Abstract
Biofilms reduce the bacterial growth rate, inhibit antibiotic penetration, lead to the development of persister cells and facilitate genetic exchange. The biofilm-associated Klebsiella pneumoniae infections have not been well studied, and their implications in overcoming the effects of antimicrobial therapy are yet to be fully understood. Hence this study evaluated the antibiotic resistance pattern, antibiotic resistance determinants of extended-spectrum beta-lactamase (ESBL) family. Biofilm-forming ability of seventy multidrug-resistant clinical isolates of K. pneumoniae and the biofilm-associated genes of representative biofilm formers from a tertiary care hospital were also assessed. The K. pneumoniae isolated from urine exhibited resistance towards ceftazidime, nalidixic acid and meropenem. Isolates from blood were resistant to cefuroxime. Higher rates of resistance were observed towards cefuroxime, nalidixic acid, and meropenem for the isolates from the endotracheal aspirate. Extended spectrum beta-lactamase production by CLSI’s disc diffusion-based confirmation test revealed all the K. pneumoniae to be as ESBL producers. Most of the isolates harboured the bla gene variants, blaSHV and blaTEM. Majority of the isolates were colistin sensitive. 97.1% of the K. pneumoniae produced biofilm. K. pneumoniae isolated from pus and blood produced fully established biofilms. Strong biofilm formers were sensitive to co-trimoxazole and ciprofloxacin. Moderate biofilm formers exhibited sensitivity towards meropenem and imipenem. Expression of the fimH gene was increased, while mrkD showed reduced expression among the strong biofilm formers. Moderate biofilm formers showed variable expression of the genes associated with the biofilm formation. The weak and non-biofilm formers showed reduced expression of both the fimbrial genes. Multidrug-resistant isolates produced ESBLs and formed well-established biofilms.

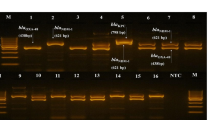
Source-wise representation of antibiotic resistance pattern of all the clinical isolates of K. pneumoniae against nine antibiotics. CIP ciprofloxacin, CAZ ceftazidime, CXM cefuroxime, C chloramphenicol, COT co-trimoxazole, CTX cefotaxime, IPM imipenem, MRP meropenem, NA nalidixic acid


source and the biofilm-forming ability of the clinical isolates of K. pneumoniae


Similar content being viewed by others
Data Availability (Data Transparency)
Not applicable.
Code Availability (Software Application or Custom Code)
Not applicable.
References
Rahamathulla MP, Harish BN, Mataseje L, Mulvey MR (2016) Carbapenem resistance mechanisms among blood isolates of Klebsiella pneumoniae and Escherichia coli. Afr J Microbiol Res 2:45–53. https://doi.org/10.5897/AJMR2015.7802
Wyres KL, Holt KE (2018) Klebsiella pneumoniae as a key trafficker of drug resistance genes from environmental to clinically important bacteria. Curr Opin Microbiol 45:131–139. https://doi.org/10.1016/j.mib.2018.04.004
Jadhav S, Misra R, Gandham N, Ujagare M, Ghosh P, Angadi K, Vyawahare C (2012) Increasing incidence of multidrug resistance Klebsiella pneumoniae infections in hospital and community settings. Int J Microbiol Res 4:253–257
Vuotto C, Longo F, Balice MP, Donelli G, Varaldo PE (2014) Antibiotic resistance related to biofilm formation in Klebsiella pneumoniae. Pathogens 3:743–758. https://doi.org/10.3390/pathogens3030743
Aher T, Roy A, Kumar P (2012) Molecular detection of virulence genes associated with pathogenicity of Klebsiella spp. isolated from the respiratory tract of apparently healthy as well as sick goats. Isr J Vet Med 67:249–252
Bandeira M, Carvalho PA, Duarte A, Jordao L (2014) Exploring dangerous connections between Klebsiella pneumoniae biofilms and healthcare-associated infections. Pathogens 3:720–731. https://doi.org/10.3390/pathogens3030720
Desai S, Sanghrajka K, Gajjar D (2019) High adhesion and increased cell death contribute to strong biofilm formation in Klebsiella pneumoniae. Pathogens 4:277
Bengoechea JA, Sa Pessoa J (2019) Klebsiella pneumoniae infection biology: living to counteract host defences. FEMS Microbiol Rev 2:123–144. https://doi.org/10.3390/pathogens8040277
Chen L, Wilksch JJ, Liu H, Zhang X, Torres VV, Bi W, Mandela E, Cao J, Li J, Lithgow T, Zhou T (2020) Investigation of LuxS-mediated quorum sensing in Klebsiella pneumoniae. J Med Microbiol 3:402
Pal S, Verma J, Mallick S, Rastogi SK, Kumar A, Ghosh AS (2019) Absence of the glycosyltransferase WcaJ in Klebsiella pneumoniae ATCC13883 affects biofilm formation, increases polymyxin resistance and reduces murine macrophage activation. Microbiology 8:891–904. https://doi.org/10.1099/mic.0.000827
Zheng JX, Lin ZW, Chen C, Chen Z, Lin FJ, Wu Y, Yang SY, Sun X, Yao WM, Li DY, Yu ZJ (2018) Biofilm formation in Klebsiella pneumoniae bacteremia strains was found to be associated with CC23 and the presence of wcaG. Front Cell Infect Microbiol 8:21. https://doi.org/10.3389/fcimb.2018.00021
El Fertas-Aissani R, Messai Y, Alouache S, Bakour R (2013) Virulence profiles and antibiotic susceptibility patterns of Klebsiella pneumoniae strains isolated from different clinical specimens. Pathol Biol 5:209–216. https://doi.org/10.1016/j.patbio.2012.10.004
Stahlhut SG, Struve C, Krogfelt KA, Reisner A (2012) Biofilm formation of Klebsiella pneumoniae on urethral catheters requires either type 1 or type 3 fimbriae. FEMS Immunol Med Microbiol 2:350–359. https://doi.org/10.1111/j.1574-695X.2012.00965.x
Devanga Ragupathi NK, Muthuirulandi Sethuvel DP, Triplicane Dwarakanathan H, Murugan D, Umashankar Y, Monk PN, Karunakaran E, Veeraraghavan B (2020) The influence of biofilms on carbapenem susceptibility and patient outcome in device associated K pneumoniae infections: insights into phenotype vs genome-wide analysis and correlation. Front Microbiol 11:3220. https://doi.org/10.3389/fmicb.2020.591679
Capita R, Alonso-Calleja C (2013) Antibiotic-resistant bacteria: a challenge for the food industry. Crit Rev Food Sci Nutr 1:11–48. https://doi.org/10.1080/10408398.2010.519837
Yasmin T (2012) Prevalence of ESBL among Esch. coli and Klebsiella spp. in a tertiary care hospital and molecular detection of important ESBL producing genes by multiplex PCR. Mymensingh Med J
Choudhury R, Panda S, Singh DV (2012) Emergence and dissemination of antibiotic resistance: a global problem. Indian J Med Microbiol 4:384. https://doi.org/10.4103/0255-0857.103756
Alcántar-Curiel MD, Ledezma-Escalante CA, Jarillo-Quijada MD, Gayosso-Vázquez C, Morfín-Otero R, Rodríguez-Noriega E, Cedillo-Ramírez ML, Santos-Preciado JI, Girón JA (2018) Association of antibiotic resistance, cell adherence, and biofilm production with the endemicity of nosocomial Klebsiella pneumoniae. Biomed Res Int. https://doi.org/10.1155/2018/7012958
Vasoo S, Barreto JN, Tosh PK (2015) Emerging issues in Gram-negative bacterial resistance: an update for the practicing clinician. Mayo Clin Proc 3:395–403. https://doi.org/10.1016/j.mayocp.2014.12.002
Ausubel FM, Brent R, Kingston RE, Moore DD, Seidman JG, Smith JA, Struhl K (1987) Current protocols in molecular biology. Greene & Wiley, New York
Stepanovic S, Cirkovic I, Ranin L, Svabic-Vlahovic M (2004) Biofilm formation by Salmonella spp. and Listeria monocytogenes on plastic surface. Lett Appl Microbiol 5:428–432. https://doi.org/10.1111/j.1472-765X.2004.01513.x
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2 (-Delta Delta C (T)) method. Methods 4:402–408. https://doi.org/10.1006/meth.2001.1262
Biradar S, Roopa C (2015) Isolation and antibiogram of Klebsiella species from various clinical specimens. IJCMAS 9:991–995
Sathyavathy K, Madhusudhan BK (2015) Isolation and identification of Klebsiella species from various clinical samples at a tertiary care hospital, South India. Indian J Public Health Res Dev 10:4033–4036
Gupta S, Maheshwari V, Shah R (2017) Prevalence of ESBL producing Escherichia coli and Klebsiella species among clinical isolates and their in vitro antimicrobial susceptibility pattern in a tertiary care hospital. Int J Curr Microbiol Appl Sci 6:2295–2303
Papadimitriou-Olivgeris M, Fligou F, Bartzavali C, Zotou A, Spyropoulou A, Koutsileou K, Vamvakopoulou S, Sioulas N, Karamouzos V, Anastassiou ED, Spiliopoulou I (2017) Carbapenemase-producing Klebsiella pneumoniae bloodstream infection in critically ill patients: risk factors and predictors of mortality. Eur J Clin Microbiol Infect Dis 7:1125–1131. https://doi.org/10.1007/s10096-017-2899-6
Varghese A, George S, Gopalakrishnan R, Mathew A (2016) Antibiotic susceptibility pattern of Klebsiella pneumoniae isolated from cases of urinary tract infection in a tertiary care setup. Evol Med Dent Sci 5:1470–1474
Sharma N, Gupta AK, Walia G, Bakhshi R (2016) A retrospective study of the changing trends of antimicrobial resistance of Klebsiella pneumoniae isolated from urine samples over last 3 years (2012–2014). J Nat Sci Biol Med 7:39–42. https://doi.org/10.4103/2F0976-9668.175060
Alcántar-Curiel MD, Rosales-Reyes R, Jarillo-Quijada MD, Gayosso-Vázquez C, Fernández-Vázquez JL, Toledano-Tableros JE, Giono-Cerezo S, Garza-Villafuerte P, López-Huerta A, Vences-Vences D, Morfín-Otero R (2019) Carbapenem-resistant Acinetobacter baumannii in three tertiary care hospitals in Mexico: virulence profiles, innate immune response and clonal dissemination. Front Microbiol 10:2116. https://doi.org/10.3389/fmicb.2019.02116
Mittal S, Mamoria VP, Singla A, Bacchani D, Chaudhary P (2020) Phenotypic Detection of Metallo-β-lactamase in Carbapenem Resistant Clinical Isolates of Klebsiella pneumoniae ssp. pneumoniae at a Tertiary Care Hospital in Jaipur. JMSCR 8:2455. https://doi.org/10.18535/jmscr/v8i3.120
Kar B, Sharma M, Peter A, Chetia P, Neog B, Borah A, Pati S, Bhattacharya D (2021) Prevalence and molecular characterization of β-lactamase producers and fluoroquinolone resistant clinical isolates from North East India. J Infect Public Health 14:628–637. https://doi.org/10.1016/j.jiph.2021.02.007
Geetha PV, Aishwarya KV, Mariappan S, Sekar U (2020) Fluoroquinolone resistance in clinical isolates of Klebsiella Pneumoniae. J Lab Phys 12:121–125. https://doi.org/10.1055/s-0040-1716478
Sonia SJ, Afroz S, Rasheduzzaman M, Uddin KH, Shamsuzzaman SM (2020) Prevalence and antimicrobial susceptibility pattern of Klebsiella Pneumoniae isolated from various clinical specimens in a tertiary care hospital in Bangladesh. Med Today 32:95–99. https://doi.org/10.3329/medtoday.v32i2.48821
Feizabadi MM, Mahamadi-Yeganeh S, Mirsalehian A, Mirafshar SM, Mahboobi M, Nili F, Yadegarinia D (2010) Genetic characterization of ESBL producing strains of Klebsiella pneumoniae from Tehran hospitals. JIDC 10:609–615. https://doi.org/10.3855/jidc.1059
Sahoo RK, Das A, Gaur M, Pattanayak A, Sahoo S, Debata NK, Rahman PK, Subudhi E (2019) Genotypic validation of extended-spectrum β-lactamase and virulence factors in multidrug resistance Klebsiella pneumoniae in an Indian hospital. Pathog Glob Health 7:315–321. https://doi.org/10.1080/20477724.2019.1705020
El-Badawy MF, Tawakol WM, El-Far SW, Maghrabi IA, Al-Ghamdi SA, Mansy MS, Ashour MS, Shohayeb MM (2017) Molecular identification of aminoglycoside-modifying enzymes and plasmid-mediated quinolone resistance genes among Klebsiella pneumoniae clinical isolates recovered from Egyptian patients. Int J Microbiol. https://doi.org/10.1155/2017/8050432
Shams E, Firoozeh F, Moniri R, Zibaei M (2015) Prevalence of plasmid-mediated quinolone resistance genes among extended-spectrum β-Lactamase-producing Klebsiella pneumoniae human isolates in Iran. J Pathog. https://doi.org/10.1155/2015/434391
Wang A, Yang Y, Lu Q, Wang Y, Chen Y, Deng L, Ding H, Deng Q, Wang L, Shen X (2008) Occurrence of qnr-positive clinical isolates in Klebsiella pneumoniae producing ESBL or AmpC-type β-lactamase from five pediatric hospitals in China. FEMS Microbiol Lett 1:112–116. https://doi.org/10.1111/j.1574-6968.2008.01163.x
Cepas V, López Y, Muñoz E, Rolo D, Ardanuy C, Martí S, Xercavins M, Horcajada JP, Bosch J, Soto SM (2019) Relationship between biofilm formation and antimicrobial resistance in Gram-negative bacteria. Microb Drug Resist 1:72–79. https://doi.org/10.1089/mdr.2018.0027
Nirwati H, Sinanjung K, Fahrunissa F, Wijaya F, Napitupulu S, Hati VP, Hakim MS, Meliala A, Aman AT, Nuryastuti T (2019) Biofilm formation and antibiotic resistance of Klebsiella pneumoniae isolated from clinical samples in a tertiary care hospital, Klaten, Indonesia. BMC 13:1–8. https://doi.org/10.1111/jam.13533
Hassan A, Usman J, Kaleem F, Omair M, Khalid A, Iqbal M (2011) Evaluation of different detection methods of biofilm formation in the clinical isolates. Braz J Infect Dis 4:305–311. https://doi.org/10.1590/S1413-86702011000400002
Seifi K, Kazemian H, Heidari H, Rezagholizadeh F, Saee Y, Shirvani F, Houri H (2016) Evaluation of biofilm formation among Klebsiella pneumoniae isolates and molecular characterization by ERIC-PCR. Jundishapur J Microbiol 1:e30682. https://doi.org/10.5812/2Fjjm.30682
Yang D, Zhang Z (2008) Biofilm-forming Klebsiella pneumoniae strains have greater likelihood of producing extended-spectrum β-lactamases. J Hosp Infect 4:369–371. https://doi.org/10.1016/j.jhin.2008.02.001
Mishra SK, Basukala P, Basukala O, Parajuli K, Pokhrel BM, Rijal BP (2015) Detection of biofilm production and antibiotic resistance pattern in clinical isolates from indwelling medical devices. Curr Microbiol 1:128–134. https://doi.org/10.1007/s00284-014-0694-5
Türkel I, Yıldırım T, Yazgan B, Bilgin M, Başbulut E (2018) Relationship between antibiotic resistance, efflux pumps, and biofilm formation in extended-spectrum β-lactamase producing Klebsiella pneumoniae. J Chemother 6–8:354–363. https://doi.org/10.1080/1120009X.2018.1521773
Subramanian P, Shanmugam N, Sivaraman U, Kumar S, Selvaraj S (2012) Antiobiotic resistance pattern of biofilm-forming uropathogens isolated from catheterised patients in Pondicherry. India Med J Aust 7:344. https://doi.org/10.4066/2FAMJ.2012.1193
Mah TF, Pitts B, Pellock B, Walker GC, Stewart PS, O’Toole GA (2003) A genetic basis for Pseudomonas aeruginosa biofilm antibiotic resistance. Nature 426(6964):306–310
Zhang L, Fritsch M, Hammond L, Landreville R, Slatculescu C, Colavita A, Mah TF (2013) Identification of genes involved in Pseudomonas aeruginosa biofilm-specific resistance to antibiotics. PLoS ONE 8(4):e61625
Saha A, Devi KM, Damrolien S, Krossnunpuii DKS, Sharma KT (2018) Biofilm production and its correlation with antibiotic resistance pattern among clinical isolates of Pseudomonas aeruginosa in a tertiary care hospital in north-East India. Int J Adv Med 4:964–968
Vuotto C, Longo F, Pascolini C, Donelli G, Balice MP, Libori MF, Tiracchia V, Salvia A, Varaldo PE (2017) Biofilm formation and antibiotic resistance in Klebsiella pneumoniae urinary strains. J Appl Microbiol 4:1003–1018. https://doi.org/10.1111/jam.13533
Clegg S, Murphy CN (2016) Epidemiology and virulence of Klebsiella pneumoniae. Mol Pathog Clin Manag 15:435–445. https://doi.org/10.1128/microbiolspec.UTI-0005-2012
Murphy CN, Mortensen MS, Krogfelt KA, Clegg S (2013) Role of Klebsiella pneumoniae type 1 and type 3 fimbriae in colonizing silicone tubes implanted into the bladders of mice as a model of catheter-associated urinary tract infections. Infect Immun 8:3009–3017. https://doi.org/10.1128/IAI.00348-13
Schroll C, Barken KB, Krogfelt KA, Struve C (2010) Role of type 1 and type 3 fimbriae in Klebsiella pneumoniae biofilm formation. BMC Microbiol 1:1
Tajbakhsh E, Ahmadi P, Abedpour-Dehkordi E, Arbab-Soleimani N, Khamesipour F (2016) Biofilm formation, antimicrobial susceptibility, serogroups and virulence genes of uropathogenic E. coli isolated from clinical samples in Iran. Antimicrob Resist Infect Control 1:1–8. https://doi.org/10.1186/s13756-016-0109-4
Mohamed SH, Khalil MS, Mohamed MS, Mabrouk MI (2020) Prevalence of antibiotic resistance and biofilm formation in Klebsiella pneumoniae carrying fimbrial genes in Egypt. Res J Pharm Technol 7:3051–3058. https://doi.org/10.5958/0974-360X.2020.00542.9
Liu Y, Liu C, Zheng W, Zhang X, Yu J, Gao Q, Hou Y, Huang X (2008) PCR detection of Klebsiella pneumoniae in infant formula based on 16S–23S internal transcribed spacer. Int J Food Microbiol 3:230–235. https://doi.org/10.1016/j.ijfoodmicro.2008.03.005
BrisseS VJ (2001) Phylogenetic diversity of Klebsiella pneumoniae and Klebsiella oxytoca clinical isolates revealed by randomly amplified polymorphic DNA gyrA and parC genes sequencing and automated ribotyping. Int J Syst Evol Microbiol 51:915–924. https://doi.org/10.1099/00207713-51-3-915
Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, Alberti S, Bush K, Tenover FC (2008) Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother 45:1151–1161. https://doi.org/10.1128/AAC.45.4.1151-1161.2001
Mahrouki S, Belhadj O, Chihi H, Mohamed BM, Celenza G, Amicosante G, Perilli M (2012) Chromosomal blaCTX-M-15 associated with ISEcp1 in Proteus mirabilis and Morganella morganii isolated at the Military Hospital of Tunis, Tunisia. J Med Microbiol 61:1286–1289. https://doi.org/10.1099/jmm.0.039487-0
Batchelor M, Hopkins K, Threlfall EJ, Clifton-Hadley FA, Stallwood AD, Davies RH (2005) blaCTX-M genes in clinical Salmonella isolates recovered from humans in England and Wales from 1992 to 2003. Antimicrob Agents Chemother 49:1319–1322. https://doi.org/10.1128/AAC.49.4.1319-1322.2005
Zhao S, White DG, Ge B, Ayers S, Friedman S, English L, Wagner D, Gaines S, Meng J (2001) Identification and characterization of integron-mediated antibiotic resistance among Shiga toxin-producing Escherichia coli isolates. Appl Environ Microbiol 67:1558–1564. https://doi.org/10.1128/AEM.67.4.1558-1564.2001
Robicsek A, Jacoby GA, Hooper DC (2006) The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis 6:629–640. https://doi.org/10.1016/S1473-3099(06)70599-0
Cattoir V, Poirel L, Nordmann P (2008) Plasmid-mediated quinolone resistance pump QepA2 in an Escherichia coli isolate from France. Antimicrob Agents Chemother 52:3801–3804. https://doi.org/10.1128/AAC.00638-08
Ritz M, Garenaux A, Berge M, Federighi M (2009) Determination of rpoA as the most suitable internal control to study stress response in C. jejuni by RT-qPCR and application to oxidative stress. J Microbiol Methods 76:196–200. https://doi.org/10.1016/j.mimet.2008.10.014
Funding
We would like to acknowledge the Nitte (Deemed to be University) for the Financial support received from (Grant no. NUFR1/2018/10/17), Mangalore, towards this study.
Author information
Authors and Affiliations
Contributions
PA—AM and BB. DVK—AM and GR. AR—AM and GR. ID – AM. IK – BB. IK – BB. ADS—AM and DB.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Institutional Ethics Committee of the Madras Medical Mission, Chennai (Reg. No: ECR/140/Inst/TN/2013/RR-20).
Informed Consent
The informed consent for each patient included in the study was obtained.
Consent for Participation
The informed consent for each patient included in the study was obtained.
Consent for Publication
All the authors are aware and have no conflicts for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ashwath, P., Deekshit, V.K., Rohit, A. et al. Biofilm Formation and Associated Gene Expression in Multidrug-Resistant Klebsiella pneumoniae Isolated from Clinical Specimens. Curr Microbiol 79, 73 (2022). https://doi.org/10.1007/s00284-022-02766-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-022-02766-z