Abstract
REHem-AR was created in 2013. The progressive implementation of neonatal screening for haemoglobinopathies in Spanish autonomous communities where the registry had not been implemented, as well as the addition of new centres during this period, has considerably increased the sample of patients covered. In this study, we update our previous publication in this area, after a follow-up of more than 5 years. An observational, descriptive, multicentre and ambispective study of adult and paediatric patients with haemoglobinopathies and rare anaemias registered in REHem was performed. The data are from a cross-sectional analysis performed on 1 June, 2023. The study population comprised 1,756 patients, of whom 1,317 had SCD, 214 had thalassaemia and 224 were diagnosed with another condition. Slightly more than one third of SCD patients (37%) were diagnosed based on neonatal bloodspot screening, and the mean age at diagnosis was 2.5 years; 71% of thalassaemia patients were diagnosed based on the presence of anaemia. Vaso-occlusive crisis and acute chest syndrome continue to be the most frequent complications in SCD. HSCT was performed in 83 patients with SCD and in 50 patients with thalassaemia. Since the previous publication, REHem-AR has grown in size by more than 500 cases. SCD and TM are less frequent in Spain than in other European countries, although the data show that rare anaemias are frequent within rare diseases. REHem-AR constitutes an important structure for following the natural history of rare anaemias and enables us to calculate investment needs for current and future treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Haemoglobinopathies are a clinically heterogeneous group of inherited diseases caused mainly by mutations and/or deletions in globin genes. The most clinically significant mutations are those affecting α and β [1] globins. Haemoglobinopathies are classified into thalassaemic haemoglobinopathies, or thalassaemias, in which there is a deficit in the synthesis of the globin affected, and structural haemoglobinopathies, in which there are changes in the amino acid sequence and whose main subgroup is characterised by haemoglobin S, or sickle cell disease (SCD). Depending on the mutation acquired, the other structural haemoglobinopathies identified include haemoglobin C, D-Punjab and O-Arab disease. We can also find mixed forms that combine characteristics of both groups, such as haemoglobin E or haemoglobin Lepore trait. The pathophysiology and clinical pattern of each disease can be very broad, as reported elsewhere [2].
The annual number of newborns with SCD, estimated at 305,800 worldwide in 2010, is likely to increase by about one third by 2050 [3,4,5].
In Madrid, the neonatal prevalence of haemoglobinopathy is 5.57 per 1,000 births; in the case of SCD, it is 1 per 6,250 births [6]. In other countries, such as the UK, between 12,500 and 15,000 people are estimated to have SCD [7].
Since the creation in 2013 of the Spanish Registry of Haemoglobinopathies and Rare Anaemias (REHem-AR), the demographic and clinical characteristics of haemoglobinopathies have been recorded. The latest publication on this subject dates from 2019, with data updated up to 31 December 2017 [6]. The progressive implementation of neonatal screening for SCD throughout Spain, as well as the inclusion of new centres in the registry during this period, has considerably increased the sample of patients. In the present study, we update the data provided by the registry, after a follow-up of more than 5 years.
Material and methods
The REHem-AR, which was launched in January 2013 and is monitored annually, collects data on patients with clinically significant rare anaemias in Spain, including transfusion-dependent thalassaemias (TDT), non-transfusion-dependent thalassaemias (NTDT), SCD and other clinically significant haemoglobinopathies, as well as enzymopathies.
This observational, descriptive, multicentre and ambispective study includes adult and paediatric patients with haemoglobinopathies and other rare anaemias registered in REHem-AR. The registry collected patients' clinical data retrospectively at the date of creation in 2013. New patients are registered and followed prospectively if they are registered at birth, and retrospectively if they are registered at an older age. Patient information is updated on an annual basis.
The data presented in the present study are from a cross-sectional analysis performed on 1 June 2023 and update those reported in the previous 2017 publication. The study population comprises patients of any age who made at least 1 visit to any paediatric or adult haematology unit in Spain. Inclusion in the cohort was at birth if neonatal screening was available or at the date of diagnosis if performed later.
Informed consent was obtained from all patients or their legal guardians in accordance with the Declaration of Helsinki. For patients who died or were lost to follow-up before initiation of the study, data were collected retrospectively from the corresponding medical records.
The registry and the data analysis were approved by the Ethics Committee of each participating centre, by the Office of the Public Prosecutor for Minors and by the Spanish Data Protection Agency. The Spanish Agency of Medicines and Medical Devices was informed of our intention to perform the study, which was sponsored by the Spanish Society of Paediatric Haematology and Oncology (SEHOP).
The different variables were entered online by each of the treating physicians and are expressed as median and interquartile range. The items entered included identification data, date of birth, sex, diagnosis and date of diagnosis, reason for diagnosis, country of birth, genotype, imaging test results, clinical complications, treatments and follow-up data (alive or deceased, lost to follow-up and causes). Potentially duplicate records were examined and excluded based on the patient identification code of the National Health System, when available. In certain cases, the combination of the patient’s name, sex, date of birth and personal contact with the treating physician was necessary to identify duplicates.
Definition of variables
SCD comprises a group of chronic haemoglobinopathies characterised by haemolysis and intermittent episodes of vascular occlusion causing tissue ischaemia and acute and chronic organ dysfunction. It is a genetic, autosomal recessive disease defined by the presence of haemoglobin S (HbS) in erythrocytes, and our registry contains homozygous or compound heterozygous individuals with several possible genotypes, namely, SS, SC, Sβ+, Sβ0 and SD [8].
Thalassaemias result from decreased or absent synthesis of 1 or more globin chains that are part of the haemoglobin structure. The phenotypic classification of thalassaemia patients included in our registry into TDT or NTDT was made by the researchers who follow the patients up, with no defined criteria. TDT manifests in early childhood with severe anaemia or significant complications requiring serial transfusion, while NTDT individuals do not require regular transfusions, although they may require them sporadically. Both groups include patients with HbE/β-thalassaemia and α-thalassaemia (haemoglobin H disease).
Statistical analysis
The analysis was performed using R 4.3.0 (R Core Team, Vienna, Austria).
Quantitative variables were expressed as median and interquartile range; qualitative variables were reported as absolute and relative frequencies. Death-free survival was studied using the Kaplan–Meier method, after stratifying by the different pathological and clinical variables. Statistical significance was set at p < 0.05.
Results
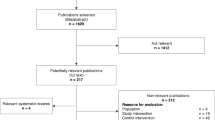
A total of 1,874 patients were collected from 80 participating hospitals throughout Spain. We excluded 118 records owing to duplication, leaving a final analysable sample of 1,756 patients.
Among the participating centres, 1 centre contributed more than 400 patients, 1 centre more than 300 patients, 1 centre more than 150 patients, 2 centres between 50 and 100 patients and the remaining 75 centres fewer than 50 patients.
There were 1,317 cases of SCD, 214 cases of thalassaemia and 224 cases with other diagnoses.
Sickle cell disease
A total of 1,317 patients with SCD were registered (75% of the total sample), with a male/female ratio of 1.09 (52% male, 48% female). The most frequent genotype found was SS (78%), followed by SC (13.5%), Sβ0 (4%), Sβ+ (4%) and SD (0.5%).
Sixty-seven percent of patients were aged under 18 years, with Spain as the country of birth for most of them (62.5%), followed by Equatorial Guinea (9%).
The breakdown of the patients' countries of birth, as well as those of their parents, is shown in Fig. 1.
Diagnosis was based on neonatal screening in 37%, clinical anaemia in 24%, pain episodes in 15% and the family study in 8%. The median age at diagnosis was 2.5 years (0.0–3.0). In addition, 8% had glucose-6-phosphate dehydrogenase deficiency.
The centres with the highest number of patients with SCD were the Gregorio Marañón, Vall d'Hebrón and Sant Joan de Déu hospitals, with 25.6%, 5.4% and 8.9%, respectively, making Madrid and Catalonia the autonomous communities with the highest number of affected persons registered.
The clinical and demographic characteristics are summarised in Table 1.
Stroke risk was assessed annually using transcranial Doppler ultrasound (TCD) in 55% of patients with SCD and the SS, Sβ0, Sβ+ or SD genotype aged 2 to 16 years between 1 January 2019 and 1 June 2023 (the vast majority, annually). TCD was not performed in the other 45% of patients in this age range, in some cases because the patient had received a transplant (16%) and in others because the patient was included in a long-term transfusion programme (29%).
Since our last publication in 2017, an annual average of 13 patients had a pathological outcome on TCD. The highest percentage was in 2018, with a pathological outcome in 20 of the 187 patients (10.5%) aged 2–16 years who underwent TCD in that year.
During the same period, 220 patients (34.5%) with SCD and genotype SS, Sβ0, Sβ+ or SD underwent brain magnetic resonance imaging, with an abnormality detected in 45% (100 patients). Lacunar infarcts were the most frequent (60%), followed by moyamoya-type vasculopathy (10%). During recent years, 19% had a cerebrovascular accident, and neurocognitive dysfunction was detected in 69%.
The annual incidence of complications of SCD since our last publication in 2017 is summarised in Fig. 2, according to the total number of patients in follow-up each year.
Incidence of the most frequent complications secondary to sickle cell disease (SCD) since our last publication in 2017. Data are expressed as a percentage over the total number of patients with SCD in follow-up that year. Vaso-occlusive crises were defined at the discretion of each investigator (they have been homogeneously defined in the registry subsequent to this analysis). Kidney disease includes proteinuria, kidney failure and nocturnal enuresis. Lung disease includes restrictive disease, obstructive disease (asthma), mixed disease, hypoxaemia and sleep apnoea-hypopnoea syndrome. Neurological complications include cerebrovascular accident (CVA) and neurocognitive abnormalities other than the sequelae of symptomatic CVA. Liver disease includes haemosiderosis or viral hepatitis. *Onset of chronic complications (e.g. nephropathy, biliary lithiasis) during the year in question. Not included if already present
Regarding treatment, 70.5% (809) of patients with SCD and genotype SS, Sβ0, Sβ+ or SD started antibiotic prophylaxis with penicillin at some point; this percentage increased to 93.5% in patients aged between 2 months and 5 years of age. Currently, 78.5% of all those who started penicillin continue to receive it (5.5% splenectomised), with an increase in age (28.5% of patients between 5 and 10 years of age, 43.5% of patients between 10 and 20 years of age).
Vitamin D prophylaxis was prescribed at some point for osteopenia in 52% of patients, and 90% were still receiving it at the time of this analysis.
Hydroxyurea was initiated in 686 patients (52%), of whom 81% continue to receive the drug, with a median age at initiation of 5 years (2.0–9.0) and a median duration of 2 years. Excluding patients with SC and Sβ + genotype, the proportion of SCD patients receiving hydroxyurea is 60%.
Ten percent of patients (133) joined a long-term hypertransfusion programme. Of these, 46.5% continue to receive transfusions. The median age of onset was 7 years (4.0–11.0), and the median duration of the programme was 1 year (0.0–2.0).
Chelation therapy was initiated in 7.5% of patients, with deferasirox being the most frequently used drug (93.5%), followed by deferoxamine (15%). The median age at initiation of chelation therapy was 9 years (6.0–14.0), with a median duration of 1 year (0.0–2.0).
A total of 51 patients (4%) underwent splenectomy at a median age of 4 years (2.0–8.0), and 75 patients (6%) underwent cholecystectomy. Ten per cent of the patients underwent another type of surgical intervention, such as adenotonsillectomy or joint replacement. Ten per cent (133 cases) required a central venous catheter (CVC).
Haematopoietic stem cell transplantation (HSCT) was performed in 83 patients (6.5%) at a median age of 7 years (4.0–10.0). Of these, 62% had complete chimerism and 29% had mixed chimerism. Five patients (6%) experienced graft failure. Seven patients (8%) subsequently developed chronic graft-versus-host disease (GvHD).
The overall survival (death-free) was 99% (95% CI 98–100%) at 10 years, 97% (95% CI 96–99%) at 30 years and 95% (95% CI 92–99%) at 60 years. Survival curves for both SCD and thalassaemia are shown in Fig. 3.
Thirty-nine percent of the patients in the sample were lost to follow-up owing to emigration to another country (26%), follow-up changed to another centre (42%), and unknown causes (30%).
Twenty-seven patients (2%) died.
As for SARS-CoV-2 infection, a total of 119 patients (9%) were diagnosed with COVID-19. Thirty-eight patients (32%) required admission, and up to 79.5% required empirical intravenous antibiotic therapy. There were no COVID-19–attributable deaths.
Thalassaemia
The registry included 214 patients with thalassaemia (12% of the total sample), of whom 115 (54%) had TDT and 99 had NTDT. Of the patients with NTDT, 28% had haemoglobin H disease. The male/female ratio was 1.01 (50.5% male, 49.5% female). The centres with the highest number of patients were the Vall d'Hebrón, Virgen del Rocío, La Fe and Gregorio Marañón hospitals, with 25.9%, 12.4%, 11.4% and 10.3%, respectively, making Catalonia, Andalusia, Valencia and Madrid the autonomous communities with the highest number of registered cases of thalassaemia.
Spain was the country of birth for most cases, with 61% of the total, followed by Morocco, with 7%. Paediatric patients (< 18 years) accounted for 47% of cases. The breakdown of the countries of birth of the patients, as well as that of their parents, is shown in Fig. 4.
The main reason for diagnosis was clinical anaemia (71%), followed by an abnormal neonatal screening result (10%) and a family study (8.5%); 10% were diagnosed for other reasons. Considering TDT cases diagnosed in the last 5 years (11 patients), 54.5% were diagnosed following neonatal screening, while among cases diagnosed before 2018, the majority (84.5%) were diagnosed via the anaemia clinic.
Positive hereditary thrombophilia findings were recorded at diagnosis in 4% of cases.
Clinical and demographic characteristics are summarised in Table 1.
In terms of treatment, 90% of patients with TDT without primary parahyperthyroidism received chelation therapy at some point during follow-up, as did 30% of patients with NTDT. In both groups, deferasirox was the most frequently used drug (89%), followed by deferoxamine (46.5%) and deferiprone (23%). The median age at initiation of chelation therapy was 2 years (1.0–3.0), with a median duration of 3.5 years (2.5–5.0).
Thirty-three per cent of patients (71) initiated prophylaxis for osteopenia with vitamin D, and 83% of these patients (59) continued to take it at the time of analysis. Hydroxyurea was associated with standard treatment in 18 patients (8.5%), all of them NTDT. The median age at initiation was 11.5 years (5.0–25.8), with a median duration of 1 year (0.0–1.5). Three patients (16.5%) are still receiving hydroxyurea.
Thirty-two percent (69 patients) required implantation of a CVC, and 15.5% (33 patients) underwent splenectomy at a median age of 10 years (6.0–22.0). Thirteen patients (6%) underwent cholecystectomy.
The annual incidence of thalassaemia complications since our last publication in 2017 is summarised in Fig. 5, according to the total number of patients registered each year.
Fifty patients (23%) underwent HSCT, at a median age of 6 years (3.0–9.0). Fifty percent had complete chimerism at the time, 16% had mixed chimerism and 8 patients experienced graft rejection. Chronic GvHD occurred in 12% (6 patients).
The overall survival (death-free) was 99% (95% CI 97–100%) at 10 years, 98% (95% CI 95–100%) at 30 years and 83% (95% CI 66–100%) at 60 years. Survival curves for both SCD and thalassaemia are shown in Fig. 3.
Forty-three patients (20%) were lost to follow-up owing to emigration to another country (30%), follow-up changed to another centre (53.5%), and unknown causes (16%). Eight patients (4%) died, with the following causes: 4 related to cardiac hemosiderosis (at 54 years, undated, 11 years and 22 years respectively); 1 due to sepsis, at 4 years old; 1 due to severe liver failure, at 41 years old; 1 due to multifactoral respiratory and cardiac insufficiency, at 41 years; and 1 due to GvHD, at 3 years old.
Regarding COVID-19 data, 118 patients (55%) have presented with the infection since 2020. 19 patients (16%) required admission and only 6.5% received empirical intravenous antibiotic therapy. There were no associated deaths.
Other rare anaemias
A total of 224 patients (13% of the total sample) were registered with other diagnoses of interest, which are broken down below.
Other haemoglobinopathies
Haemoglobinopathies other than those previously described were recorded in 43.5% (97 patients), as follows: 20 patients (20.5%) with HbCC, 1 patient with HbDD, 1 patient with HbOC, 1 patient with HbOO and 74 patients (75.5%) with other haemoglobinopathies.
Most of the patients were diagnosed based on abnormalities in the haemoglobinopathy study as part of neonatal bloodspot screening or the finding of anaemia in the blood analysis. Most (86.5%) were born in Spain, as were their parents. The centres with the largest number of patients were the Gregorio Marañón and Vall d'Hebrón hospitals, with 52 and 29 cases, respectively.
Enzymopathies
A total of 103 patients (46%) had an enzymopathy: pyruvate kinase (PK) deficiency in 20 patients (19.5%) and glucose-6-phosphate dehydrogenase (G6PHD) deficiency in 83 patients (80.5%). The centres with largest percentages of patients were Vall d'Hebron (29.5%) and Sant Joan de Déu (23.5%).
In both diseases, most cases (65% in PK deficiency and 54% in G6PHD) were diagnosed mainly based on clinical compatibility or anaemia in laboratory tests, followed by family study findings.
Despite the high heterogeneity observed, the country of birth of most patients and their parents was Spain in both cases.
As for the treatment of patients with PK deficiency, up to 45% (9 patients) had received chelation therapy, with deferasirox being, once again, the most commonly used drug. Of these, 44% continue to receive deferasirox. Eight patients (40%) underwent splenectomy. One patient underwent HSCT and did not present GvHD.
Other hereditary anaemias
Another type of congenital anaemia was diagnosed in 7% (16 patients): congenital dyserythropoietic anaemia in 8 patients (3 patients with subtype IB, 2 patients with subtype II), xerocytosis in 6 patients and congenital sideroblastic anaemia in 2 patients.
Up to 69% of the cases (11 patients) were diagnosed based on anaemia in the blood analysis. Most (85.7%) were born in Spain, as were their parents.
None of the patients received chelation therapy at the time of the study. One patient with dyserythropoietic anaemia had undergone splenectomy, and none had received HSCT.
Discussion
The increase in cases in REHem-AR has been progressive in recent years, as can be seen in Fig. 6, with a peak between 2020 and 2021 of more than 300 cases, probably due to a general call for the update of patients made during that year to the hospitals included in the registry, or to an increase in the migratory flow to Spain. An increase in the birth rate seems less plausible, since this decreased in Spain from 7.19% in 2020 to 7.12% in 2021, according to data collected by the National Institute of Statistics (INE). The finding is consistent with a study conducted in the USA, where the demand for contraceptive therapies increased and conception decreased considerably in relation to the COVID-19 [9] pandemic.
In recent decades, migration from areas with a higher prevalence of haemoglobinopathies to Europe has increased. In the specific case of Spain, data from the INE show that in the last 20 years, the number of foreigners from Africa, Central and South America (where many of our SCD patients or their parents come from) and Asia has almost doubled, from approximately 1,700,000 in 2003 to 3,300,000 in 2022; in the specific case of migrants from Africa, the increase has been greater, 2.3 times higher than in 2002 [10, 11]. Consistent with this, most patients' parents are from Nigeria and Equatorial Guinea (in the case of SCD) and Morocco and Pakistan (in the case of thalassaemia), thus supporting the figures reported above for Spain.
In Spain, the number of new diagnoses has increased owing to the progressive implementation of screening in all autonomous communities [12]. In 2021 alone, 68 new cases in the registry corresponded to children diagnosed that year through neonatal bloodspot screening, making it the most frequent means of diagnosis of SCD and other haemoglobinopathies in Spain.
Focusing on patients with SCD, the most frequent complications were vaso-occlusive crisis (10% of patients in 2019, 7% in 2020) followed by acute chest syndrome (5.5% in 2019, 2% in 2020). Consistent with the literature, this finding reflects the complex pathophysiology of the disease, which is largely dependent on microcirculatory occlusion due to the hyperinflammatory state typical of affected patients [13,14,15].
In the case of thalassaemia, the most frequent diagnostic indicator is clinical anaemia, although the most recent cases of TDT were diagnosed as a result of neonatal bloodspot screening for SCD. Of note is the low incidence of stroke (0.5% in 2021, no cases reported all other years), similar to that found in other series comprising several thousand patients (around 0.25%), and the low rate of alloimmunisation, which is probably related to the usual practice of extensive erythrocyte phenotyping and transfusion based on the ABO, Rh and Kell groups, at least in the large centres that provide the most patients to REHem-AR. Endocrinopathies continue to be the main complication (Gupta and Aggarwal report up to 65% prevalence for this type of complication [16]), followed by haemosiderosis and the pathophysiology of the disease itself, despite adequate chelating treatment [17]. Consistent with findings reported elsewhere, we found hypogonadism to be the most prevalent endocrinopathy in recent years [16, 18].
Only a small percentage of thalassaemia patients have ever received hydroxyurea, all of them NTDT, for which some studies have shown a reduction in the frequency of anaemia in specific patients.
Only 60% of patients with SCD and an SS or Sβ0 genotype initiated hydroxyurea, a lower number than would be expected based on the recommendations in the guidelines of the Spanish Society of Paediatric Haematology and Oncology (SEHOP, 2019) [8], which favour starting the drug in all children at 9 months of age even if they are asymptomatic, and the recommendations of the Spanish Society of Haematology and Haemotherapy (SEHH, 2021) [19], which favour continuing it into adulthood in patients who were taking it or starting it in those who present symptoms or signs of organ damage.
Of note is the increase in HSCT procedures in SCD compared with the previous publication (3.5% previous vs. 6.5% current). The classic indications are restrictive and limited to specific and severe cases, such as a previous episode of stroke or severe and recurrent acute chest syndrome [8]. However, in recent years, these indications have been revised, given that the potential future severity of the disease is considered a sufficient criterion for transplantation in affected patients. In addition, overall and event-free survival outcomes are significantly higher in patients aged younger than 12–15 years, since transplant-related mortality increases in parallel with age [20,21,22].
The overall survival of patients with SCD and thalassemia in our study is consistent with data from other European countries (being much lower in countries such as Nigeria, Guinea or Pakistan, where most patients die before 5 years of age) [15, 20], largely influenced by the implementation of penicillin prophylaxis from 2 months of age in the case of SCD, adequate transfusion support and chelation therapy in the case of thalassaemia, and the prevention of associated complications in both cases [23,24,25,26].
On January 29, 2020, the WHO reported the first cases of SARS-COV-2 in the Eastern Mediterranean area. The social isolation measures that ensued to prevent transmission of the disease adversely affected the storage and transport chain of blood transfusion networks, which are indispensable for many haemoglobinopathy patients [27].
Along with the decrease in blood supply, an increase in the demand for blood of up to 10–25% was recorded in some centres. To date, our registry has only recorded the percentage of patients with a diagnosis of SCD who have received and are currently receiving a hypertransfusion regimen. We have never recorded the periodicity of transfusions; therefore, it has not been possible to see a change in this area during these years. However, with respect to the latest update of our registry, the number of cases that received a long-term hypertransfusion regimen has not been significantly affected (10% current vs. 8% previous).
Furthermore, it can be assumed that patients with SCD and/or thalassaemia are at greater risk of developing complications secondary to SARS-COV-2 infection [28, 29]. Therefore, most of the patients with SCD in our registry received empirical antibiotic therapy, in line with experience gathered in Great Britain and France [30]. None of the patients in our registry died.
The main limitation of this study is that REHem-AR is not population-based, and the inclusion of patients depends on the health care personnel who volunteer to follow the patients up. Furthermore, REHem-AR arose within the SEHOP and was later extended to include adult patients. This explains the greater participation of specialists caring for minors and the greater weight that minors have in the cohort registered, even though the proportion of adult patients is expected to be greater, since these diseases manifest throughout life (except in the case of primary parahyperthyroidism). Another important limitation continues to be the high rate of loss to follow-up in the registry, due mainly to the transfer of patients back to their country of origin or to a change in follow-up to a hospital not belonging to the REHem-AR network. Follow-up is also hampered by low socioeconomic level and the lack of recognition of the potential severity of the disease in some of our patients.
Moreover, the fact that data are entered into the registry by a multitude of different investigators limits the homogeneity of the response criteria. Some variables had not been well defined at the time of data collection and were defined a posteriori (e.g., vaso-occlusive crisis), and other variables have been added to complement them.
REHem-AR was recently linked to the European registry Rare Anaemia Disorders European Epidemiological Platform (RADeep), which is included in the ENROL study and in the framework of the European network ERN-EuroBloodNet. RADeep started its activity in 2017 with the aim of analyzing the demographics, survival, diagnostic methods, clinical manifestations and treatments of rare anaemias [31] in the European Union. Twelve member states, including Belgium, Germany and Spain, are currently part of the network.
Conclusion
Since the previous publication in 2019, and following the inclusion of new centres in the registry (currently 80), the number of cases in REHem-AR has increased by more than 500, in parallel with the increase in migration from Africa, Asia and Central and South America.
Vaso-occlusive crisis and acute chest syndrome continue to be the most important complications in SCD, followed by endocrinopathy in patients with thalassaemia. These data are consistent with those described in the literature. The life expectancy of patients with SCD and thalassaemia in our registry is consistent with that of other European countries.
The increase in the performance of HSCT in SCD represents a paradigm shift in the classic indications for these patients, although with the advent of gene therapy, it remains to be seen whether this trend will change in the coming years.
The data reflected in this work go some way to increasing our understanding of haemoglobinopathies and rare anaemias. The availability of new data can help to promote the development of new proposals to improve the diagnosis and treatment of these diseases.
References
Greene DN, Vaughn CP, Crews BO, Agarwal AM (2015) Advances in detection of hemoglobinopathies. Clin Chim Acta. 439:50-7. doi: https://doi.org/10.1016/j.cca.2014.10.006. Epub 2014 Oct 12. PMID: 25314938
Hoppe CC (2013) Prenatal and newborn screening for hemoglobinopathies. Int J Lab Hematol. 35(3):297-305
Piel FB, Steinberg MH, Rees DC (2017) Sickle Cell Disease. N Engl J Med. 376(16):1561-1573https://doi.org/10.1056/NEJMra1510865PMID: 28423290
Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN (2013) Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 10(7):e1001484. doi: https://doi.org/10.1371/journal.pmed.1001484. Epub 2013 Jul 16. PMID: 23874164; PMCID: PMC3712914
Brandow AM, Liem RI (2022) Advances in the diagnosis and treatment of sickle cell disease. J Hematol Oncol. 15(1):20https://doi.org/10.1186/s13045-022-01237-z PMID: 35241123; PMCID: PMC8895633
Bardón Cancho EJ, García-Morín M, Beléndez C, Velasco P, Benéitez D, Ruiz-Llobet A, Berrueco R, Argilés B, Cervera Á, Salinas JA, Vecilla C, Gondra A, Vallés G, Murciano T, Bermúdez M, Cela E (2020) en representación del grupo de trabajo de Eritropatología de la Sociedad Española de Hematología y Oncología Pediátricas (SEHOP). Update of the Spanish registry of haemoglobinopathies in children and adults. Med Clin (Barc). 155(3):95–103. English, Spanish. doi: https://doi.org/10.1016/j.medcli.2019.10.011. Epub 2020 Feb 26. PMID: 32113697
Weil LG, Charlton MR, Coppinger C, Daniel Y, Streetly A (2020) Sickle cell disease and thalassaemia antenatal screening programme in England over 10 years: a review from 2007/2008 to 2016/2017. J Clin Pathol. 73(4):183-190https://doi.org/10.1136/jclinpath-2019-206317Epub 2019 Nov 26. PMID: 31771971
Guía de Práctica Clínica. Enfermedad de células falciformes. Sociedad Española de Hematología y Oncología Pediátricas (2019)
Ullah MA, Moin AT, Araf Y, Bhuiyan AR, Griffiths MD, Gozal D. Potential Effects of the COVID-19 Pandemic on Future Birth Rate. Front Public Health. 2020 Dec 10;8:578438 https://doi.org/10.3389/fpubh.2020.578438 PMID: 33363080; PMCID: PMC7758229
Shook LM, Ware RE. Sickle cell screening in Europe: the time has come. Br J Haematol. 2018 Nov;183(4):534-535https://doi.org/10.1111/bjh.15596Epub 2018 Nov 14. PMID: 30430539
Howard J, Davies SC. Sickle cell disease in North Europe. Scand J Clin Lab Invest. 2007;67(1):27-38https://doi.org/10.1080/00365510601046441PMID: 17365983
Lobitz S, Telfer P, Cela E, Allaf B, Angastiniotis M, Backman Johansson C, Badens C, Bento C, Bouva MJ, Canatan D, Charlton M, Coppinger C, Daniel Y, de Montalembert M, Ducoroy P, Dulin E, Fingerhut R, Frömmel C, García-Morin M, Gulbis B, Holtkamp U, Inusa B, James J, Kleanthous M, Klein J, Kunz JB, Langabeer L, Lapouméroulie C, Marcao A, Marín Soria JL, McMahon C, Ohene-Frempong K, Périni JM, Piel FB, Russo G, Sainati L, Schmugge M, Streetly A, Tshilolo L, Turner C, Venturelli D, Vilarinho L, Yahyaoui R, Elion J, Colombatti R; with the endorsement of EuroBloodNet, the European Reference Network in Rare Haematological Diseases (2018) Newborn screening for sickle cell disease in Europe: recommendations from a Pan-European Consensus Conference. Br J Haematol. 183(4):648–660. doi: https://doi.org/10.1111/bjh.15600. Epub 2018 Oct 18. PMID: 30334577
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010 Dec 11;376(9757):2018-31https://doi.org/10.1016/S0140-6736(10)61029-XEpub 2010 Dec 3. PMID: 21131035
Ofori-Acquah SF (2020) Sickle cell disease as a vascular disorder. Expert Rev Hematol. (6):645-653https://doi.org/10.1080/17474086.2020.1758555Epub 2020 May 3. PMID: 32362160
Ware RE, de Montalembert M, Tshilolo L, Abboud MR (2017) Sickle cell disease. Lancet. 390(10091):311-323https://doi.org/10.1016/S0140-6736(17)30193-9Epub 2017 Feb 1. PMID: 28159390
Gupta V, Aggarwal P (2022) Complications in Transfusion-Dependent Thalassemia. Indian Pediatr. 59(12):911-912. PMID: 36511205
Vichinsky E (2016) Non-transfusion-dependent thalassemia and thalassemia intermedia: epidemiology, complications, and management. Curr Med Res Opin. 32(1):191-204https://doi.org/10.1185/03007995.2015.1110128Epub 2015 Nov 25. PMID: 26479125
Tiosano D, Hochberg Z (2001) Endocrine complications of thalassemia. J Endocrinol Invest. 24(9):716-23https://doi.org/10.1007/BF03343916PMID: 11716158
Guía de Enfermedad de Células Falciformes. Grupo de Eritropatología de la Sociedad Española de Hematología y Hemoterapia (2021)
Cimpeanu E, Poplawska M, Jimenez BC, Dutta D, Lim SH (2021) Allogeneic hematopoietic stem cell transplant for sickle cell disease: The why, who, and what. Blood Rev. 50:100868 https://doi.org/10.1016/j.blre.2021.100868Epub 2021 Jul 18. PMID: 34332804
Kanter J, Liem RI, Bernaudin F, Bolaños-Meade J, Fitzhugh CD, Hankins JS, Murad MH, Panepinto JA, Rondelli D, Shenoy S, Wagner J, Walters MC, Woolford T, Meerpohl JJ, Tisdale J (2021) American Society of Hematology 2021 guidelines for sickle cell disease: stem cell transplantation. Blood Adv. 5(18):3668-3689https://doi.org/10.1182/bloodadvances.2021004394C. PMID: 34581773; PMCID: PMC8945587
Angelucci E, Matthes-Martin S, Baronciani D, Bernaudin F, Bonanomi S, Cappellini MD, Dalle JH, Di Bartolomeo P, de Heredia CD, Dickerhoff R, Giardini C, Gluckman E, Hussein AA, Kamani N, Minkov M, Locatelli F, Rocha V, Sedlacek P, Smiers F, Thuret I, Yaniv I, Cavazzana M, Peters C; EBMT Inborn Error and EBMT Paediatric Working Parties (2014) Hematopoietic stem cell transplantation in thalassemia major and sickle cell disease: indications and management recommendations from an international expert panel. Haematologica. 99(5):811–20. doi: https://doi.org/10.3324/haematol.2013.099747. PMID: 24790059; PMCID: PMC4008115
Wastnedge E, Waters D, Patel S, Morrison K, Goh MY, Adeloye D, Rudan I (2018) The global burden of sickle cell disease in children under five years of age: a systematic review and meta-analysis. J Glob Health. 8(2):021103 https://doi.org/10.7189/jogh.08.021103. PMID: 30574296; PMCID: PMC6286674
Telfer P (2009) Update on survival in thalassemia major. Hemoglobin. 33 Suppl 1:S76-80https://doi.org/10.3109/03630260903347336PMID: 20001636
Brandow AM, Liem RI (2022) Advances in the diagnosis and treatment of sickle cell disease. J Hematol Oncol. 15(1):20https://doi.org/10.1186/s13045-022-01237-z PMID: 35241123; PMCID: PMC8895633
Kato GJ, Piel FB, Reid CD, Gaston MH, Ohene-Frempong K, Krishnamurti L, Smith WR, Panepinto JA, Weatherall DJ, Costa FF, Vichinsky EP (2018 ) Sickle cell disease. Nat Rev Dis Primers. 4:18010https://doi.org/10.1038/nrdp.2018.10PMID: 29542687
Piel FB, Patil AP, Howes RE, Nyangiri OA, Gething PW, Dewi M, Temperley WH, Williams TN, Weatherall DJ, Hay SI (2013) Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet. 381(9861):142–51. doi: https://doi.org/10.1016/S0140-6736(12)61229-X. Epub 2012 Oct 25. PMID: 23103089; PMCID: PMC3547249
Al-Riyami AZ, Abdella YE, Badawi MA, Panchatcharam SM, Ghaleb Y, Maghsudlu M, Satti M, Lahjouji K, Merenkov Z, Adwan A, Feghali R, Gebril N, Hejress S, Hmida S, AlHumaidan H, Jamal D, Najjar O, Raouf M (2021) The impact of COVID-19 pandemic on blood supplies and transfusion services in Eastern Mediterranean Region. Transfus Clin Biol. 28(1):16–24. doi: https://doi.org/10.1016/j.tracli.2020.11.002. Epub 2020 Dec 1. PMID: 33276150; PMCID: PMC7706593
McCloskey KA, Meenan J, Hall R, Tsitsikas DA (2020) COVID-19 infection and sickle cell disease: a UK centre experience. Br J Haematol. 190(2):e57-e58https://doi.org/10.1111/bjh.16779Epub 2020 Jun 17. PMID: 32369606
Arlet JB, de Luna G, Khimoud D, Odièvre MH, de Montalembert M, Joseph L, Chantalat-Auger C, Flamarion E, Bartolucci P, Lionnet F, Monnier S, Guillaumat C, Santin A (2020) Prognosis of patients with sickle cell disease and COVID-19: a French experience. Lancet Haematol. 7(9):e632-e634. doi: https://doi.org/10.1016/S2352-3026(20)30204-0. Epub 2020 Jun 18. Erratum in: Lancet Haematol. 2020 Sep;7(9):e635. PMID: 32563282; PMCID: PMC7302791
Mañú Pereira MDM, Colombatti R, Alvarez F, Bartolucci P, Bento C, Brunetta AL, Cela E, Christou S, Collado A, de Montalembert M, Dedeken L, Fenaux P, Galacteros F, Glenthøj A, Gutiérrez Valle V, Kattamis A, Kunz J, Lobitz S, McMahon C, Pellegrini M, Reidel S, Russo G, Santos Freire M, van Beers E, Kountouris P, Gulbis B (2023) Sickle cell disease landscape and challenges in the EU: the ERN-EuroBloodNet perspective. Lancet Haematol. 10(8):e687-e694https://doi.org/10.1016/S2352-3026(23)00182-5Epub 2023 Jul 11. PMID: 37451300
Kohne E (2011) Hemoglobinopathies: clinical manifestations, diagnosis, and treatment. Dtsch Arztebl Int. 108(31–32):532–40. doi: https://doi.org/10.3238/arztebl.2011.0532. Epub 2011 Aug 8. PMID: 21886666; PMCID: PMC3163784
Piel FB, Tatem AJ, Huang Z, Gupta S, Williams TN, Weatherall DJ (2014) Global migration and the changing distribution of sickle haemoglobin: a quantitative study of temporal trends between 1960 and 2000. Lancet Glob Health. 2(2):e80-9https://doi.org/10.1016/S2214-109X(13)70150-5. PMID: 24748392; PMCID: PMC3986033
Viprakasit V, Ekwattanakit S (2018) Clinical Classification, Screening and Diagnosis for Thalassemia. Hematol Oncol Clin North Am. 32(2):193-211https://doi.org/10.1016/j.hoc.2017.11.006PMID: 29458726
Acknowledgements
The authors would like to thank the patients, their families, the investigators and the research collaborators at each participating centre and the heads of the neonatal screening laboratories for their important work.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. JM.M.S employment contract has been partially funded by a research grant from Novartis.
Author information
Authors and Affiliations
Contributions
Marco Sánchez, Jose Manuel wrote and reviewed the manuscript text, prepared figures and did the research of the variables. Bardon Cancho, Eduardo Jesus; Beneitez, David; Payan-Pernia, Salvador; Collado Gimbert, Anna; Ruiz-Llobet, Anna; Salinas, Jose Antonio; Sebastian, Elena; Argiles, Bienvenida; Bermudez, Mar; Vazquez, Maria Angeles; Ortega Maria Jose; Lopez Rubio, Montserrat; Gondra Ainhoa; Uriz, Jose Javier; Morado Marta; Coll, Maria Teresa; Lopez Duarte, Monica; Baro Maria; Cervera, Aurea; Recasens, Valle; Garcia Blanes, Carmen; Carcavilla, Maria del Pozo; Tallon, Maria; Gonzalez Espin, Ana; Olteanu, Francisco; Gonzalez, Pablo; Mañu, Mar; and Cela, Elena, contributed to data collection and reviewed the manuscript text.
Corresponding author
Ethics declarations
S.P.P. has received speaker or consulting fees from Novartis, Agios, Alexion Pharmaceuticals, Amgen, Pfizer and Vertex Pharmaceuticals.
Conflict of interest
The authors declare that they have no conflicts of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
On behalf of the registry's Scientific Committee, made up of members of the Erythropathology working groups of the Spanish Society of Paediatric Haematology and Oncology (SEHOP) and the Spanish Society of Haematology and Haemotherapy (SEHH), and the rest of the registry's researchers.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marco Sánchez, J.M., Bardón Cancho, E.J., Benéitez, D. et al. Haemoglobinopathies and other rare anemias in Spain: ten years of a nationwide registry (REHem-AR). Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05788-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05788-8