Abstract
Purpose
Sorafenib is an effective therapy for advanced hepatocellular carcinoma (HCC). Hand–foot syndrome (HFS) is a serious adverse effect associated with sorafenib therapy. This study aimed to develop an updated clinical prediction tool that allows personalized prediction of HFS following sorafenib initiation.
Methods
Individual participant data from Phase III clinical trial NCT00699374 were used in Cox proportional hazard analysis of the association between pre-treatment clinicopathological data and grade ≥ 3 HFS occurring within the first 365 days of sorafenib treatment for advanced HCC. Multivariable prediction models were developed using stepwise forward inclusion and backward deletion and internally validated using a random forest machine learning approach.
Results
Of 542 patients, 116 (21%) experienced grades ≥ 3 HFS. The prediction tool was optimally defined by sex (male vs female), haemoglobin (< 130 vs ≥ 130 g/L) and bilirubin (< 10 vs 10–20 vs ≥ 20 µmol/L). The prediction tool was able to discriminate subgroups with significantly different risks of grade ≥ 3 HFS (P ≤ 0.001). The high (score = 3 +)-, intermediate (score = 2)- and low (score = 0–1)-risk subgroups had 40%, 27% and 14% probability of developing grade ≥ 3 HFS within the first 365 days of sorafenib treatment, respectively.
Conclusion
A clinical prediction tool defined by female sex, high haemoglobin and low bilirubin had high discrimination for predicting HFS risk. The tool may enable improved evaluation of personalized risks of HFS for patients with advanced HCC initiating sorafenib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) accounts for approximately 80–85% of primary liver cancers [1]. Due to the lack of symptoms in early stages, HCC is often left undetected until it progresses to advanced stages, resulting in poor prognosis [2, 3]. Sorafenib is a multi-kinase inhibitor approved for treatment of HCC; however, it is associated with multiple dose-limiting toxicities.
Dermatologic side effects are amongst the most common side effects of sorafenib [4, 5]. For example, hand–foot syndrome (HFS) of any grade is experienced by approximately 61% of patients [5]. HFS typically develops 2–4 weeks after sorafenib initiation [6] and is characterized by painful erythema, scaling, and ulceration affecting the hand and feet, which can lead to reduced patient quality of life [7, 8]. Further, the development of HFS of grade ≥ 3 is considered a serious adverse effect that may lead to dosage regimen adjustment and/or premature treatment termination [9].
Risk prediction models are used by clinicians to inform the management of patients using anti-cancer medicines [10, 11]. A clinical prediction tool for sorafenib-induced grade ≥ 2 HFS in advanced renal cell carcinoma has been previously developed [9]; however, it is unclear if this tool is generable to patients with advanced HCC where sorafenib is mostly used. Further, there is limited specificity to the prediction of sorafenib-induced grade ≥ 3 HFS, which are the events more likely to result in dose adjustments/treatment termination. This study aimed to calibrate a clinical prediction tool that allows personalized risk predictions of grade ≥ 3 HFS following sorafenib initiation for advanced HCC treatment.
Materials and methods
Patient population
Individual participant data (IPD) from the sorafenib arm of phase III trial NCT00699374 were used for this secondary analysis. Sorafenib was initiated at 400 mg twice daily, in 4-week cycles, to eligible participants with locally advanced or metastatic HCC [5]. Dose reduction was permitted to manage dose-limiting toxicities.
Data were made available through Project Data Sphere (www.projectdatasphere.org). Project Data Sphere is an independent non-profit, open-access cancer research platform hosting de-identified patient-level data from completed cancer clinical trials that can be shared with independent researchers to improve cancer care. Secondary analysis of anonymized IPD was exempted from review by the Southern Adelaide Local Health Network, Office for Research and Ethics as it was classified as minimal risk research.
Predictors and outcomes
The primary assessed outcome was grade ≥ 3 HFS occurring within the first 365 days of sorafenib. Adverse effects were defined by grade according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 3.0 [12].
Assessed pre-treatment clinicopathological variables were selected upon availability, prior evidence, and biological plausibility and included age (years), sex (male vs female), race (Asian vs Non-Asian), body mass index, ECOG performance status (ECOG PS), presence of liver/lung metastases, tumour count, leukocyte count, albumin, serum alanine aminotransferase, bilirubin, haemoglobin, estimated glomerular filtration rate, urea, and concomitant use of corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs). The rationale for selecting each of the aforementioned variables is provided in supplementary Table 1.
Statistical analysis
A univariable Cox proportional hazard analysis was conducted to assess the association between potential predictors and grade ≥ 3 HFS. Associations were reported as hazard ratios (HR) with 95% confidence intervals (CI). Statistical significance was set at P < 0.05, determined via the likelihood ratio test. Continuous variables were categorised based on model fit, observed non-linearity, prior evidence, and clinically interpretable cut-points. Prediction performances were assessed via the concordance statistic (c statistic) estimated using the Harrell method [13].
A multivariable risk prediction model was developed using stepwise forward inclusion of variables with a P < 0.05 and the greatest improvement in the c statistic at each forward step; followed by backward deletion of variables with P > 0.05 and did not increase the c statistic by 0.02. The backward deletion process was conducted to find the minimal number of predictors with maintained prediction performance.
The final multivariable model was then internally validated using random forest analysis [14], a machine learning approach. Specifically, random forest analysis enabled an independent evaluation of variables of importance as compared to variables selected as important in the stepwise model. The relative importance of variables in the random forest model was determined using permutation variable importance measure as described previously [15]. The relative importance of each variable was scaled to 100, with a higher value indicating a stronger influence on predicting the outcome of interest.
The random forest was also used to assess for any signs of model overfitting. Model overfitting was assessed by training the model using the k-fold cross-validation approach (fivefold cross-valuation repeated 10 times). Using this approach, the data are split randomly into fivefold of training and test sets. The training set is used to build the model, the model is used to predict the test data, and the prediction performance of the model is recorded. This process was repeated 10 times (i.e. total number of trained models = 50) and the average (95% CI) of the prediction performance (c statistics) was reported. The values for the random forest hyperparameters were set to default and the model was trained using 1000 fitted trees.
To facilitate clinical utility, a risk prediction tool was developed from the validated final multivariable model. Whereby the estimates of the regression coefficients in the final multivariable model were scaled to the nearest integer value to allow the calculation of a linear predictor score (i.e. an interpretable risk score). The integer values allocated to each significant predictor within the final prediction model are described in the results section. The performance of the developed tool was further compared to the prediction model of grade ≥ 2 HFS proposed by Dranitsaris et al. in patients with advanced cell carcinoma receiving sorafenib [9]. Risk probabilities were assessed using the Kaplan–Meier method. Statistical analysis was performed using R version 4.1.0.
Results
Patient population
Data were available from 542 patients with advanced HCC who received sorafenib therapy. All patients received a starting sorafenib dose of 400 mg twice daily until disease progression or occurrence of unexpected toxicity. Median follow-up was 22 [95% CI 21–24] months in the cohort. A summary of pre-treatment patient characteristics is presented in Table 1. Of the 542 patients, 116 (21%) experienced grade ≥ 3 HFS during follow-up, with 78% of these events occurring within the first 30 days.
Prediction of grade ≥ 3 hand–foot syndrome
Univariable analysis identified bilirubin, albumin, haemoglobin, sex, race as significantly associated with the development of grade ≥ 3 HFS following sorafenib initiation (P < 0.05, Supplementary Table 2). On forward inclusion, bilirubin, haemoglobin, sex, race, and age were identified as the statistically significant predictors. The backwards elimination process resulted in a final multivariable model optimally defined by bilirubin (< 10 vs ≥ 10 and < 20 vs ≥ 20 µmol/L), haemoglobin (≥ 130 vs < 130 g/L), and sex (female vs male) (Table 2, c statistics = 0.64).
Machine learning model validation
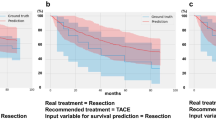
The random forest machine learning model identified sex, bilirubin and haemoglobin as the most important variables in predicting grade ≥ 3 HFS confirming the validity of the variables selected in the final multivariable model. The top 10 most influential predictors of HFS from the random forest are presented in Fig. 1. The discrimination performance from the repeated cross-validated random forest model (mean, 95% CI) was 0.61 (0.59–0.63), suggesting no overfitting of the training data.
Development of clinical prediction tool of grade ≥ 3 hand–foot syndrome
A risk scoring tool based on the final multivariable model was then developed. Prediction risk scores were derived from the final multivariable model where female sex equated to 1 point, haemoglobin ≥ 130 g/L equated to 1 point, bilirubin ≥ 10 and < 20 µmol/L equated to 1 point and bilirubin < 10 µmol/L equated to 2 points. Patients were then categorized into three categories (0–1, 2 and 3+) where a higher score indicates an increased risk of grade ≥ 3 HFS (Fig. 2).
The discrimination performance (mean c, 95%CI) of the developed risk prediction tool (Supplementary Table 3) was superior to Dranitsaris et al. risk tool for predicting grade ≥ 3 HFS (developed risk tool c = 0.63 [0.58–0.67], Dranitsaris et al. risk tool c = 0.50 [0.45–0.56], P < 0.001). The latter suggests that Dranitsaris et al. risk tool, which was initially developed to predict grade ≥ 2 HFS in patients with renal cell carcinoma, is not generalizable to predicting grade ≥ 3 HFS in patients with hepatocellular carcinoma.
The estimated probability (median, 95% CI) of developing grade ≥ 3 HFS within the first 365 days of sorafenib therapy in the high (score = 3+)-, intermediate (score = 2)- and low (score = 0–1)-risk subgroups were 40% [28–50%], 27% [19%-33%] and 14% [9–18%], respectively (Fig. 2). Figure 3 presents the Kaplan–Meier plots for grade ≥ 3 HFS according to risk score subgroups.
Discussion
This study developed a clinical prediction tool for sorafenib-induced grade ≥ 3 HFS in advanced HCC. The model was internally validated using a random forest machine learning approach. The predicted risk of grade ≥ 3 HFS within the first 365 days of initiating sorafenib therapy ranged from 14 to 40% and was optimally defined by sex (male vs female), haemoglobin (< 130 vs ≥ 130 g/L) and bilirubin (< 10 vs ≥ 10 and < 20 vs ≥ 20 µmol/L) levels.
The female sex association with HFS following sorafenib treatment in advanced HCC is consistent with existing literature where the reported relative risk for developing HFS upon sorafenib treatment in renal cell carcinoma cohort is increased by 68% in females [9]. In addition, high baseline bilirubin was independently associated with decreased risk of HFS. Prior research assessing the association of bilirubin levels and HFS is lacking. In a small study of 83 patients, Boudou-Rouquette et al. reported an increased incidence of HFS in patients with high bilirubin levels; however, the association was confounded, and their finding was not significant upon multivariable analysis [16]. Further investigation is needed on the complex relationship between bilirubin and sorafenib-induced HFS. Further, this analysis identified high haemoglobin levels to be associated with increased risk for grade ≥ 3 HFS. A previous preliminary study identified haemoglobin as an important factor in the development of HFS [17]. While the exact mechanism is not fully elucidated, previous studies reported that sorafenib was observed to cause haemolysis of red blood cells leading to an increase in extracellular haeme [18, 19]. Extracellular haeme can cause oxidative damage and vascular injury and high-grade skin inflammation [20,21,22,23] and, therefore, can potentially contribute to the development of HFS.
The analysis presented herein demonstrates that the existing prediction model developed for predicting sorafenib-induced grade ≥ 2 HFS in advanced renal cell carcinoma population is not generalizable to patients with advanced HCC. Unlike the previous study [9], the presented analysis herein evaluated bilirubin amongst the potential predictors and was shown to be the most predictive variable for HFS in advanced HCC populations.
A strength of this analysis is the use of large high-quality data collected within clinical trial and the developed risk prediction tool. The tool being simple to use will greatly facilitate its implementation in the clinic for personalized risk predictions of grade ≥ 3 HFS in patients initiating sorafenib in advanced HCC. Being able to provide patient-specific risk predictions will enable patients and clinicians to better interpret the risk–benefit ratio of sorafenib therapy.
A potential study limitation is that the evaluation was restricted to patients treated with sorafenib within a clinical trial. Strict inclusion criteria of clinical trials may limit their generalizability to real-world populations. Therefore, external validation of the developed risk tool is necessary to assess the generalizability of the tool before the implementation of the tool for risk assessment in the clinic. Another potential limitation is the moderate prediction performance of the developed tool (c = 0.63) [24]. While including a broader range of predictors to build the model may improve the predictions, this analysis was limited by available sorafenib data. For example, available sorafenib data lacked information on vitamin B6/B12 and folate levels that may potentially be associated with the risk of HFS [25]. Despite these limitations, the prediction tool was able to discriminate high-, intermediate-, and low-risk patients.
In conclusion, a clinical prediction tool for sorafenib-induced grade ≥ 3 HFS was optimally developed based upon sex, haemoglobin, and bilirubin levels. The developed tool enables discrimination between risk groups and may enable improved evaluation of personalized risks of HFS for patients with advanced HCC initiating sorafenib. Future research should aim to validate this study’s findings to facilitate the transition of the development tool into clinical practice.
Availability of the data and material
Data were made available through Project Data Sphere (www.projectdatasphere.org).
References
Gelband H, Chen CJ, Chen W, Franceschi S, Hall SA, London WT, McGlynn KA, Wild CP (2015) Cancer. In: Gelband HJP, Sankaranarayanan R et al. (eds) Cancer: Disease Control Priorities, Third Edition, vol 3. 3 edn. The International Bank for Reconstruction and Development/The World Bank
Golabi P, Fazel S, Otgonsuren M, Sayiner M, Locklear CT, Younossi ZM (2017) Mortality assessment of patients with hepatocellular carcinoma according to underlying disease and treatment modalities. Medicine 96(9):e5904. https://doi.org/10.1097/MD.0000000000005904
Chen XP, Qiu FZ, Wu ZD, Zhang ZW, Huang ZY, Chen YF (2006) Long-term outcome of resection of large hepatocellular carcinoma. Br J Surg 93(5):600–606. https://doi.org/10.1002/bjs.5335
Robert C, Mateus C, Spatz A, Wechsler J, Escudier B (2009) Dermatologic symptoms associated with the multikinase inhibitor sorafenib. J Am Acad Dermatol 60(2):299–305. https://doi.org/10.1016/j.jaad.2008.06.034
Cheng AL, Kang YK, Lin DY, Park JW, Kudo M, Qin S, Chung HC, Song X, Xu J, Poggi G, Omata M, Pitman Lowenthal S, Lanzalone S, Yang L, Lechuga MJ, Raymond E (2013) Sunitinib versus sorafenib in advanced hepatocellular cancer: results of a randomized phase III trial. J Clin Oncol 31(32):4067–4075. https://doi.org/10.1200/JCO.2012.45.8372
Kamimura K, Shinagawa-Kobayashi Y, Goto R, Ogawa K, Yokoo T, Sakamaki A, Abe S, Kamimura H, Suda T, Baba H, Tanaka T, Nozawa Y, Koyama N, Takamura M, Kawai H, Yamagiwa S, Aoyagi Y, Terai S (2018) Effective prevention of sorafenib-induced hand–foot syndrome by dried-bonito broth. Cancer Manag Res 10:805–813. https://doi.org/10.2147/CMAR.S159370
Cuesta L, Betlloch I, Toledo F, Latorre N, Monteagudo A (2011) Severe sorafenib-induced hand–foot skin reaction. Dermatol Online J 17(5):14
Degen A, Alter M, Schenck F, Satzger I, Volker B, Kapp A, Gutzmer R (2010) The hand–foot-syndrome associated with medical tumor therapy—classification and management. J Dtsch Dermatol Ges 8(9):652–661. https://doi.org/10.1111/j.1610-0387.2010.07449.x
Dranitsaris G, Vincent MD, Yu J, Huang L, Fang F, Lacouture ME (2012) Development and validation of a prediction index for hand–foot skin reaction in cancer patients receiving sorafenib. Ann Oncol Off J Eur Soc Med Oncol 23(8):2103–2108. https://doi.org/10.1093/annonc/mdr580
Zheng Y, Hua X, Win AK, MacInnis RJ, Gallinger S, Marchand LL, Lindor NM, Baron JA, Hopper JL, Dowty JG, Antoniou AC, Zheng J, Jenkins MA, Newcomb PA (2020) A new comprehensive colorectal cancer risk prediction model incorporating family history, personal characteristics, and environmental factors. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 29(3):549–557. https://doi.org/10.1158/1055-9965.Epi-19-0929
Waters EA, Taber JM, McQueen A, Housten AJ, Studts JL, Scherer LD (2020) Translating cancer risk prediction models into personalized cancer risk assessment tools: stumbling blocks and strategies for success. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 29(12):2389–2394. https://doi.org/10.1158/1055-9965.Epi-20-0861
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13(3):176–181. https://doi.org/10.1016/s1053-4296(03)00031-6
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387. https://doi.org/10.1002/(sici)1097-0258(19960229)15:4%3c361::Aid-sim168%3e3.0.Co;2-4
Ishwaran H, Kogalur UB, Kogalur MUB (2020) Package ‘randomForestSRC’
Ishwaran H (2007) Variable importance in binary regression trees and forests. Electr J Stat 1:519–537. https://doi.org/10.1214/07-Ejs039
Boudou-Rouquette P, Ropert S, Mir O, Coriat R, Billemont B, Tod M, Cabanes L, Franck N, Blanchet B, Goldwasser F (2012) Variability of sorafenib toxicity and exposure over time: a pharmacokinetic/pharmacodynamic analysis. Oncologist 17(9):1204–1212. https://doi.org/10.1634/theoncologist.2011-0439
Naito M, Yamamoto T, Hara S, Shimamoto C, Miwa Y (2017) Hemoglobin value is the most important factor in the development of hand–foot syndrome under the capecitabine regimen. Chemotherapy 62(1):23–29. https://doi.org/10.1159/000445866
Hu S, Chen Z, Franke R, Orwick S, Zhao M, Rudek MA, Sparreboom A, Baker SD (2009) Interaction of the multikinase inhibitors sorafenib and sunitinib with solute carriers and ATP-binding cassette transporters. Clin Cancer Res 15(19):6062–6069. https://doi.org/10.1158/1078-0432.CCR-09-0048
Lupescu A, Shaik N, Jilani K, Zelenak C, Lang E, Pasham V, Zbidah M, Plate A, Bitzer M, Foller M, Qadri SM, Lang F (2012) Enhanced erythrocyte membrane exposure of phosphatidylserine following sorafenib treatment: an in vivo and in vitro study. Cell Physiol Biochem 30(4):876–888. https://doi.org/10.1159/000341465
Balla J, Vercellotti GM, Nath K, Yachie A, Nagy E, Eaton JW, Balla G (2003) Haem, haem oxygenase and ferritin in vascular endothelial cell injury. Nephrol Dial Transplant 18(Suppl 5):v8-12. https://doi.org/10.1093/ndt/gfg1034
Kumar S, Bandyopadhyay U (2005) Free heme toxicity and its detoxification systems in human. Toxicol Lett 157(3):175–188. https://doi.org/10.1016/j.toxlet.2005.03.004
AlV G-S, Arruda MAB, de Freitas MS, Barja-Fidalgo C, Oliveira PL (2002) Neutrophil activation by heme: implications for inflammatory processes. Blood 99(11):4160–4165. https://doi.org/10.1182/blood.V99.11.4160
Tsuchiya N, Narita S, Inoue T, Hasunuma N, Numakura K, Horikawa Y, Satoh S, Notoya T, Fujishima N, Hatakeyama S, Ohyama C, Habuchi T (2013) Risk factors for sorafenib-induced high-grade skin rash in Japanese patients with advanced renal cell carcinoma. Anticancer Drugs 24(3):310–314. https://doi.org/10.1097/CAD.0b013e32835c401c
Révész D, Engelhardt EG, Tamminga JJ, Schramel F, Onwuteaka-Philipsen BD, van de Garde EMW, Steyerberg EW, Jansma EP, De Vet HCW, Coupé VMH (2017) Decision support systems for incurable non-small cell lung cancer: a systematic review. BMC Med Inform Decis Mak 17(1):144. https://doi.org/10.1186/s12911-017-0542-1
Yap YS, Kwok LL, Syn N, Chay WY, Chia JWK, Tham CK, Wong NS, Lo SK, Dent RA, Tan S, Mok ZY, Koh KX, Toh HC, Koo WH, Loh M, Ng RCH, Choo SP, Soong RCT (2017) Predictors of hand–foot syndrome and pyridoxine for prevention of capecitabine-induced hand–foot syndrome: a randomized clinical trial. JAMA Oncol 3(11):1538–1545. https://doi.org/10.1001/jamaoncol.2017.1269
Acknowledgements
This publication uses information obtained from https://www.projectdatasphere.org, which is maintained by Project Data Sphere, LLC. Neither Project Data Sphere, LLC, nor the owners of any information from the web site have contributed to, approved or are in any way responsible for the contents of this publication.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. R.A.M. and M.J.S. are supported by Beat Cancer Research Fellowships from Cancer Council South Australia. A.M.H. is supported by a Postdoctoral Fellowship from the National Breast Cancer Foundation, Australia (PF-17–007). Data access and salary of A.Y.A. were supported by funding from an Australian, Tour de Cure Early Career Research Grant (RSP-155–18/19).
Author information
Authors and Affiliations
Contributions
All authors contributed to study design, interpretation, and preparation the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
R.A.M and M.J.S report investigator-initiated project grants from Pfizer, outside the submitted work. A.Y.A,S.B, W.R,K.S,A.T and A.M.H have no conflicts of interest to disclose.
Ethical approval
Secondary analysis of anonymized individual participant data (IPD) was exempted from review by the Southern Adelaide Local Health Network, Office for Research and Ethics as it was classified as minimal risk research.
Consent to participate
Not applicable. The manuscript is a secondary analysis of anonymized individual participant data (IPD).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abuhelwa, A.Y., Badaoui, S., Yuen, HY. et al. A clinical scoring tool validated with machine learning for predicting severe hand–foot syndrome from sorafenib in hepatocellular carcinoma. Cancer Chemother Pharmacol 89, 479–485 (2022). https://doi.org/10.1007/s00280-022-04411-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-022-04411-9