Abstract
Purpose
The present study evaluates the safety and efficacy of double-plasma filtration (PF) to remove the exceeding pegylated liposomal doxorubicin (PLD) in circulation, thus reducing mucocutaneous toxicity.
Methods
A total of 16 patients with platinum-resistant ovarian cancer were treated with 50 mg/m2 PLD applied in 1-h IV infusion every 28 days. PF was scheduled at 44–46 h post-infusion. The concentration of plasma PLD and non-liposomal doxorubicin (NLD) was monitored with high-performance liquid chromatography at 116 h post-infusion. A non-linear method for mixed-effects was used in the population pharmacokinetic model. The dose fraction of PLD eliminated by the patient prior to PF was compared with the fraction removed by PF. PLD-related toxicity was recorded according to CTCAE v4.0 criteria and compared to historical data. Anticancer effects were evaluated according to RECIST 1.1 criteria.
Results
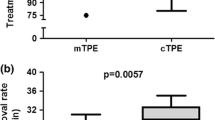
The patients received a median of 3 (2–6) chemotherapy cycles. A total of 53 cycles with PF were evaluated, which removed 31% (10) of the dose; on the other hand, the fraction eliminated prior to PF was of 34% (7). Exposure to NLD reached only 10% of exposure to the parent PLD. PLD-related toxicity was low, finding only one case of grade 3 hand–foot syndrome (6.7%) and grade 1 mucositis (6.7%). Other adverse effects were also mild (grade 1–2). PF-related adverse effects were low (7%). Median progression-free survival (PFS) and overall survival (OS) was of 3.6 (1.5–8.1) and 7.5 (1.7–26.7) months, respectively. Furthermore, 33% of the patients achieved stable disease (SD), whereas that 67% progressed.
Conclusion
PF can be considered as safe and effective for the extracorporeal removal of PLD, resulting in a lower incidence of mucocutaneous toxicity.



Similar content being viewed by others
Abbreviations
- AmPF :
-
Dose (%) eliminated during plasmafiltration
- Amuntil PF :
-
Dose (%) eliminated before plasmafiltration
- AUC:
-
Area under the concentration–time curve
- AUC0−tlast :
-
Area under the concentration–time curve from zero until tlast
- AUCtlast−∞ :
-
Area under the concentration–time curve tlast until infinity
- CHT:
-
Chemotherapy
- CLn :
-
Native (endogenous) clearance (CLuntilPF + CLpostPF)
- CLPF :
-
Extracorporeal clearance
- CLpostPF :
-
PLD clearance after PF termination up to the last plasma concentration at 117 h after PLD administration
- CLuntilPF :
-
Estimated PLD clearance before PF at 45–47 h after PLD administration
- C last :
-
Plasma concentration predicted for the last sampling interval
- C max :
-
Maximum plasma concentration
- CR:
-
Complete response
- CT:
-
Computed tomography
- C Tmax :
-
Peak (Cmax) plasma concentration in tumors
- ECOG:
-
Eastern Cooperative Oncology Group
- EOC:
-
Epithelial ovarian cancer
- EPR:
-
Enhanced permeability and retention effect
- HPLC:
-
High-performance liquid chromatography
- IV:
-
Intravenous
- LVEF:
-
Left ventricular ejection fraction
- MRI:
-
Magnetic resonance imaging
- NLD:
-
Non-liposomal doxorubicin
- NP:
-
Nanoparticles
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PF:
-
Plasmafiltration
- PFI:
-
Platinum-free interval
- PFS:
-
Progression-free survival
- PK:
-
Pharmacokinetic
- PLD:
-
Pegylated liposomal doxorubicin
- PPE:
-
Palmar–plantar erythrodysesthesia (hand–foot syndrome)
- PR:
-
Partial response
- PS:
-
Performance status
- Q12:
-
Inter-compartmental clearance
- QTc:
-
Corrected QT interval
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SD:
-
Stable disease
- SPC:
-
Summary of product characteristics
- t 1/2 :
-
Elimination half-life
- t last :
-
Last sampling interval
- TD:
-
Toxicodynamics
- V 1 :
-
Distribution volume of the central compartment
- V 2 :
-
Distribution volume of the peripheral compartment
- λ z :
-
Terminal slope on the loge (concentration)–time curve
References
EMA (2014) Summary of product characteristics Caelyx (EPAR). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000089/WC500020180.pdf. Accessed 27 Dec 2015
Gabizon AA, Patil Y, La-Beck NM (2016) New insights and evolving role of pegylated liposomal doxorubicin in cancer therapy. Drug Resist Update 29:90–106. https://doi.org/10.1016/j.drup.2016.10.003
Gabizon AA (2001) Pegylated liposomal doxorubicin: metamorphosis of an old drug into a new form of chemotherapy. Cancer Investig 19(4):424–436
Gabizon A, Shmeeda H, Barenholz Y (2003) Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clin Pharmacokinet 42(5):419–436. https://doi.org/10.2165/00003088-200342050-00002
Maeda H, Wu J, Sawa T, Matsumura Y, Hori K (2000) Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 65(1–2):271–284
Fang J, Nakamura H, Maeda H (2011) The EPR effect: unique features of tumor blood vessels for drug delivery, factors involved, and limitations and augmentation of the effect. Adv Drug Deliv Rev 63(3):136–151. https://doi.org/10.1016/j.addr.2010.04.009
Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC (2014) Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv Drug Deliv Rev 66:2–25. https://doi.org/10.1016/j.addr.2013.11.009
Safra T, Muggia F, Jeffers S, Tsao-Wei DD, Groshen S, Lyass O, Henderson R, Berry G, Gabizon A (2000) Pegylated liposomal doxorubicin (Doxil): reduced clinical cardiotoxicity in patients reaching or exceeding cumulative doses of 500 mg/m2. Ann Oncol 11(8):1029–1033
Lyass O, Uziely B, Ben-Yosef R, Tzemach D, Heshing NI, Lotem M, Brufman G, Gabizon A (2000) Correlation of toxicity with pharmacokinetics of pegylated liposomal doxorubicin (Doxil) in metastatic breast carcinoma. Cancer 89(5):1037–1047
Boers-Sonderen MJ, van Herpen CM, van der Graaf WT, Desar IM, van der Logt MG, de Beer YM, Ottevanger PB, van Erp NP (2014) Correlation of toxicity and efficacy with pharmacokinetics (PK) of pegylated liposomal doxorubicin (PLD) (Caelyx(R)). Cancer Chemother Pharmacol 74(3):457–463. https://doi.org/10.1007/s00280-014-2514-9
Mayer LD, Tai LC, Ko DS, Masin D, Ginsberg RS, Cullis PR, Bally MB (1989) Influence of vesicle size, lipid composition, and drug-to-lipid ratio on the biological activity of liposomal doxorubicin in mice. Cancer Res 49(21):5922–5930
Gabizon A, Goren D, Horowitz AT, Tzemach D, Lossos A, Siegal T (1997) Long-circulating liposomes for drug delivery in cancer therapy: a review of biodistribution studies in tumor-bearing animals. Adv Drug Deliv Rev 24(2):337–344. https://doi.org/10.1016/S0169-409X(96)00476-0
Northfelt DW, Dezube BJ, Thommes JA, Miller BJ, Fischl MA, Friedman-Kien A, Kaplan LD, Du Mond C, Mamelok RD, Henry DH (1998) Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi’s sarcoma: results of a randomized phase III clinical trial. J Clin Oncol 16(7):2445–2451
Lorusso D, Di Stefano A, Carone V, Fagotti A, Pisconti S, Scambia G (2007) Pegylated liposomal doxorubicin-related palmar-plantar erythrodysesthesia (‘hand-foot’ syndrome). Ann Oncol 18(7):1159–1164. https://doi.org/10.1093/annonc/mdl477
Eckes J, Schmah O, Siebers JW, Groh U, Zschiedrich S, Rautenberg B, Hasenburg A, Jansen M, Hug MJ, Winkler K, Putz G (2011) Kinetic targeting of pegylated liposomal doxorubicin: a new approach to reduce toxicity during chemotherapy (CARL-trial). BMC Cancer 11:337. https://doi.org/10.1186/1471-2407-11-337
Ngoune R, Contini C, Hoffmann MM, von Elverfeldt D, Winkler K, Putz G (2018) Optimizing antitumor efficacy and adverse effects of pegylated liposomal doxorubicin by scheduled plasmapheresis: impact of timing and dosing. Curr Drug Deliv 15(9):1261–1270. https://doi.org/10.2174/1567201815666180518125839
Martinkova J, Blaha M, Kubecek O, Malakova J, Spacek J, Bezouska J, Krulichova IS, Filip S (2015) Plasmafiltration as a possible contributor to kinetic targeting of pegylated liposomal doxorubicin (PLD) in order to prevent organ toxicity and immunosuppression. Cancer Chemother Pharmacol. https://doi.org/10.1007/s00280-015-2936-z
Blaha M, Martinkova J, Lanska M, Filip S, Malakova J, Kubecek O, Bezouska J, Spacek J (2017) Plasma filtration for the controlled removal of liposomal therapeutics—From the apheretic site of view. Atheroscler Suppl 30:286–293. https://doi.org/10.1016/j.atherosclerosissup.2017.05.022
Robert J (1980) Extraction of anthracyclines from biological fluids for HPLC evaluation. J Liq Chromatogr 3(10):1561–1572. https://doi.org/10.1080/01483918008062796
Bellott R, Pouna P, Robert J (2001) Separation and determination of liposomal and non-liposomal daunorubicin from the plasma of patients treated with Daunoxome. J Chromatogr B Biomed Sci Appl 757(2):257–267
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG, European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92(3):205–216
Harrington KJ, Mohammadtaghi S, Uster PS, Glass D, Peters AM, Vile RG, Stewart JS (2001) Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Cancer Res 7(2):243–254
Gabizon A, Catane R, Uziely B, Kaufman B, Safra T, Cohen R, Martin F, Huang A, Barenholz Y (1994) Prolonged circulation time and enhanced accumulation in malignant exudates of doxorubicin encapsulated in polyethylene–glycol coated liposomes. Cancer Res 54(4):987–992
Hong R-L, Tseng Y-L (2001) Phase I and pharmacokinetic study of a stable, polyethylene-glycolated liposomal doxorubicin in patients with solid tumors. Cancer 91(9):1826–1833. https://doi.org/10.1002/1097-0142(20010501)91:9%3c1826:AID-CNCR24%3e3.0.CO;2-J
La-Beck NM, Zamboni BA, Gabizon A, Schmeeda H, Amantea M, Gehrig PA, Zamboni WC (2012) Factors affecting the pharmacokinetics of pegylated liposomal doxorubicin in patients. Cancer Chemother Pharmacol 69(1):43–50. https://doi.org/10.1007/s00280-011-1664-2
Bally MB, Masin D, Nayar R, Cullis PR, Mayer LD (1994) Transfer of liposomal drug carriers from the blood to the peritoneal cavity of normal and ascitic tumor-bearing mice. Cancer Chemother Pharmacol 34(2):137–146
Norda R, Stegmayr BG (2003) Therapeutic apheresis in Sweden: update of epidemiology and adverse events. Transfus Apher Sci 29(2):159–166. https://doi.org/10.1016/s1473-0502(03)00121-6
Blaha M, Cermanova M, Blaha V, Blazek M, Maly J, Siroky O, Solichova D, Filip S, Rehacek V (2007) Safety and tolerability of long lasting LDL-apheresis in familial hyperlipoproteinemia. Ther Apher Dial 11(1):9–15. https://doi.org/10.1111/j.1744-9987.2007.00450.x
Blaha M, Ptak J, Cap J, Ceeova V, Masin V, Filip S, Blazek M (2009) WAA apheresis registry in the Czech Republic: two centers experience. Transfus Apher Sci 41(1):27–31. https://doi.org/10.1016/j.transci.2009.05.005
Lánská M (2018) Rheopheresis. Clinical importance of rheological, technical and further hemapheretic indicators of effectivity, side-effects and economy. Doctoral thesis
Klingel R, Fassbender C, Heibges A, Koch F, Nasemann J, Engelmann K, Carl T, Meinke M, Erdtracht B (2010) RheoNet registry analysis of rheopheresis for microcirculatory disorders with a focus on age-related macular degeneration. Ther Apher Dial 14(3):276–286. https://doi.org/10.1111/j.1744-9987.2010.00807.x
Schwartz J, Padmanabhan A, Aqui N, Balogun RA, Connelly-Smith L, Delaney M, Dunbar NM, Witt V, Wu Y, Shaz BH (2016) Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the Writing Committee of the American Society for Apheresis: the seventh special issue. J Clin Apher 31(3):149–162. https://doi.org/10.1002/jca.21470
Allen TM, Newman MS, Woodle MC, Mayhew E, Uster PS (1995) Pharmacokinetics and anti-tumor activity of vincristine encapsulated in sterically stabilized liposomes. Int J Cancer 62(2):199–204
Amantea MA, Forrest A, Northfelt DW, Mamelok R (1997) Population pharmacokinetics and pharmacodynamics of pegylated-liposomal doxorubicin in patients with AIDS-related Kaposi’s sarcoma. Clin Pharmacol Ther 61(3):301–311. https://doi.org/10.1016/s0009-9236(97)90162-4
Muggia FM, Hainsworth JD, Jeffers S, Miller P, Groshen S, Tan M, Roman L, Uziely B, Muderspach L, Garcia A, Burnett A, Greco FA, Morrow CP, Paradiso LJ, Liang LJ (1997) Phase II study of liposomal doxorubicin in refractory ovarian cancer: antitumor activity and toxicity modification by liposomal encapsulation. J Clin Oncol 15(3):987–993. https://doi.org/10.1200/jco.1997.15.3.987
Gordon AN, Granai CO, Rose PG, Hainsworth J, Lopez A, Weissman C, Rosales R, Sharpington T (2000) Phase II study of liposomal doxorubicin in platinum- and paclitaxel-refractory epithelial ovarian cancer. J Clin Oncol 18(17):3093–3100. https://doi.org/10.1200/jco.2000.18.17.3093
Gordon AN, Fleagle JT, Guthrie D, Parkin DE, Gore ME, Lacave AJ (2001) Recurrent epithelial ovarian carcinoma: a randomized phase III study of pegylated liposomal doxorubicin versus topotecan. J Clin Oncol 19(14):3312–3322
Rose PG, Maxson JH, Fusco N, Mossbruger K, Rodriguez M (2001) Liposomal doxorubicin in ovarian, peritoneal, and tubal carcinoma: a retrospective comparative study of single-agent dosages. Gynecol Oncol 82(2):323–328. https://doi.org/10.1006/gyno.2001.6272
Lorusso D, Naldini A, Testa A, D’Agostino G, Scambia G, Ferrandina G (2004) Phase II study of pegylated liposomal doxorubicin in heavily pretreated epithelial ovarian cancer patients. May a new treatment schedule improve toxicity profile? Oncology 67(3–4):243–249. https://doi.org/10.1159/000081324
Wilailak S, Linasmita V (2004) A study of pegylated liposomal doxorubicin in platinum-refractory epithelial ovarian cancer. Oncology 67(3–4):183–186. https://doi.org/10.1159/000081315
Chou HH, Wang KL, Chen CA, Wei LH, Lai CH, Hsieh CY, Yang YC, Twu NF, Chang TC, Yen MS (2006) Pegylated liposomal doxorubicin (Lipo-Dox) for platinum-resistant or refractory epithelial ovarian carcinoma: a Taiwanese gynecologic oncology group study with long-term follow-up. Gynecol Oncol 101(3):423–428. https://doi.org/10.1016/j.ygyno.2005.10.027
Mutch DG, Orlando M, Goss T, Teneriello MG, Gordon AN, McMeekin SD, Wang Y, Scribner DR Jr, Marciniack M, Naumann RW, Secord AA (2007) Randomized phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in patients with platinum-resistant ovarian cancer. J Clin Oncol 25(19):2811–2818. https://doi.org/10.1200/jco.2006.09.6735
Ferrandina G, Ludovisi M, Lorusso D, Pignata S, Breda E, Savarese A, Del Medico P, Scaltriti L, Katsaros D, Priolo D, Scambia G (2008) Phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in progressive or recurrent ovarian cancer. J Clin Oncol 26(6):890–896. https://doi.org/10.1200/jco.2007.13.6606
Colombo N, Kutarska E, Dimopoulos M, Bae DS, Rzepka-Gorska I, Bidzinski M, Scambia G, Engelholm SA, Joly F, Weber D, El-Hashimy M, Li J, Souami F, Wing P, Engelholm S, Bamias A, Schwartz P (2012) Randomized, open-label, phase III study comparing patupilone (EPO906) with pegylated liposomal doxorubicin in platinum-refractory or -resistant patients with recurrent epithelial ovarian, primary fallopian tube, or primary peritoneal cancer. J Clin Oncol 30(31):3841–3847. https://doi.org/10.1200/jco.2011.38.8082
Blank N, Laskov I, Kessous R, Kogan L, Lau S, Sebag IA, Gotlieb WH, Rudski L (2017) Absence of cardiotoxicity with prolonged treatment and large accumulating doses of pegylated liposomal doxorubicin. Cancer Chemother Pharmacol 80(4):737–743. https://doi.org/10.1007/s00280-017-3412-8
Bollinger A, Pfister G, Hoffmann U, Franzeck UK (1989) Fluorescence microlymphography in chronic venous incompetence. Int Angiol 8(4 Suppl):23–26
Acknowledgements
The authors thank Dr. Gerhard Pütz (Institute of Clinical Chemistry and Laboratory Medicine, University Medical Center Freiburg) for his invaluable advice. The authors wish to thank Dr. Daniel Díaz, Ph.D. for his kind assistance in English language revision and proofreading.
Funding
The present study was supported by the Grant AZV 16-30366A from the Ministry of Health, CZ and PROGRES Q40/06.
Author information
Authors and Affiliations
Contributions
The authors SF, JM (Jiřina Martínková), MB, JS and OK developed the trial outline, protocols and applied for ethics committee approval; The authors OK, MH, and JS were responsible for patient information and obtaining written consent; OK, MH, and SF were responsible for chemotherapy administration and patient care at the Department of Gynecology, University Hospital in Hradec Králové, while MB was responsible for the extracorporeal treatment at the Apheresis Center, 4th Department of Internal Medicine, University Hospital in Hradec Králové. JM (Jana Maláková) performed the analysis of serum PLD and NLD concentrations; JC was responsible for the model calculations of population pharmacokinetics and statistic evaluation, while JM (Jiřina Martínková) performed data analysis and interpretation of pharmacokinetic parameters; The manuscript was drafted by OK, while the authors JM (Jiřina Martínková), JC, MB, and SF made major contributions and improvements. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kubeček, O., Martínková, J., Chládek, J. et al. Plasmafiltration as an effective method in the removal of circulating pegylated liposomal doxorubicin (PLD) and the reduction of mucocutaneous toxicity during the treatment of advanced platinum-resistant ovarian cancer. Cancer Chemother Pharmacol 85, 353–365 (2020). https://doi.org/10.1007/s00280-019-03976-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-019-03976-2