaka, Japan). Monoclonal antibody against human CD13 was purchased from Becton Dickinson (San Jose, Calif., USA).
Serum Sampling
Serum was collected from 61 patients with CVD (Table 1). The diagnosis of CVD was based on American College of Rheumatology criteria. The CVD patients included 17 with systemic lupus erythematosus (SLE), 21 with rheumatoid arthritis (RA), ten with systemic sclerosis (SSc), eight with polymyositis/dermatomyositis (PM/DM), and five with Sjögren's syndrome (SjS). Normal volunteers consisted of seven young doctors, none of whom showed any abnormalities on physical examination or chest radiography. Control patients were free of collagen vascular diseases; four had mild pulmonary emphysema, three had diabetes mellitus, and three had inactive gastric ulcers.
Bronchoalveolar lavage
Bronchoalveolar lavage (BAL) was performed for patients with CVD with interstitial pneumonia (CVD-IP) and control subjects. These patients consisted of eight RA (three men, 57.7±5.1 years old), six SSc (two men, 51.3±3.9 years old), six PM/DM (two men, age 48.8±3.5 years), and eight SjS patients (one man, age 62.0±5.3 years). The controls consisted of 15 normal volunteers (13 men, age 22.8±1.0 years) and 13 control patients (nine men, age 56.0±5.1 years). None of the normal volunteers showed any abnormalities on physical examination, chest radiography, or lung function tests. All control patients were free of interstitial lung disease; 11 had localized lung cancer and two had no detectable lesion in the lungs, although they complained of hemosputum. The BAL was performed as described previously [18]. Briefly, a flexible fiber-optic Model 1T20 bronchoscope (Olympus, Tokyo, Japan) was wedged into a segmental or subsegmental bronchus of the middle lobe or lingula, and lavage was performed with a total volume of 150 ml of sterile 0.9% saline in three 50-ml portions. The lavage fluid was gently aspirated by syringe after deep inspiration. The fluid recovered was passed through sterile gauze and centrifuged at 250 G for 10 min at 4°C to precipitate cells, and the supernatant (BAL fluid, or BALF) was stored at −70°C until examination.
Preparation of alveolar macrophages
The precipitated cells were analyzed. Their total numbers, suspended in an appropriate volume of saline, were counted in a hemocytometer. Differential counts on 500 cells were carried out on smears of sedimented cells stained with May-Giemsa stain, and the percentages of alveolar macrophages (AM), lymphocytes, neutrophils, and eosinophils were calculated. The cells were suspended in RPMI-1640 medium and plated into 96-multiwell plates (C8) (White Maxisorp, Nunc, Denmark) (AM density 104 cells/well). After 1 h incubation in 5% CO2 at 37°C, nonadherent cells were removed by gentle washing. Then the aminopeptidase activity on the adherent AM was measured as described below.
Sampling of pleural effusions
Pleural effusions was collected via diagnostic thoracentesis. Patients consisted of five with SLE (one man, age 59.4±5.4 years), 51 with pleuritis carcinomatosa, 24 with infectious pleuritis, and 14 with transudate pleural effusion (ten men, age 67.7±2.3 years). All pleuritis carcinomatosa was due to primary lung cancer in 31 adenocarcinoma patients (20 men, age 62.9±2.1 years), ten squamous cell carcinoma patients (seven men, age 71.9±4.0 years), and ten small cell lung cancer patients (eight men, age 64.7±3.3 years). Infectious pleuritis included 15 nontuberculous pleuritis (13 men, age 66.5±1.9 years) and nine tuberculous pleuritis patients (six men, age 55.3±4.8 years). After centrifugation at 400 G for 10 min, the cell-free supernatants were separated and stored at −70°C until examination.
Sampling of synovial fluids
Studies were done on 33 patients with RA (nine men, age 61.9±6.2 years) and eight with osteoarthritis (OA) (five men, age 71.8±4.4 years). These patients fulfilled the American Rheumatoid Association criteria for the diagnosis of definite or classic RA [19]. Synovial fluid samples were obtained from the swollen joints of patients and centrifuged at 250 G for 30 min. The supernatants were stored at −20°C until testing.
Determination of protease activity of aminopeptidase
The protease activity of aminopeptidase was assayed fluorometrically as described previously [13, 20]. In brief, 80 μl of 0.1 M Tris-HCL buffer (pH 8.0), 100 μl of 100-μM L-leucine-AMC diluted with the buffer, and 20-μl samples were added into the wells of 96-multiwell plates (C8) (White Maxisorp, Nunc, Denmark). The standard contained various amounts of AMC. The plates were incubated at 37°C for 1 h. The fluorescence intensity was measured in MTP-32 (Corona Electric, Ibaragi, Japan) with 365 nm for excitation and 450 nm for emission wavelengths. The aminopeptidase activity is expressed in nanomoles of substrate cleaved per h.
Western blotting
The BAL cells dissolved in RPMI-1640 (Nissui, Tokyo, Japan) were incubated in Falcon 3003 tissue culture dishes (Falcon Plastics, Oxnard, Calif., USA) at 37°C in a humidified atmosphere of 5% CO2 for 60 min, and the plates were washed three times with PBS to remove nonadherent cells. Adherent AM were scraped from the plates using a cell scraper (Sumitomo Bakelite, Osaka, Japan) and sonicated twice at 20 kHz for 5 s. The resulting cell lysates were mixed with an equal volume of loading buffer (125 mM Tris-HCl [6.8], 4% sodium dodecyl sulfate [SDS], 2 mg/ml methyl green, and 10% glycerol). Fifty micrograms of protein were subjected to 10% polyacrylamide gel electrophoresis in SDS running buffer (25 mM Tris-HCl [pH 8.3]), 192 mM glycine, and 0.1% SDS). After electrophoresis, the protein bands were transferred to an Immobilon-P membrane (Millipore, Bedford, Mass., USA) in a buffer containing 25 mM Tris (pH 8.3), 192 mM glycine, 0.1% SDS, and 20% methanol. The blots were pretreated with 1% skim milk and incubated with antihuman CD13 antibody as primary antibody and biotinylated antimurine IgG as secondary antibody. The reacted proteins were visualized using a Vectastain ABC kit (Vector, Burlingame, Calif., USA) according to the manufacturer's instructions. Phosphate-buffered solution containing 0.05% Tween 20 was used as a washing buffer throughout the blotting experiments.
Statistical analysis
All results were expressed as mean±SEM. Statistical analysis was performed using Student's two-tailed unpaired t-test for comparisons between two groups. Correlations between two parameters were evaluated using Pearson's test. Differences were considered significant if P values were 0.05 or less. Data were analyzed on a Macintosh computer using Statview software.
Results
Aminopeptidase activity in bronchoalveolar lavage fluid
Aminopeptidase activity was measured in the BALF from patients with CVD and compared with that from normal volunteers and control patients. The CVD patients consisted of eight with RA, six with SSc, six with PM/DM, and eight with SjS, all of them having interstitial lung disease due to CVD. Very low aminopeptidase activity was detected in the BALF from normal volunteers and control patients (18.8±7.5 nmol/h and 10.2±4.0 nmol/h, respectively) (Fig. 1). On the other hand, it was significantly higher in patients with RA, SSc, PM/DM, and SjS, but there was no significant difference between these disease groups.
Aminopeptidase activity in the BALF from normal volunteers (NV), control patients (CP), and patients with CVD. The activity was assayed fluorometrically with L-leucine-AMC as a substrate and expressed in nanomoles of substrate cleaved per h. *Significantly different from the values of normal volunteers and Control patients (P<0.05)
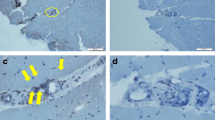
Aminopeptidase activity and expression of CD13/aminopeptidase N in AM
CD13/aminopeptidase N is an ectoenzyme located in the outer cell membranes of various cells such as monocytes/macrophages. To determine the cellular origin of aminopeptidase in BALF, aminopeptidase activity on AM from patients with CVD-IP was measured, because the predominant cells in alveolar space are AM. As shown in Fig. 2, significantly increased aminopeptidase activity was found on AM from patients with CVD-IP than in normal volunteers. Next, the expression of CD13/aminopeptidase N protein in AM was determined by Western blotting, documented in Fig. 3. When 50 μg of AM lysate protein was separated on SDS polyacrylamide gel electrophoresis (SDS-PAGE), CD13/aminopeptidase N protein, with a molecular mass of approximately 150 kD, was detected in normal volunteers at very low levels. On the other hand, the AM lysate protein from nine patients with CVD-IP contained higher amounts of CD13 corresponding to the aminopeptidase activity in the BALF and on AM (Fig. 3).
Aminopeptidase activity on AM from normal volunteers (n=4) and patients with CVD-IP (n=9). The AM suspended in RPMI-1640 were plated into 96-multiwell plates (AM density 104 cells/well), and the activity was assayed fluorometrically with L-leucine-AMC as a substrate and was expressed in nanomoles of substrate cleaved per h. *Significantly different from the value of normal volunteers (P<0.05)
Western blot analysis of CD13/aminopeptidase N protein expression in AM. Fifty micrograms of AM lysate protein were separated on SDS polyacrylamide gel and blotted. CD13/aminopeptidase N was detected by a monoclonal antihuman CD13/aminopeptidase N antibody. Lanes 1–4 contain lysates of AM from normal volunteers, and lanes 5–13 contain those from patients with CVD-IP (lane 5–7 RA, lane 8 DM, lane 9 PM, lane 10–12 SSc, lane 13 SjS). Aminopeptidase activity in BALF and AM was assayed fluorometrically with L-leucine-AMC as a substrate
Aminopeptidase activity in pleural effusion
The level of aminopeptidase activity in pleural effusion was measured in patients with SLE (Fig. 4) and found to be significantly higher than in transudate effusion due to adenocarcinoma and small-cell lung cancer but not to squamous cell carcinoma or infectious diseases. In pleural effusion of SLE patients, it was also significantly higher than that in nontuberculous infection, adenocarcinoma, squamous cell carcinoma, and small cell lung cancer (P=0.0003, P=0.0012, P=0.0053, and P=0.0294, respectively)
Aminopeptidase activity in pleural effusions from patients with transudate effusion, tuberculosis (TB), non-TB, lung cancer and patients with SLE. The activity was assayed fluorometrically with L-leucine-AMC as a substrate and expressed in nanomoles of substrate cleaved per h. *Significantly different from the value of normal volunteers (P<0.05)
Aminopeptidase activity in synovial fluid
Aminopeptidase activity in the synovial fluid from 33 patients with RA and eight with OA is shown in Table 2. It was low in synovial fluid of OA patients. The mean value in the synovial fluid of RA patients was significantly higher than in those with OA. It correlated significantly with the number of lymphocytes in synovial fluid (r=0.85, P=0.0001).
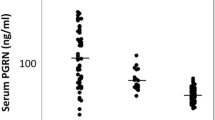
Serum aminopeptidase activity
Aminopeptidase activity in sera from normal subjects and patients with CVD is shown in Fig. 5. It was low in the sera of normal volunteers and control patients (77.0±4.1 nmol/h, 82.9±9.2 nmol/h). The mean activity in sera from patients with SLE, RA, SSc, and PM/DM was significantly higher (133.1±13.0, 115.7±5.7, 120.2±9.1, and 147.1±15.6 nmol/h, respectively) than that of normal volunteers and control patients, but individual values varied widely.
Aminopeptidase activity in sera of normal volunteers, control patients, and patients with CVD. The activity was assayed fluorometrically with L-leucine-AMC as a substrate and expressed in nanomoles of substrate cleaved per h. *Significantly different from the value of normal volunteers and control patients (P<0.05)
Discussion
Here we showed increased aminopeptidase activity in samples from disease sites such as BALF, pleural effusion, and synovial fluid of patients with CVD. The aminopeptidase family mainly consists of leucine aminopeptidase (E.C.3.4.11.1), CD13/aminopeptidase N (E.C.3.4.11.2), and cystyl aminopeptidase (E.C.3.4.11.3) [21, 22]. L-leucine-AMC, which was used in this study as a substrate to detect the aminopeptidase activity, could be cleaved by leucine aminopeptidase and CD13/aminopeptidase N but not by cystyl aminopeptidase [21]. Additionally, cystyl aminopeptidase is mainly localized in placental lysosomes [21]. Leucine aminopeptidase is generally located in liver and has an optimal pH degree of 10. On the other hand, CD13/aminopeptidase N was located in all tissues studied, in which the optimal pH is neutral (pH 6.5–8.5) [24]. These findings indicate that increased aminopeptidase activity in the disease site of CVD may be predominantly composed of CD13/aminopeptidase N.
The BALF from patients with CVD-IP contained higher aminopeptidase activity than that from control subjects. Activated macrophages have an important role in initiating and amplifying immunologic and inflammatory responses in various inflammatory lung diseases including CVD-IP [23, 24]. CD13/aminopeptidase N expressed in macrophages was shown to be an ectoenzyme marker that increases as macrophages mature or become activated [4]. In this study, increased activity and expression of CD13/aminopeptidase N protein were found in AM from patients with CVD-IP, indicating that AM may be responsible for the aminopeptidase activity detected in the BALF from CVD-IP patients. However, CD13/aminopeptidase N has also been reported to be expressed in fibroblasts, neutrophils, and endothelial cells [3, 4, 5, 6, 25, 26]. Further studies are necessary to determine the cells responsible for aminopeptidase in BALF.
Significantly increased activity of aminopeptidase was found in pleural effusion due to SLE than in transudate effusion, indicating that aminopeptidase was locally produced in pleural space and has a role in pleuritis in SLE. A higher aminopeptidase activity was also detected in pleural effusion due to adenocarcinoma and small cell carcinoma, though it was significantly lower than in SLE patients. This result corresponds to previous reports which show that CD13/aminopeptidase N expressed on cancer cells is involved in tumor cell invasion and extracellular matrix degradation [10, 11, 27].
Higher aminopeptidase activity was detected in synovial fluid of RA patients than in OA patients. CD13/aminopeptidase N is expressed on a variety of cells such as macrophages [4]. It is not expressed in peripheral blood lymphocytes but was shown to be expressed in synovial fluid lymphocytes [28]. Further studies are necessary to clarify the cellular origin of CD13/aminopeptidase N in synovial fluids of RA patients.
We showed significantly higher aminopeptidase activity in sera from patients with CVD than in normal volunteers and control patients. Favaloro et al. showed that serum aminopeptidase activity could mainly be ascribed to CD13/aminopeptidase N [29]. We recently reported that increased aminopeptidase activity was detected in BALF from patients with pulmonary sarcoidosis, but its serum level was not higher than in normal controls [13]. Therefore, the increased aminopeptidase detected in serum from CVD patients may represent the total activity of CD13/aminopeptidase N of general CVD lesions in the body and is possibly a useful marker of CVD disease activity.
The role of CD13/aminopeptidase N remains unclear. We recently found that CD13/aminopeptidase N is a chemoattractant for T lymphocytes, and the enzymatic activity was required for T-cell chemotactic activity because its inhibition resulted in the abolishment of chemotactic activity [13]. These results suggest that enzymatically active CD13/aminopeptidase N has a role in the migration of T lymphocytes to the disease site of CVD. On the other hand, CD13/aminopeptidase N is known to be present on cell surface as the membrane-bound enzyme and can cleave N-terminal amino acids from oligopeptides [1]. Recent reports demonstrated increased aminopeptidase activity in urine from patients with diabetic nephropathy [30] and carboplatin-induced renal damage [31] and those treated with extracorporeal shock wave lithotripsy [32]. This activity correlated with the extent of renal damage. Accordingly, the proteolytic activity of CD13/aminopeptidase N may induce the degradation of structural proteins, which results in tissue inflammation in CVD.
The data presented here indicate that CD13/aminopeptidase N activity may serve as a marker of diagnosis and activity of CVD and suggest that CD13/aminopeptidase N may participate in the mechanism of tissue inflammation in this disorder. A greater understanding of the regulation of production and action of this enzyme may lead to new insights for the control and treatment of CVD.
References
Look AT, Ashmun RA, Shapiro LH, Peiper SC (1989) Human myeloid plasma membrane glycoprotein CD13 (gp150) is identical to aminopeptidase. N J Clin Invest 83:1299–1307
Shipp MA, Look T (1993) Hematopoietic differentiation antigens that are membrane-associated enzymes: cutting is the key. Blood 82:1052–1070
Harris CA, Hunte B, Krauss MR, Taylor A, Epstein LB (1992) Induction of leucine aminopeptidase by interferon-gamma. J Biol Chem 267:6865–6869
Turek JJ, Robinson JP (1994) Leucine aminopeptidase activity by flow cytometry. Methods Cell Biol 41:461–467
Raynaud F, Bauvouis B, Gerbaud P, Evain-Brion (1992) Characterization of specific proteases associated with the surface of human skin fibroblasts, and their modulation in pathology. J Cell Physiol 151:378–385
Piela-Smith TH, Korn JH (1995) Aminopeptidase N: a constitutive cell-surface protein on human dermal fibroblasts. Cell Immunol 162:42–48
Yeager CL, Ashmun RA, Williams RK, Cardellichio CB, Shapiro LH, Look AT (1992) Human aminopeptidase is a receptor for human corona virus 229E. Nature 357:420–422
Delmas B, Gelfi J, L'Haridon R, Vogel LK, Sjostrom H, Noren O (1992) Aminopeptidase N is a major receptor for the enteropathogenic coronavirus TGEV. Nature 357:417–420
Pulido-Cejudo G, Conway B, Proulx P, Brown R, Izaguirre CA (1997) Bestatin-mediated inhibition of leucine aminopeptidase may hide HIV infection. Antiviral Res 36:167–177
Saiki I, Fujii H, Yoneda J, Abe F, Nakajima M, Tsuruo T (1993) Role of aminopeptidase N (CD13) in tumor-cell invasion and extracellular matrix degradation. Int J Cancer 54:137–43
Ino K, Goto S, Okamoto T, Nomura S, Nawa A, Isobe K (1994) Expression of aminopeptidase N on human choriocarcinoma cells and cell growth suppression by the inhibition of aminopeptidase N activity. Jpn J Cancer Res 85:927–933
Hansen AS, Noren O, Sjostrom H, Werdelin O (1993) A mouse aminopeptidase N is a marker for antigen-presenting cells and appears to be co-expressed with major histocompatibility complex class II molecules. Eur J Immunol 23:2358–2364
Tani K, Ogushi F, Huang L, Kawano T, Tada H, Sone S (2000) CD13/aminopeptidase N, a novel chemoattractant for T lymphocytes in pulmonary sarcoidosis. Am J Respir Crit Care Med 161:1636–1642
Calen JP, Tuffanelli DL, Provost TT (1993) Collagen-vascular disease: an update. J Am Acad Dermatol 28:477–484
Vyse TJ, Kotzin BL (1998) Genetic susceptibility to systemic lupus erythematosus. Annu Rev Immunol 16:261–292
Plotz PH (1995) Myositis—immunologic contribution to understanding cause, pathogenesis, and therapy. Ann Intern Med 122,715–724
Wiedeman HP, Matthay RA (1989) Pulmonary manifestation of collagen vascular disease. Clin Chest Med 10:677–621
Yano S, Yanagawa H, Nishioka Y, Mukaida N, Matsushima K, Sone S (1996) T helper 2 cytokines differently regulate monocyte chemoattractant protein-1 production by human peripheral blood monocytes and alveolar macrophages. J Immunol 157:2660–2665
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Tani K, Yasuoka S, Ogushi F, Asada K, Fujisawa K, Ozaki T, Ogura T (1991) Thrombin enhances lung fibroblast proliferation in bleomycin-induced pulmonary fibrosis. Am J Respir Cell Mol Biol 5:34–40
Sanderink G-J, Artur Y, Siest G (1988) Human aminopeptidases: a review of the literature. J Clin Chem Clin Biochem 26:795–807
Mendz GL, McCall MN, Kuchel PW (1989) Characterization of leukocyte enzyme involved in the release of amino acids in incubated blood cell lysates. J Biol Chem 264:2108–2117
Sibille Y, Reynolds HY (1990) Macrophages and polymorphonuclear neutrophils in lung defense and injury. Am Rev Respir Dis 141:471–501
Thornton SC, Robbins JM, Penny R (1992) Fibroblast growth factors in connective tissue disease associated interstitial lung disease. Clin Exp Immunol 90:447–452
Favaloro EJ (1991) CD-13 (gp150;aminopeptidase-N): co-expression on endothelial and haemopoietic cells with conservation of functional activity. Immunol Cell Biol 69:253–260
Smith GP, MacGregor RR, Peters TJ (1983) Subcellular localization of leucine aminopeptidase in human polymorphonuclear leukocytes. Biochim Biophys Acta 728:222–227
Mahoney KH, Miller BE, Heppner GH (1985) FACS quantitation of leucine m aminopeptidase and acid phosphatase on tumor-associated macrophages from metastatic and nonmetastatic mouse mammary tumors. J Leukoc Biol 38:573–585
Riemann D, Schwachula A, Hentschel M, Langner J (1993) Demonstration of CD13/aminopeptidase N on synovial fluid T cells from patients with different forms of joint effusions. Immunobiology 187:24–35
Favaloro EJ, Browning T, Nandurkar H (1993) The hepatobiliary disease marker serum alanine aminopeptidase predominantly comprises an isoform of the haematological myeloid differentiation antigen and leukaemia marker CD13/gp150. Clin Chim Acta 220:81–90
Bedir A, Ozener IC, Emerk K (1996) Urinary leucine aminopeptidase is a more sensitive indicator of early damage in non-insulin-dependent diabetics than microalbuminuria. Nephron 74:110–113
Metz-Kurschel U, Kurschel E, Niederle N, Aulbert E (1990) Investigations on the acute and chronic nephrotoxicity of the new platinum analogue carboplatin. J Cancer Res Clin Oncol 116:203–206
Sarica K, Suzer O, Yaman O, Kupeli B, Baltaci S, Bilaloglu E (1996) Leucine aminopeptidase enzymuria: quantification of renal tubular damage following extracorporeal shock wave lithotripsy. Intern Urol Nephrol 28:621–626
Acknowledgements
This work was supported in part by a grant-in-aid for general scientific research (C) from the Ministry of Education, Science, and Culture and the Ministry of Health and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dan, H., Tani, K., Hase, K. et al. CD13/aminopeptidase N in collagen vascular diseases. Rheumatol Int 23, 271–276 (2003). https://doi.org/10.1007/s00296-003-0292-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-003-0292-5