Abstract
Purpose
Dasatinib (BMS-354825) is a potent, oral multi-targeted kinase inhibitor. It is an effective therapy for patients with imatinib-resistant or -intolerant Ph+ leukemias,. It has demonstrated promising preclinical anti-tumor activity, and is under clinical evaluation in solid tumors. To support the clinical development of dasatinib, we identified a pharmacodynamic biomarker to assess in vivo SRC kinase inhibition, with subsequent evaluation in cancer patients.
Methods
The biomarker, phosphorylated SRC (phospho-SRC), was first identified in human prostate PC-3 tumor cells and peripheral blood mononuclear cells (PBMCs) in vitro. It was further assessed in nude mice bearing PC-3 xenografts. Phospho-SRC[pY418] in tumors and PBMC were measured by western blot analysis, and were quantified by ELISA assays. Dasatinib plasma concentrations were determined using LC/MS/MS.
Results
In PC-3 cells, dasatinib showed dose-dependent anti-proliferative effect, which correlated with the inhibition of phospho-SRC[pY418] and of SRC kinase activity. With a single oral dose of 50 or 15 mg/kg, tumoral phospho-SRC[pY418] was maximally inhibited at 3 h, partially reversed between 7 and 17 h, and completely recovered after 24 h post dose. At 5 mg/kg, tumoral phospho-SRC[pY418] inhibition was less pronounced and recovered more rapidly to baseline level within 24h. Dasatinib (1 mg/kg) resulted in little inhibition. In PBMCs, a similar time course and extent of phospho-SRC[pY418] inhibition was observed. Inhibition of phospho-SRC[pY418] in vivo appeared to correlate with the preclinical in vivo efficacy and PK profiles of dasatinib in mice.
Conclusions
Phospho-SRC[pY418] may potentially be used as a biomarker to enable assessment of target inhibition in clinical studies exploring dasatinib antitumor activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
SRC family kinases are non-receptor intracellular tyrosine kinases that mediate a variety of cellular signaling pathways [1]. SRC kinases are overexpressed in many common tumor types, including colon [2, 3], lung [4], ovarian [5, 6], prostate [7], and pancreatic [8] cancers. Dysregulation of SRC function has been strongly linked to the pathogenesis of human cancers [9]. SRC activity is essential for the stimulation of DNA synthesis, G1 to S phase transition, and proliferation in response to growth factors, such as platelet-derived growth factor (PDGF) [10, 11]. Tumor cells with heightened metastatic potential show higher SRC kinase activity than poorly metastatic cells; mutations in a critical carboxy-terminal tyrosine regulatory region of SRC lead to SRC activation and increased metastasis [11, 12]. SRC family kinases also mediate signaling from many receptor tyrosine kinases, including EGFR, VEGFR, PDGFR, and c-Met [12–14]. Interference of SRC activity leads to mitotic blockade [15]. Therefore, strategies designed to target SRC kinases and other kinase-mediated signaling pathways, either alone or in combination with chemotherapy, could be effective against primary tumor growth as well as metastasis.
Dasatinib is a novel, oral multi-targeted inhibitor of kinases including SRC family kinases. Dasatinib is highly potent, with a biochemical IC50 of 0.8 nM for SRC kinase [16, 17]. It has demonstrated in vivo anti-tumor activity in several human tumor xenograft models [16, 17] and is currently being evaluated in phase I/II trials in a variety of treatment-refractory solid tumors, and has recently received regulatory approval for the treatment of imatinib-resistant CML [16–19]. A common goal of early-phase clinical trials of novel, molecularly targeted agents, such as dasatinib and sunitinib malate, is to provide the proof of concept. To ensure optimal clinical development of these agents, it is critical to prove drug targeting, to determine the extent and duration of target inhibition, and to identify the optimal dose and regimen. Furthermore, it is essential to confirm that modulation of the target correlates with the predicted pharmacological effects (tumor stasis, disease stabilization, and/or tumor reduction). Rigorous determination of the pharmacokinetic (PK) and pharmacodynamic (PD) biomarker relationship drives preclinical efficacy and safety, and subsequent translation of these findings to the clinic streamlines the clinical development process [20–23].
It has been demonstrated that autophosphorylation of tyrosine 418 in the catalytic domain of SRC is required for activation of SRC kinase activity, while dephosphorylation of phosphotyrosine 418 inhibits SRC kinase activity [24]. In a tumor array of 60 human colon carcinomas, 84% of carcinomas had detectable levels of phospho-SRC Tyr418 expression levels [25]. Therefore, phospho-SRC[pY418] may provide a useful marker for inhibition of Src activity in tumors and was evaluated as a potential PD biomarker to assess SRC kinase inhibition by dasatinib in the present study. Specifically, we conducted a series of preclinical studies designed to: (a) evaluate the correlation between the proposed PD biomarker and the target inhibition and antiproliferative effects of dasatinib; (b) determine the efficacious oral exposure range of dasatinib in vivo in a preclinical tumor model; (c) assess the relationship between a PK/PD biomarker and anti-tumor activity, i.e. the in vivo modulation of SRC kinase activity in both tumor and surrogate tissue PBMC at efficacious and inactive doses; (d) explore the utility of phospho-SRC as a PD biomarker to assess in vivo target exposure in patients.
Materials and methods
Chemical reagents and antibodies
Complete protease inhibitor tablets were acquired from Roche Diagnostics (Indianapolis, IN, USA). MicroBCA reagents were from Pierce (Rockford, IL, USA). Rabbit polyclonal anti-phospho-SRC[pY418] antibody and anti-phospho-cortactin[pY421] antibody were purchased from Biosource International Inc. (Camarillo, CA, USA). Mouse monoclonal anti-SRC antibody and anti-cortactin antibody were purchased from Upstate Biotechnology (Lake Placid, NY, USA). Anti-rabbit-IgG and anti-mouse-IgG antibodies conjugated with horseradish peroxidase (HRP) were purchased from BD Bioscience (Lexington, KY, USA). Unless otherwise specified, all other chemicals and reagents were from Sigma (St Louis, MO, USA). Sterile buffers and solutions were obtained from GIBCO/BRL (Carlsbad, CA, USA). Sterile tissue culture ware was obtained from Fisher Scientific Co. (Hanover Park, IL, USA). Cell Preparation Tube™ (CPT) was from BD Biosciences (Franklin Lake, NJ, USA).
Animals
Female nude mice, 5–6 weeks of age, were obtained from Harlan Sprague-Dawley Co. (Indianapolis, IN, USA) and maintained in an ammonia-free environment in a defined and pathogen-free colony. Animals were quarantined for approximately 3 weeks prior to their use for tumor propagation and drug efficacy testing. They were fed food and water ad libitum. All studies were performed in accordance with the regulations of the Animal Care and Use Committee of Bristol–Myers Squibb (BMS) and the American Association for Accreditation of Laboratory Animal Care (AAALAC).
Drug formulation and administration
For oral and intravenous (i.v.) administration, dasatinib was dissolved in a mixture of propylene glycol/water (50:50). The volume of administration was 0.01 mL/g for mice.
In vitro analysis of antiproliferative effects
Cell proliferation assays were conducted in 6-well culture plates. Cells were plated at a density of 1 × 104 cells/well, cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum for 24 h, and then treated with various concentrations of dasatinib for 72 h. Every 24 h, cell growth was determined by counting cell number using a Coulter Channelyzer (Beckman Coulter, Miami, FL). IC50 values were then calculated using XLFit software. The highest concentration of DMSO (drug diluent) added to the cells had no effect on cell proliferation.
In vitro analysis of phospho-SRC inhibition
For phospho-SRC in tumor cells, PC-3 cells were cultured in the same conditions as in proliferation assay and were treated in culture medium containing drug for 1 h at 37°C. Cells were then lysed in ice-cold radio-immunoprecipitation assay (RIPA) buffer containing protease and phosphatase inhibitor cocktails. For phospho-SRC in human PBMCs, drug was spiked in 1 mL of fresh blood collected from apparently healthy donors after proper consent and incubated for 1 h at 37°C. PBMCs were then isolated according to a modified protocol. In brief, the blood was mixed with an equal volume of ice-cold PBS before being laid on top of an equal volume of lymphocyte separation medium (LSM). The layer of PBMCs formed by centrifugation at 400×g at 4°C for 10 min was aspirated. PBMCs were immediately lysed in the buffer containing phosphotase and protease inhibitors and stored in liquid N2 until further analysis by western and/or ELISA for phospho-SRC. Alternatively, a one-step CPT method was used for isolation of PBMC. Briefly, blood was either drawn or placed into CPT tubes. The tubes were centrifuged for 30 min at 1,700×g. Carefully discard the plasma (upper half of the tube, clear solution). Transfer the remaining solution containing monocyte and lymphocyte to a different tube then wash with PBS three times. Harvest the PBMC pellet after centrifuging the solution for 15 min at 300×g, 4°C.
In vivo efficacy testing
PC-3 human prostate tumor fragments (10–20 mg) were subcutaneously implanted into the flanks of nude mice. Tumors were then allowed to grow to the pre-determined size window (between 150 and250 mg, tumors outside the range were excluded) and animals were evenly distributed to various treatment and control groups. Each group of animals was weighed before the initiation of treatment (Wt1) and then again following the last treatment dose (Wt2). Tumor response was determined by measurement of tumor size with a caliper twice a week, until the tumor reached a predetermined target size of 1 g or became necrotic. Tumor weights (mg) were estimated from the formula:
In vivo antitumor activity was determined by the relative percent of tumor growth inhibition (%TGI) of treated versus control animals at different time points using the formula:
where C t = the median tumor weight of control mice (C) at time t; T t = the median tumor weight of treated mice (T) at time t; C0 = the median tumor weight of control mice (C) at the time of the first drug treatment. The minimum antitumor activity was defined as a continuous %TGI ≥ 50% for at least one tumor volume doubling time (TVDT) during any time post drug treatment, which was accompanied by a statistically significant tumor growth delay (T–C value). T–C was defined as the difference in time (days) required for the treated tumors (T) to reach a predetermined target size compared to those of the control group (C); TVDT = median time (days) for control tumors to reach target size–median time (days) for control tumors to reach half the target size. Statistical evaluations of data were performed using Gehan’s generalized Wilcoxon test for comparisons of time to reach tumor target size [26]. Statistical significance was declared at P < 0.05. Treated animals were checked daily for the treatment related toxicity/mortality. When death occurred, the day of death was recorded. Treated mice dying prior to having their tumors reach the target size were considered to have died from drug toxicity. Any treatment group with more than one death (n = 8) caused by drug would be considered to have had excessively toxic treatments and the data were not included in the evaluation of a compound’s antitumor efficacy.
Pharmacokinetics in mice
To characterize the PK parameters of dasatinib, mice (n = 3 per time point) were given a single i.v. (5 mg/kg) or p.o. (1, 5, 15, or 50 mg/kg) dose, and were bled by cardiac puncture 0, 0.08, 0.25, 1, 3, 6, and 24 h (i.v. dosing) or 0, 0.5, 1, 3, 7, 17, and 24 h (p.o. dosing) after treatment. Blood was centrifuged immediately; plasma was collected and frozen at −80°C until analysis by high-performance liquid chromatography/mass spectrometry (LC/MS/MS). In brief, plasma samples were de-proteinized with acetonitrile, the supernatant was analyzed by LC/MS/MS. The HPLC column was a C18-ODS3 column (2 mm × 50 mm, 3 μM particles) (Torrance, CA) maintained at 60°C with a flow rate of 0.5 mL/min. The mobile phase consisted of 5 mM ammonium formate pH 3.75 (A) and acetonitrile (B). The initial mobile phase composition was 87.5% A/12.5% B. After sample injection, the mobile phase was changed to 37.5% A/62.5% B over 2 min, and was held at that composition for 1.5 min. The HPLC was interfaced to a Finnigan LCQ Advantage (Thermo Electron Corp, San Jose, CA, USA) ion-trap mass spectrometer operated in the positive ion electrospray and full MS/MS mode. The standard curve ranged from 2 to 5,000 ng/mL and was fitted with a quadratic regression weighted by reciprocal concentration (1/x). The limit of quantitation (LOQ) for the purposes of this assay was 2 ng/mL.
Pharmacokinetics data analysis was performed by the noncompartmental method using Kinetica (v4.0.2, InnaPhase Corporation, Philadelphia, PA, USA). The maximum plasma concentration (C max) and the time to reach C max (T max) were determined by visually inspecting the profiles of plasma drug concentration versus time. The area under the plasma drug concentration curve (AUC) was estimated by the trapezoidal rule.
Pharmacodynamics in mice
Pharmacodynamics studies were conducted in mice bearing PC-3 human prostate tumors (150–250 mg). Following a single oral administration of dasatinib at 1, 5, 15, or 50 mg/kg, tumors were surgically removed at 0, 0.5, 1, 3, 7, 17, and 24 h and were immediately snap-frozen in liquid nitrogen and stored at −80°C. Prior to analysis, frozen tumor tissues were ground into powder under −80°C and then lysed in ice-cold radio-immunoprecipitation assay buffer containing protease and phosphatase inhibitor cocktails. In the same experiment, blood was sampled at the same time points and PBMCs were isolated and lysed according to the same procedure described in the section of “In vitro analysis of phospho-SRC inhibition” for further analysis of phospho-SRC.
Western blot analysis of phospho-SRC[pY418] and phospho-cortactin[pY421]
The total protein concentration of either tumor or PBMC lysate was determined using the MicroBCA method (Pierce, Rockford, IL, USA). The denatured lysate was further resolved on 12% SDS-PAGE gels and transferred to Immobilon-P polyvinyl membrane (Millipore Corp, Bedford, MA, USA) at constant voltage at 4°C overnight. To detect the phospho-proteins, the membrane was incubated with a rabbit polyclonal anti-phospho-SRC[pY418] or anti-phospho-cortactin[pY421] antibody (1:1,000 dilution) for 30 min at 37°C, followed by incubation with 0.1 μg/mL of anti-rabbit-IgG antibody conjugated with HRP. To detect concentrations of total proteins, the same blot was stripped and blotted with mouse monoclonal anti-SRC or anti-cortactin antibody (1:1,000 dilution) followed by anti-mouse-IgG antibody conjugated with HRP (Millipore Corp, Bedford, MA, USA). Proteins were visualized with western blot chemiluminescence reagent ECL Plus (Amersham Pharmacia Biotech, Piscataway, NJ, USA) as directed by the manufacturer. The molecular sizes of the proteins were estimated by comparison with pre-stained protein precision markers (Bio-Rad Laboratories, Hercules, CA, USA).
Quantitation of phospho-SRC
Concentrations of phospho-SRC were quantitated by an ELISA assay, which was modified from the SRC[pY418] Immunoassay Kit from Biosource International Inc. (Camarillo, CA). In this method, an anti-SRC mouse monoclonal capture antibody was coated to wells of microtiter strips. Phospho-SRC in lysate binds to both the immobilized capture antibody and a rabbit polyclonal anti-SRC[pY418] secondary antibody to form a sandwich.The polyclonal secondary antibody is recognized by anti-rabbit-IgG antibody conjugated with HRP. HRP catalyzes the tetramethylbenzidine/H2O2 reaction and the color formation was measured at an absorbance of 450 nm using a SpectraMax plate reader, which is directly proportional to the concentration of phospho-SRC in the samples. The concentration of phospho-SRC was determined using a calibration curve, prepared in a 10% cell lysis buffer and fitted with a 4-Parameter equation [y = ((A − D)/(1 + (x/C)^B)) + D] in Softmax PRO 4.0. The standard curve range is 1.56–100 units/mL, with read back accuracy ranged from 98.3 to 103% and precision ranged from 2.2 to 10.6% CV (n = 6). The QC samples consisted of cell lysis buffer spiked with recombinant and platelet-derived phospho-SRC and a transfected colon cell line that expresses a significant amount of phospho-SRC. The within-day assay precision ranged from 3.2 to 19.8% CV (n = 6), while between-day assay variation ranged from 9.8 to 25.8% CV (n = 20). Lower limit of quantitation of the assay is 1.56 units/mL. Using this method, we have observed that phospho-Src in human PBMC (isolated from six different donors) is stable for up to 14 weeks when stored at either −80 or −192°C, enabling us to utilize this biomarker in clinical trials.
Results
Correlation of tumor growth inhibition with phospho-SRC inhibition by dasatinib
In PC-3 human prostate tumor cells in vitro, dasatinib showed a dose-dependent inhibition of cell proliferation with an IC50 of 15 nM (Fig. 1a). Western blot with a phospho-specific antibody, anti-SRC[pY418], showed that tumoral phospho-SRC was also inhibited dose-dependently within the same drug concentration range (Fig. 1b). The total protein concentrations of SRC were not changed following dasatinib treatment, suggesting that inhibition of phospho-SRC was attributable primarily to inhibition of autophosphorylation of SRC at the tyrosine residue 418. Phospho-SRC inhibition appeared to correlate with the antiproliferative effect of dasatinib in PC-3 cells (Fig. 1c). To confirm that inhibition of phospho-SRC correlated with inhibition of SRC kinase activity, the phosphorylation status of cortactin, a well-established biological substrate of SRC kinase [27–29], was analyzed with a phospho-specific antibody, anti-cortactin[pY421]. Inhibition of phospho-cortactin paralleled inhibition of phospho-SRC closely, indicating inhibition of SRC kinase activity by dasatinib in PC-3 tumor cells (Fig. 1b). A similar levels of inhibition of phospho-SRC were also inhibited in several other type of tumor cells (data not shown), including breast and colon, suggesting phospho-SRC as a biomarker to assess SRC kinase activity in solid tumors in general, which is consistent with the recent findings in colon cancer cells [25]. Collectively, phospho-SRC appeared to correlate with SRC kinase activity as well as with tumor cell proliferation, and was therefore further evaluated as a biomarker to assess SRC kinase inhibition by dasatinib in vivo.
Inhibition of tumor proliferation (a), SRC kinase inhibition (b) by dasatinib in PC-3 cells in vitro and correlation of SRC kinase inhibition with anti-proliferative effect of dasatinib (c). a PC-3 cells in exponential growth were treated at various concentrations of dasatinib. Each day thereafter, the number of cells was counted for cell growth determination. b Cells in exponential growth were treated with the indicated concentrations of dasatinib for 1 h then lyzed for western blot analysis
Evaluation of phospho-SRC as a biomarker in mice bearing PC-3 human prostate tumor xenografts
The in vivo efficacy of dasatinib (1–50 mg/kg/dose BID × 14) has been fully evaluated in PC-3 tumors grown subcutaneously in nude mice [17]. Dasatinib significantly delayed tumor growth (P < 0.05) and showed similar efficacy across the dose range 15–50 mg/kg/dose. Dasatinib was less efficacious at 5 mg/kg/dose and inactive at 1 mg/kg/dose. Therefore, dasatinib dose levels from 15 to 50 mg/kg/dose were considered to be within the efficacious range; 15 mg/kg/dose appeared to provide optimal antitumor activity in the PC-3 human prostate tumor model.
Phospho-SRC inhibition was evaluated in mice bearing PC-3 tumors following a single oral dose of 1, 5, 15, or 50 mg/kg in the present study. Western blot analysis using anti-SRC[pY418] antibody showed that tumoral phospho-SRC was inhibited dose dependently, but the extent and duration of phospho-SRC inhibition appeared to vary between dose levels of 1–50 mg/kg (Fig. 2a). Inhibition of phospho-SRC was further quantitated by an ELISA assay (Fig. 2b). At 50 and 15 mg/kg, tumoral phospho-SRC was maximally inhibited 3 h after administration, partially reversed between 7 and 17 h after dosing and completely recovered within 24 h of administration. The overall extent of tumoral phospho-SRC inhibition appeared somewhat similar between 50 and 15 mg/kg. At 5 mg/kg, tumoral phospho-SRC was inhibited to a lesser extent and recovered to basal level more rapidly within 24 h. No significant inhibition of tumoral phospho-SRC was observed at 1 mg/kg. In PBMCs, a similar time course and extent of phospho-SRC inhibition was observed (Fig. 2c). The area under the inhibitory curve of phospho-SRC (AUE) in both tumors and PBMCs appeared to follow a similar dose response trend as the in vivo efficacy (TGI) (Fig. 2d). Analysis showed the AUE in tumor and PBMCs are correlated with the TGI shown in Fig. 2e with correlation coefficient of 0.94 and 0.95, respectively.
Inhibition of phospho-SRC in tumor (a, b) and in PBMCs (c) of mice and the correlation with in vivo tumor growth inhibition (d). Mice bearing PC-3 human prostate tumor xenografts were administered a single oral dose of dasatinib at 50, 15, 5, or 1 mg/kg. At the indicated time points, tumors were excised and prepared for western blot analysis. Phospho-SRC inhibition was determined by western blot analysis and was quantitated by ELISA. The in vivo tumor growth inhibition was calculated by the tumor weight between the control and treated mice. e Correlation of area under the phospho-SRC inhibitory curve (AUE) vs in vivo efficacy (TGI)
Pharmacokinetics of dasatinib in mice
To correlate phospho-SRC inhibition with the plasma exposure to dasatinib, PK was investigated in mice treated with a single oral dose of 5, 15, or 50 mg/kg. Upon oral administration, dasatinib was rapidly absorbed with a T max of ∼2 h. The C max was 50.5, 155.3, and 1577.7 ng/mL for 5, 15, and 50 mg/kg, respectively, while the AUC0–24 h was 594.4, 2823.6, and 9412.1 ng × h/mL, respectively. In general, the time course of tumoral phospho-SRC inhibition and recovery appeared to be dose dependent and to correlate directly with the plasma concentrations of dasatinib at 5 and 15 mg/kg (Fig. 3a). The correlation of the AUC with the in vivo efficacy was much less robust (Fig. 3b) (correlation coefficient of 0.72), in contrast to a strong correlation between the AUE of phospho-SRC and the in vivo efficacy (Fig. 2d).
The correlation of the plasma concentrations (a) or AUC (b) with the inhibition of tumoral phospho-SRC in mice following a single po administration of dasatinib. Nude mice were treated orally with 15 and 5 mg/kg of dasatinib. At the indicated time points, plasma and tumors were sampled. Plasma concentrations of dasatinib were determined by LC/MS/MS and phospho-SRC inhibition was quantitated by ELISA. Each datum point represents mean (±SD) from three mice
Comparison of phospho-SRC inhibition between mouse and human PBMCs
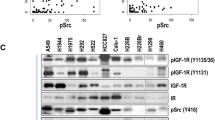
To determine the potential clinical utility of phospho-SRC as a biomarker, inhibition of phospho-SRC by dasatinib in PBMCs was compared side by side in freshly isolated human and mouse blood. Dasatinib appeared to inhibit phospho-SRC dose dependently in both human and mouse PBMCs (Fig. 4a). The phospho-SRC levels in PBMCs were further quantitated with the ELISA assay, a similar inhibitory potency and kinetics for phospho-SRC were observed between human and mouse PBMCs (Fig. 4b). Analysis showed phospho-SRC inhibition is correlated in human and mouse PBMCs with a correlation coefficient of 0.99. The EC50, the concentration required to achieve 50% phospho-SRC inhibition in human PBMCs, was ∼25.8 nM (∼12.5 ng/mL) estimated by a regression analysis using the inhibitory Emax model. In a separate experiment, inhibition of phosphorylation of cortactin in PBMCs, was also investigated and was found to parallel inhibition of phospho-SRC (data not shown), indicating the causal relationship of phospho-SRC level with SRC kinase activity in PBMCs, which was similarly shown in PC-3 tumor cells in the present study.
Discussion
Phospho-SRC was proposed as a biomarker to assess SRC kinase targeting based on in vitro observations in tumor cells in our laboratory as well as other investigator laboratory [25]. It appeared that inhibition of tumoral phospho-SRC has a causal relationship with antiproliferative effect as well as inhibition of tumoral SRC kinase activity in PC-3 cells (Fig. 1). Similar relationship was also observed in several other tumor types, including colon and breast cancer, suggesting that phospho-SRC could be useful to assess SRC kinase inhibition in multiple solid tumor types which are usually seen in phase I dose escalation study. Furthermore, phospho-SRC inhibition in surrogate tissue PBMCs showed a similar relationship with inhibition of SRC kinase activity. These observations confirmed that phospho-SRC was an attractive biomarker candidate, warranting further in vivo evaluation in both preclinical models and cancer patients. Inhibition of phospho-SRC was subsequently evaluated in vivo in mice bearing PC-3 tumor xenografts at both efficacious and inactive doses (Fig. 2). Interestingly, the time course and extent of inhibition of phospho-SRC was similar between tumor and PBMCs, implying that measurement of phospho-SRC levels in PBMCs may provide information on tumoral phospho-SRC inhibition in the clinic. This is particularly relevant when phospho-SRC in PBMCs is used as a biomarker for clinical studies, in which availability of tumor biopsies is usually limited. When the biomarker response (inhibition of phospho-SRC) was compared with tumor growth inhibition by dasatinib, phospho-SRC levels in both tumors and PBMCs correlated well with the preclinical in vivo efficacy (Fig. 2d, e). This suggests that phospho-SRC, as a mechanism-based biomarker, may have the potential to correlate with the antitumor activity of dasatinib in cancer patients. This hypothesis is currently being tested in phase II trials.
It is of great interest and importance to evaluate if and how these preclinical observation can be translated into the clinical evaluation of dasatinib. The relationship between dasatinib pharmacokinetic exposures and the in vivo efficacy appears to be less direct and less robust than in in vitro models. A clear discrepancy has been observed between the systemic exposure and the antitumor activity of dasatinib, especially for high dose levels (Fig. 3b). This implies that the target (SRC kinase) may be completely inhibited at dose levels or exposures that are not sufficient to saturate the systemic clearance of dasatinib. Alternatively, clinical efficacy may not correlate with drug exposures, which is routinely determined in early-phase studies. Clinical scenarios are probably much more complicated than those observed in animal models. However, our study supports the notion that the optimal biological dose for molecularly targeted therapies can be better defined based on the mechanism-based biomarkers than the tolerability in phase 1 dose-escalation studies.
In our study, the inhibitory potency and kinetics of dasatinib were similar in human and mouse PBMCs (Fig. 4), suggesting that phospho-SRC has considerable potential as a biomarker in both clinical as well as preclinical settings. In cancer patients, dasatinib significantly inhibits phospho-SRC in PBMCs, implying modulation of SRC kinase activity in PBMCs, and probably in tumors also following dasatinib therapy, the inhibitory EC50 of phospho-SRC, the plasma concentration of dasatinib for 50% phospho-SRC inhibition, was estimated as 8–10 ng/mL in PBMCs of cancer patients who received dasatinib. When compared with the plasma concentrations of dasatinib in cancer patients, dasatinib had achieved plasma concentrations above the inhibitory EC50 for ∼16 h at dose >90 mg BID (Fig. 5) [30], which was considered to be the minimally required for optimal efficacy in the preclinical model. The apparent modulation by dasatinib of SRC kinase activity in PBMCs may also apply to tumors, although differences in the degree of modulation are possible due to tumor heterogeneity. The correlation of phospho-SRC inhibition between PBMCs and tumor is currently being evaluated in a clinical study. Furthermore, it remains to be seen if and how phospho-SRC inhibition correlates with clinical benefits in ongoing phase II studies.
Pharmacokinetics of dasatinib in cancer patients at steady state. Dasatinib was administered orally at 90 mg BID or 180 mg QD. Plasma samples were assayed for dasatinib by a validated liquid chromatography tandem mass spectrometry (LC/MS/MS) method. For BID regimen, the plasma curve post second daily dose was assumed to be identical to the one post the first daily dose based on no essential accumulation between day and day 29 (steady state) (30)
The emergence of small molecule tyrosine kinase inhibitors into clinical development presents the opportunity to optimize dosing and scheduling based on a desired level and duration of target inhibition (and subsequent biological effect) rather than more traditional identification of a maximum tolerated dose (MTD) for chemotherapeutic agents. To adopt this approach, the PK/PD biomarker relationship linking target modulation and anti-tumor efficacy in preclinical tumor models must be elucidated to expedite clinical evaluation. Analysis of signal transduction pathways in tumors from xenograft models provides a useful approach to determine the kinetics and magnitude of target inhibition associated with biological response/efficacy, and the drug plasma concentrations needed to achieve this objective.
The present study provides evidence that phospho-SRC has the potential as a biomarker for assessing SRC targeting, which could provide a rapid proof of concept that dasatinib can inhibit SRC kinase when given to patients in early-phase studies. Extensive preclinical or translational PK/PD biomarker studies have been presented for several molecularly targeted therapies that have undergone clinical evaluation, including trastuzumab (Herceptin), gefitinib (Iressa), imatinib (Gleevec), and sunitinib malate (Sutent) [20, 31–35]. In all cases, biomarkers indicative of disease mechanisms effectively helped to address central issues, such as rapid proof of concept and selection of the optimal dose and regimen. The experience with those drugs helped developing the strategy for the clinical development of the novel SRC kinase inhibitor, dasatinib.
Biomarkers may be essential predictive factors to select patients for molecularly targeted therapy. The clinical benefit of trastuzumab is limited to patients whose tumors demonstrate amplification of HER2 [36] and imatinib is effective only in patients with Ph+ CML [37]. Careful selection of patient populations for early clinical studies of dasatinib may influence the likelihood of achieving proof of concept and will be critical in maximizing efficacy and tolerability. Identification of tumor types in which the target plays a pivotal role will also influence the successful application of targeted therapies [32, 34]. In addition, pharmacogenomic and proteomic profiling in different tumor types appears to be a promising approach to identifying gene or protein biomarkers predictive of responsive patient populations. We have discovered a set of gene and protein biomarkers predicting treatment response to dasatinib with a panel of sensitive and resistant tumors using pharmacogenomic and proteomic approaches [38]. The validity of these biomarkers is currently being tested in clinical studies.
In summary, we believe that effective development of novel, molecularly targeted agents requires determination of the optimal clinical exposure and regimen for phase II/III studies using an array of biomarkers, including target exposure biomarkers and patient selection biomarkers, in combination with efficacy and safety profiles defined in phase I trials.
References
Brown MT, Cooper JA (1996) Regulation, substrates and functions of src. Biochim Biophys Acta 1287:121–149
Windham TC, Parikh NU, Siwak DR, Summy JM, McConkey DJ, Kraker AJ, Gallick GE (2002) Src activation regulates anoikis in human colon tumor cell lines. Oncogene 21:7797–7807
Haier J, Gallick GE, Nicolson GL (2002) Src protein kinase pp60c-src influences adhesion stabilization of HT-29 colon carcinoma cells to extracellular matrix components under dynamic conditions of laminar flow. J Exp Ther Oncol 2:237–245
Mazurenko NN, Kogan EA, Zborovskaya IB, Kisseljov FL (1992) Expression of pp60c-src in human small cell and non-small cell lung carcinomas. Eur J Cancer 28:372–377
Budde RJ, Ke S, Levin VA (1994) Activity of pp60c-src in 60 different cell lines derived from human tumors. Cancer Biochem Biophys 14:171–175
Wiener JR, Nakano K, Kruzelock RP, Bucana CD, Bast RC Jr, Gallick GE (1999) Decreased Src tyrosine kinase activity inhibits malignant human ovarian cancer tumor growth in a nude mouse model. Clin Cancer Res 5:2164–2170
Nam S, Kim D, Cheng JQ, Zhang S, Lee JH, Buettner R, Mirosevich J, Lee FY, Jove R (2005) Action of the Src family kinase inhibitor, dasatinib (BMS-354825), on human prostate cancer cells. Cancer Res 65:9185–9189
Lutz MP, Esser IB, Flossmann-Kast BB, Vogelmann R, Luhrs H, Friess H, Buchler MW, Adler G (1998) Overexpression and activation of the tyrosine kinase Src in human pancreatic carcinoma. Biochem Biophys Res Commun 243:503–508
Frame MC (2002) Src in cancer: deregulation and consequences for cell behaviour. Biochim Biophys Acta 1602:114–130
Barone MV, Courtneidge SA (1995) Myc but not Fos rescue of PDGF signalling block caused by kinase-inactive Src. Nature 378:509–512
Irby RB, Mao W, Coppola D, Kang J, Loubeau JM, Trudeau W, Karl R, Fujita DJ, Jove R, Yeatman TJ (1999) Activating SRC mutation in a subset of advanced human colon cancers. Nat Genet 21:187–190
Mao W, Irby R, Coppola D, Fu L, Wloch M, Turner J, Yu H, Garcia R, Jove R, Yeatman TJ (1997) Activation of c-Src by receptor tyrosine kinases in human colon cancer cells with high metastatic potential. Oncogene 15:3083–3090
Biscardi JS, Maa MC, Tice DA, Cox ME, Leu TH, Parsons SJ (1999) c-Src-mediated phosphorylation of the epidermal growth factor receptor on Tyr845 and Tyr1101 is associated with modulation of receptor function. J Biol Chem 247:8335–8343
Luttrell DK, Lee A, Lansing TJ, Crosby RM, Jung KD, Willard D, Luther M, Rodriguez M, Berman J, Gilmer TM (1994) Involvement of pp60c-src with two major signaling pathways in human breast cancer. Proc Natl Acad Sci USA 91:83–87
Roche S, Fumagalli S, Courtneidge SA (1994) Requirement for Src family protein tyrosine kinases in G2 for fibroblast cell division. Science 269:1567–1569
Luo FR, Yang Z, Camuso A, Smykla R, McGlinchey K, Fager K, Flefleh C, Castaneda S, Inigo I, Kan D, Wen M-L, Kramer R, Blackwood-Chirchir A, Lee FY (2006) Dasatinib (BMS-354825) pharmacokinetics and pharmacodynamic biomarkers in animal models predict optimal clinical exposure. Clin Cancer Res 12:7180–7186
Lee FY, Lombardo L, Camuso A, Castaneda S, Fager K, Flefleh C, Inigo I, Johnson K, Kan D, McGlinchey K, Pang S, Peterson R, Wen M-L, Wild R, Fairchild C, Wong T, Borzilleri R, Luo FR, Kramer R (2005) BMS-354825 potently inhibits multiple selected oncogenic tyrosine kinases and possesses broad-spectrum antitumor activities in vitro and in vivo. In: AACR 96th annual meeting
Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL (2004) Overriding imatinib resistance with a novel ABL kinase inhibitor. Science 305:399–401
Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R, Cortes J, O’Brien S, Nicaise C, Bleickardt E, Blackwood-Chirchir A, Iyer V, Chen TT, Huang F, Decillis AP, Sawyers CL (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 345:2531–2541
Baselga J, Rischin D, Ranson M, Calvert H, Raymond E, Kieback DG, Kaye SB, Gianni L, Harris A, Bjork T, Averbuch SD, Feyereislova A, Swaisland H, Rojo F, Albanell J (2002) Phase I safety, pharmacokinetic, and pharmacodynamic trial of ZD1839, a selective oral epidermal growth factor receptor tyrosine kinase inhibitor, in patients with five selected solid tumor types. J Clin Oncol 20:4292–4302
Park JW, Kerbel RS, Kelloff GJ, Barrett JC, Chabner BA, Parkinson DR, Peck J, Ruddon RW, Sigman CC, Slamon DJ (2004) Rationale for biomarkers and surrogate end points in mechanism-driven oncology drug development. Clin Cancer Res 10:3885–3896
Fox E, Curt GA, Balis FM (2002) Clinical trial design for target-based therapy. Oncologist 7:401–409
Wolf M, Swaisland H, Averbuch S (2004) Development of the novel biologically targeted anticancer agent gefitinib: determining the optimum dose for clinical efficacy. Clin Cancer Res 10:4607–4613
Roskoski R Jr (2005) Src kinase regulation by phosphorylation and dephosphorylation. Biochem Biophys Res Commun 331:1–14
Serrels A, Macpherson IR, Evans TR, Lee FY, Clark EA, Sansom OJ, Ashton GH, Frame MC, Brunton VG (2006) Identification of potential biomarkers for measuring inhibition of Src kinase activity in colon cancer cells following treatment with dasatinib. Mol Cancer Ther 5:3014–3022
Gehan EA (1965) A generalized two-sample Wilcoxon test for doubly censored data. Biometrika 52:650–653
Kanner SB, Reynolds AB, Vines RR, Parsons JT (1990) Monoclonal antibodies to individual tyrosine-phosphorylated protein substrates of oncogene-encoded tyrosine kinases. Proc Natl Acad Sci USA 87:3328–3332
Wu H, Reynolds AB, Kanner SB, Vines RR, Parsons JT (1991) Identification and characterization of a novel cytoskeleton-associated pp60src substrate. Mol Cell Biol 11:5113–5124
Kanner SB, Reynolds AB, Wang HC, Vines RR, Parsons JT (1991) The SH2 and SH3 domains of pp60src direct stable association with tyrosine phosphorylated proteins p130 and p110. Embo J 10:1689–1698
Luo FR, Barrett Y, Wu C, Ji P, Palme H, McCann B, Rhyne P, Clark E, He K, Bleickardt E, Blackwood-Chirchir A (2006) Dasatinib (BMS-354825) pharmacokinetics correlate with pSRC pharmacodynamics in phase I studies of patients with cancer (CA180002, CA180003). J Clin Oncol 24:3046–3046
Mendel DB, Laird AD, Xin X, Louie SG, Christensen JG, Li G, Schreck RE, Abrams TJ, Ngai TJ, Lee LB, Murray LJ, Carver J, Chan E, Moss KG, Haznedar JO, Sukbuntherng J, Blake RA, Sun L, Tang C, Miller T, Shirazian S, McMahon G, Cherrington JM (2003) In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors: determination of a pharmacokinetic/pharmacodynamic relationship. Clin Cancer Res 9:327–337
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM, Lydon NB, Kantarjian H, Capdeville R, Ohno-Jones S, Sawyers CL (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344:1031–1037
Baselga J, Norton L, Albanell J, Kim YM, Mendelsohn J (1998) Recombinant humanized anti-HER2 antibody (Herceptin) enhances the antitumor activity of paclitaxel and doxorubicin against HER2/neu overexpressing human breast cancer xenografts. Cancer Res 58:2825–2831
Baselga J, Tripathy D, Mendelsohn J, Baughman S, Benz CC, Dantis L, Sklarin NT, Seidman AD, Hudis CA, Moore J, Rosen PP, Twaddell T, Henderson IC, Norton L (1996) Phase II study of weekly intravenous recombinant humanized anti-p185HER2 monoclonal antibody in patients with HER2/neu-overexpressing metastatic breast cancer. J Clin Oncol 14:737–744
Lipton A, Ali SM, Leitzel K, Demers L, Chinchilli V, Engle L, Harvey HA, Brady C, Nalin CM, Dugan M, Carney W, Allard J (2002) Elevated serum Her-2/neu level predicts decreased response to hormone therapy in metastatic breast cancer. J Clin Oncol 20:1467–1472
Mass RD, Press MF, Anderson S, Cobleigh MA, Vogel CL, Dybdal N, Leiberman G, Slamon DJ (2005) Evaluation of clinical outcomes according to HER2 detection by fluorescence in situ hybridization in women with metastatic breast cancer treated with trastuzumab. Clin Breast Cancer 6:240–246
Cortes J, Talpaz M, O’Brien S, Jones D, Luthra R, Shan J, Giles F, Faderl S, Verstovsek S, Garcia-Manero G, Rios MB, Kantarjian H (2005) Molecular responses in patients with chronic myelogenous leukemia in chronic phase treated with imatinib mesylate. Clin Cancer Res 11:3425–3432
Reeves K, Han X, Shaw PM, Clark E, Peterson R, Johnston K, Fairchild C, Wu Q, Platero S, Wong TW, Kan D, Inigo I, Castenada S, Lee FY, Huang F (2005) Identification of Pharmacogenomic Markers for Predicting Sensitivity to BMS-354825, a SRC/ABL Kinase Inhibitor. In: 41st ASCO annual meeting
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. R. Luo and Y. C. Barrett contributed equally to this work.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Luo, F.(., Barrett, Y.C., Yang, Z. et al. Identification and validation of phospho-SRC, a novel and potential pharmacodynamic biomarker for dasatinib (SPRYCEL™), a multi-targeted kinase inhibitor. Cancer Chemother Pharmacol 62, 1065–1074 (2008). https://doi.org/10.1007/s00280-008-0699-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-008-0699-5