Abstract
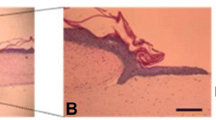
In the present study, neonate keratinocytes were cocultured with human adipose-derived mesenchymal stem cells (hAMSCs) on the electrospun polycaprolactone-platelet gel (PCL–PG) scaffold. To evaluate its potential of wound healing and skin tissue engineering, neonate keratinocytes must be differentiated. The PCL scaffold prepared by the electrospinning technique was fabricated and coated by PG. Then scaffolds were fully characterized by SEM, contact angle, FTIR–ATR, and tensile test. Following seeding hAMSCs as a feeder layer, neonate keratinocytes were cocultured directly on PCL–PG scaffolds and neat PCL. The hAMSCs and neonate keratinocytes' viability was measured using MTT assay for up to 10 days (1st, 3rd, 5th, 7th, and 10th days). To examine the epidermal maturation, cytokeratin 10 and loricrin determinants detection was used through immunocytochemistry (ICC). In addition, real-time PCR was used to examine keratinocyte marker genes in keratin 10, keratin 14, and Involucrin. The MTT assay results showed higher cell viability and the proliferation of neo-keratinocytes on PCL–PG fibrillar scaffolds than the PCL scaffold. On the PCL–PG scaffolds in the presence of hAMSCs as a feeder layer, the PCR and ICC analysis had a higher cell differentiation compared to neat PCL scaffolds. Moreover, SEM images showed that the keratinocytes cocultured with hAMSCs demonstrated a better proliferation and adhesion on PCL–PG nanofiber scaffolds. Based on results, PG increased the nanofibrous PCL scaffold's biological properties, including hydrophilicity, cell attachment, cell viability, and expression of keratinocyte markers in the neat keratinocytes and hAMSCs coculture system. The findings support the potential of this engineered construct for engineering skin tissue and wound dressing.
Graphic abstract






Similar content being viewed by others
Availability of data and materials
The data sets supporting the results of this article are included in the article.
Abbreviations
- hAMSCs:
-
Human adipose-derived mesenchymal stem cells
- neo-K:
-
Neonate Keratinocytes
- PCL:
-
Polycaprolactone
- PG:
-
Platelet gel
- SEM:
-
Scanning electron microscope
- FTIR-ATR:
-
Fourier transform infrared Spectroscopy-Attenuated total reflection
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- ICC:
-
Immunocytochemistry
- PCR:
-
Polymerase chain reaction
- 3D:
-
Three dimensional
References
Golchin A, Hosseinzadeh S, Jouybar A et al (2020) Wound healing improvement by curcumin-loaded electrospun nanofibers and BFP-MSCs as a bioactive dressing. Polym Adv Technol. https://doi.org/10.1002/pat.4881
Papini R (2004) Management of burn injuries of various depths. BMJ 329:158–160. https://doi.org/10.1136/bmj.329.7458.158
Jayarama Reddy V, Radhakrishnan S, Ravichandran R et al (2013) Nanofibrous structured biomimetic strategies for skin tissue regeneration. Wound Repair Regen 21:1–16
Golchin A, Farahany TZ (2019) Biological products: cellular therapy and FDA approved products. Stem Cell Rev Rep 15:1–10. https://doi.org/10.1007/s12015-018-9866-1
Golchin A, Hosseinzadeh S, Staji M et al (2019) Biological behavior of the curcumin incorporated chitosan/poly(vinyl alcohol) nanofibers for biomedical applications. J Cell Biochem. https://doi.org/10.1002/jcb.28808
Mavis B, Demirtaş TT, Gümüşderelioǧlu M et al (2009) Synthesis, characterization and osteoblastic activity of polycaprolactone nanofibers coated with biomimetic calcium phosphate. Acta Biomater 5:3098–3111. https://doi.org/10.1016/j.actbio.2009.04.037
Chen VJ, Ma PX (2004) Nano-fibrous poly(L-lactic acid) scaffolds with interconnected spherical macropores. Biomaterials 25:2065–2073. https://doi.org/10.1016/j.biomaterials.2003.08.058
Hartgerink JD, Beniash E, Stupp SI (2002) Peptide-amphiphile nanofibers: a versatile scaffold for the preparation of self-assembling materials. Proc Natl Acad Sci U S A 99:5133–5138. https://doi.org/10.1073/pnas.072699999
Zhu Y, Leong MF, Ong WF et al (2007) Esophageal epithelium regeneration on fibronectin grafted poly(l-lactide-co-caprolactone) (PLLC) nanofiber scaffold. Biomaterials 28:861–868. https://doi.org/10.1016/j.biomaterials.2006.09.051
Nemati S, Jeong KS, Shin YM, Shin H (2019) Current progress in application of polymeric nanofibers to tissue engineering. Nano Converg 6:1–16
Gizaw M, Faglie A, Pieper M et al (2019) The role of electrospun fiber scaffolds in stem cell therapy for skin tissue regeneration. Med One. https://doi.org/10.20900/mo.20190002
Kim HS, Sun X, Lee JH et al (2019) Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv Drug Deliv Rev 146:209–239
Golchin A, Nourani MR (2020) Effects of bilayer nanofibrillar scaffolds containing epidermal growth factor on full-thickness wound healing. Polym Adv Technol 31:2443–2452. https://doi.org/10.1002/pat.4960
Yildirimer L, Thanh NTK, Seifalian AM (2012) Skin regeneration scaffolds: a multimodal bottom-up approach. Trends Biotechnol 30:638–648. https://doi.org/10.1016/j.tibtech.2012.08.004
Golchin A, Hosseinzadeh S, Jouybar A et al (2020) Wound healing improvement by curcumin-loaded electrospun nanofibers and BFP-MSCs as a bioactive dressing. Polym Adv Technol. https://doi.org/10.1002/pat.4881
Gunatillake PA, Adhikari R, Gadegaard N (2003) Biodegradable synthetic polymers for tissue engineering. Eur Cells Mater 5:1–16
Woodfield TBF, Malda J, De Wijn J et al (2004) Design of porous scaffolds for cartilage tissue engineering using a three-dimensional fiber-deposition technique. Biomaterials 25:4149–4161. https://doi.org/10.1016/j.biomaterials.2003.10.056
Yol S, Tekin A, Yilmaz H et al (2008) Effects of platelet rich plasma on colonic anastomosis. J Surg Res 146:190–194
James Woodall MTMTAMH, BHB (2008) Cellular effects of Platelet Rich Plasma: Interleukin-1 release from PRP treated macrophages. Biomed Sci Instrum 44:489–494
Martinez-Zapata MJ, Martí-Carvajal AJ, Solà I et al (2016) Autologous platelet-rich plasma for treating chronic wounds. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006899.pub3
Rothe M, Falanga V (1989) Growth factors: their biology and promise in dermatologic diseases and tissue repair. Arch Dermatol 125:1390–1398. https://doi.org/10.1001/archderm.125.10.1390
Ting Yuan C-QZ 1 , M-JTS-CGB-FZ (2009) Autologous platelet-rich plasma enhances healing of chronic wounds - PubMed. Wounds 21:280–285
Declair V (1999) The importance of growth factors in wound healing - PubMed. Ostomy Wound Manag 45:64–68
Erdag G, Sheridan RL (2004) Fibroblasts improve performance of cultured composite skin substitutes on athymic mice. Burns 30:322–328. https://doi.org/10.1016/j.burns.2003.12.007
El-Ghalbzouri A, Gibbs S, Lamme E et al (2002) Effect of fibroblasts on epidermal regeneration. Br J Dermatol 147:230–243. https://doi.org/10.1046/j.1365-2133.2002.04871.x
Golchin A, Farahany TZ, Khojasteh A et al (2018) The clinical trials of mesenchymal stem cell therapy in skin diseases: an update and concise review. Curr Stem Cell Res Ther 14:22–33. https://doi.org/10.2174/1574888x13666180913123424
Aoki S, Toda S, Ando T, Sugihara H (2004) Bone marrow stromal cells, preadipocytes, and dermal fibroblasts promote epidermal regeneration in their distinctive fashions. Mol Biol Cell 15:4647–4657. https://doi.org/10.1091/mbc.E04-01-0038
Maas-Szabowski N, Szabowski A, Stark HJ et al (2001) Organotypic cocultures with genetically modified mouse fibroblasts as a tool to dissect molecular mechanisms regulating keratinocyte growth and differentiation. J Invest Dermatol 116:816–820. https://doi.org/10.1046/j.1523-1747.2001.01349.x
Jiang Y, Jahagirdar BN, Reinhardt RL et al (2002) Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 418:41–49. https://doi.org/10.1038/nature00870
Pivarcsi A, Kemény L, Dobozy A (2004) Innate immune functions of the keratinocytes: a review. Acta Microbiol Immunol Hung 51:303–310
Ardeshirylajimi A, Golchin A, Khojasteh A, Bandehpour M (2018) Increased osteogenic differentiation potential of MSCs cultured on nanofibrous structure through activation of Wnt/β-catenin signalling by inorganic polyphosphate. Artif Cells Nanomed Biotechnol 46:S943–S949. https://doi.org/10.1080/21691401.2018.1521816
Golchin A, Rekabgardan M, Taheri RA, Nourani MR (2018) Promotion of cell-based therapy: special focus on the cooperation of mesenchymal stem cell therapy and gene therapy for clinical trial studies. In: Turksen K (ed) Advances in experimental medicine and biology. Springer, New York, NY, pp 103–118
Havasi P, Nabioni M (2013) Mesenchymal stem cells as an appropriate feeder layer for prolonged in vitro culture of human induced pluripotent stem cells. Mol Biol Rep. https://doi.org/10.1007/s11033-012-2376-3
Yang HS, Shin J, Bhang SH et al (2011) Enhanced skin wound healing by a sustained release of growth factors contained in platelet-rich plasma. Exp Mol Med 43:622–629. https://doi.org/10.3858/emm.2011.43.11.070
Jeong SI, Jun ID, Choi MJ et al (2008) Development of electroactive and elastic nanofibers that contain polyaniline and poly(L-lactide-co-ε-caprolactone) for the control of cell adhesion. Macromol Biosci 8:627–637. https://doi.org/10.1002/mabi.200800005
Ardeshirylajimi A, Soleimani M, Hosseinkhani S et al (2014) A comparative study of osteogenic differentiation human induced pluripotent stem cells and adipose tissue derived mesenchymal stem cells. Cell J 16:235–244
Gümüşderelioglu M, Dalkiranoǧlu S, Aydin RST, Çakmak S (2011) A novel dermal substitute based on biofunctionalized electrospun PCL nanofibrous matrix. J Biomed Mater Res - Part A. https://doi.org/10.1002/jbm.a.33143
Chang MC, Tanaka J (2002) FT-IR study for hydroxyapatite/collagen nanocomposite cross-linked by glutaraldehyde. Biomaterials 23:4811–4818. https://doi.org/10.1016/S0142-9612(02)00232-6
Sa C, Wc C, N S, et al (2007) An electrospun triphasic nanofibrous scaffold for bone tissue engineering. Biomed Mater. https://doi.org/10.1088/1748-6041/2/2/013
Mansur HS, Oréfice RL, Mansur AAP (2004) Characterization of poly(vinyl alcohol)/poly(ethylene glycol) hydrogels and PVA-derived hybrids by small-angle X-ray scattering and FTIR spectroscopy. Polymer (Guildf) 45:7193–7202. https://doi.org/10.1016/j.polymer.2004.08.036
Ma Z, Mao Z, Gao C (2007) Surface modification and property analysis of biomedical polymers used for tissue engineering. Colloids Surf B Biointerfaces 60:137–157
Tharakan S, Pontiggia L, Biedermann T et al (2010) Transglutaminases, involucrin, and loricrin as markers of epidermal differentiation in skin substitutes derived from human sweat gland cells. Pediatr Surg Int 26:71–77. https://doi.org/10.1007/s00383-009-2517-5
Duan H, Feng B, Guo X et al (2013) Engineering of epidermis skin grafts using electrospun nanofibrous gelatin/polycaprolactone membranes. Int J Nanomed 8:2077–2084. https://doi.org/10.2147/IJN.S42384
Zhang Y, Ouyang H, Chwee TL et al (2005) Electrospinning of gelatin fibers and gelatin/PCL composite fibrous scaffolds. J Biomed Mater Res - Part B Appl Biomater 72:156–165. https://doi.org/10.1002/jbm.b.30128
Fréchette JP, Martineau I, Gagnon G (2005) Platelet-rich plasmas: Growth factor content and roles in wound healing. J Dent Res 84:434–439. https://doi.org/10.1177/154405910508400507
Carter CA, Jolly DG, Worden CE et al (2003) Platelet-rich plasma gel promotes differentiation and regeneration during equine wound healing. Exp Mol Pathol 74:244–255. https://doi.org/10.1016/S0014-4800(03)00017-0
Tayer HA, Sh A, Bateni HM, Tayer Akbar H (2012) Iran J Pediatr Hematol Oncol Vol. 2. No. 2
Kliche S, Waltenberger J (2001) VEGF receptor signaling and endothelial function. IUBMB Life 52:61–66
B C Adelmann-Grill FWZCRHTK, (1990) Chemotactic migration of normal dermal fibroblasts towards epidermal growth factor and its modulation by platelet-derived growth factor and transforming growth factor-beta - PubMed. Eur J Cell Biol 51:322–326
Andresen JL, Ehlers N (1998) Chemotaxis of human keratocytes is increased by platelet-derived growth factor-BB, epidermal growth factor, transforming growth factor-alpha, acidic fibroblast growth factor, insulin-like growth factor-I, and transforming growth factor-beta. Curr Eye Res 17:79–87. https://doi.org/10.1076/ceyr.17.1.79.5261
HOSGOOD G, (1993) Wound healing: the role of platelet-derived growth factor and transforming growth factor beta. Vet Surg 22:490–495. https://doi.org/10.1111/j.1532-950X.1993.tb00426.x
Barrientos S, Stojadinovic O, Golinko MS et al (2008) Growth factors and cytokines in wound healing. Wound Repair Regen 16:585–601
Ranjbarvan P, Soleimani M, Samadi Kuchaksaraei A et al (2017) Skin regeneration stimulation: the role of PCL-platelet gel nanofibrous scaffold. Microsc Res Tech 80:495–503. https://doi.org/10.1002/jemt.22821
Solovieva A, Miroshnichenko S, Kovalskii A et al (2017) Immobilization of platelet-rich plasma onto COOH plasma-coated PCL nanofibers Boost viability and proliferation of human mesenchymal stem cells. Polymers (Basel) 9:736. https://doi.org/10.3390/polym9120736
Chavez-Munoz C, Nguyen KT, Xu W et al (2013) Transdifferentiation of adipose-derived stem cells into keratinocyte-like cells: Engineering a stratified epidermis. PLoS One. https://doi.org/10.1371/journal.pone.0080587
Dos Odile Damour M (2014) Adipose-derived stem cells promote skin homeostasis and prevent its senescence in an in vitro skin model. J Stem Cell Res Ther. https://doi.org/10.4172/2157-7633.1000194
Sugiyama H, Maeda K, Yamato M et al (2008) Human adipose tissue-derived mesenchymal stem cells as a novel feeder layer for epithelial cells. J Tissue Eng Regen Med 2:445–449. https://doi.org/10.1002/term.111
Tosca MC, Chlapanidas T, Galuzzi M et al (2015) Human adipose-derived stromal cells as a feeder layer to improve keratinocyte expansion for clinical applications. Tissue Eng Regen Med 12:249–258. https://doi.org/10.1007/s13770-015-0007-5
Hejazian LB, Esmaeilzade B, Ghoroghi FM et al (2012) The role of biodegradable engineered nanofiber scaffolds seeded with hair follicle stem cells for tissue engineering. Iran Biomed J 16:193–201. https://doi.org/10.6091/ibj.1074.2012
Acknowledgments
The authors thank their colleagues in the Stem Cell Technology Research Center, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
PR and AG: conception, performing, collecting data, data analyzing, and interpreting. All authors cooperated in manuscript writing and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethics approval and consent to participate
The study protocol was approved by the Tehran University of Medical Sciences of Iran, and all procedures were performed following the guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ranjbarvan, P., Golchin, A., Azari, A. et al. The bilayer skin substitute based on human adipose-derived mesenchymal stem cells and neonate keratinocytes on the 3D nanofibrous PCL-platelet gel scaffold. Polym. Bull. 79, 4013–4030 (2022). https://doi.org/10.1007/s00289-021-03702-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-021-03702-0