Abstract
Very few data are available about hypomethylating agent (HMA) efficiency in core binding factor acute myeloid leukemias (CBF-AML). Our main objective was to evaluate the efficacy and safety of HMA in the specific subset of CBF-AML. Here, we report the results of a multicenter retrospective French study about efficacy of HMA monotherapy, used frontline or for R/R CBF-AML. Forty-nine patients were included, and received a median of 5 courses of azacitidine (n = 46) or decitabine (n = 3). ORR was 49% for the whole cohort with a median time to response of 112 days. After a median follow-up of 72.3 months, median OS for the total cohort was 10.6 months. In multivariate analysis, hematological relapse of CBF-AML at HMA initiation was significantly associated with a poorer OS (HR: 2.13; 95%CI: 1.04–4.36; p = 0.038). Responders had a significantly improved OS (1-year OS: 75%) compared to non-responders (1-year OS: 15.3%; p < 0.0001). Hematological improvement occurred for respectively 28%, 33% and 48% for patients who were red blood cell or platelet transfusion-dependent, or who experienced grade 3/4 neutropenia at HMA initiation. Adverse events were consistent with the known safety profile of HMA. Our study highlights that HMA is a well-tolerated therapeutic option with moderate clinical activity for R/R CBF-AML and for patients who cannot handle intensive chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a type of cancer derived from an oligoclonal proliferation of undifferentiated hematopoietic myeloid precursors[1]. Core-Binding Factor AML (CBF-AML) account for about 10–15% of adult AML[2, 3], and are graded in the favorable risk group of European LeukemiaNet (ELN) classification[4]. CBF-AML are characterized by either the chromosomal translocation t(8;21)(q22;q22.1) or rearrangement inv(16)(p13.1q22)/t(16;16)(p13.1;q22), respectively leading to the translation of aberrant fusion proteins RUNX1::RUNX1T1 and CBFB::MYH11[5,6,7]. Where, under normal conditions, RUNX1 and CBFB form a heterodimeric protein complex of transcription factors involved in normal myeloid differentiation, in CBF-AML, those fusion transcripts induce, through aberrant epigenetic mechanisms, the silencing of genes involved in normal hematopoiesis[8, 9], and drive the differentiation blockade in CBF-AML[10, 11].
When a cytarabine-based chemotherapy is used as first-line treatment, reported first complete remission rate is about 90%, even in elderly[12,13,14]. Nonetheless, 5-year relapse rate is 30–40% and 5-year overall survival (OS) is 60–75%, suggesting the heterogeneity of the disease[2]. Several prognostic factors are associated with CBF-AML outcomes, such as age, white blood cell (WBC) count at diagnosis, cooperative tyrosine-kinase mutations (KIT, FLT3, N/KRAS) or clonal architecture[15,16,17,18,19,20,21,22]. Measurable residual disease (MRD) is also a strong prognosis factor to identify patients with a high risk of relapse[23]. An early MRD reduction ≥ 3 log has been shown to significantly lower the incidence of relapse in multivariate analysis[24], whereas MRD persistence in blood at the end of treatment is associated with higher levels of relapse in CBF-AML with t(8;21)[25].
In retrospective studies about outcomes of relapsed / refractory (R/R) CBF-AML, reported second complete remission rate remains high (> 75%) in patients treated with high-dose chemotherapy, gemtuzumab ozogamicin (GO) and/or allogeneic stem cell transplant (ASCT), but OS seems shorter than for patients in CR1, especially in the elderly, or when the CR1 duration was short[26, 27]. Moreover, even if CBF-AML are classified as favorable prognosis AML, relapses after intensive chemotherapy remain a major cause of death[26], and a significant proportion of patients (elderly, patients with poor performance status) may not handle intensive chemotherapy toxicities. In these situations, use of hypomethylating agents (HMA), such as azacitidine or decitabine, might be a therapeutic option. HMA has now become the standard treatment for frail patients with high-risk myelodysplastic syndromes and AML, alone or in combination with other therapies such as venetoclax[28,29,30,31,32]. Nevertheless, given that these studies excluded or did not specifically analyze patients with CBF-AML, and that the proportion of CBF-AML decreases with age[33, 34], very few data were published about HMA efficacy in the specific CBF-AML subset.
Here, we report the results of a multicenter retrospective French study about effectiveness and safety of HMA as monotherapy, used in frontline or for R/R CBF-AML.
Methods
Patients and data collection
We retrospectively screened patients aged ≥ 18 years receiving HMA as monotherapy for frontline treatment or for R/R CBF-AML (cytologic relapse or molecular relapse/progression), diagnosed according to the 2016 World Health Organization classification[35], in 17 French centers between January 2008 and December 2019. CBF-AML associated translocations and/or corresponding fusion transcripts had to be confirmed by conventional karyotype, fluorescence in situ hybridization or by RT-qPCR. Patients with CBF-AML in complete response who received HMA for preventive treatment after ASCT for were excluded. No other exclusion criterion was applied.
Clinical, biological and treatment-related data were retrospectively gathered from available medical reports. When available, molecular MRD levels performed in peripheral blood and/or bone marrow by RT-qPCR were collected. Declared hematological and non-hematological adverse events were classified according to Common Terminology Criteria for Adverse Events (CTCAE) version 5.0[36].
According to French laws and national guidelines, retrospective studies using data from medical charts only require a declaration to the “Commission Nationale Informatique & Libertés” (CNIL, declaration number 2761316)[37]. There was therefore no requirement for a declaration to an ethics committee.
End points and statistical analysis
Primary end point was overall survival (OS). Secondary end points included (i) event-free survival (EFS), (ii) overall response rate (ORR), (iii) transfusion independence rate and hematological improvement for neutrophils, and (iv) description of reported adverse events during HMA courses.
Data are described as median and ranges for quantitative variables, and frequency and percentages for qualitative variables. Characteristics of subgroups were compared with nonparametric tests (Fisher exact test for qualitative variables, Wilcoxon test for quantitative variables). Survival analysis were assessed using Kaplan–Meier method. OS was defined as time from the first HMA injection to death resulting of any cause. Alive patients were censored at the end of follow-up. The effect of pre-therapeutic parameters on OS was tested with univariate and multivariate Cox model. EFS was defined as time between HMA initiation and any event (treatment failure, progressive disease, hematologic relapse or death). Statistical significance in OS differences between groups was determined by the log-rank test.
When possible, CBF-AML status and response were assessed retrospectively according to 2017 and 2018 ELN recommendations for all HMA courses[38, 39]. ORR was defined by complete remission with undetectable MRD (CRMRD-), complete remission (CR), complete remission with incomplete hematologic recovery (CRi) or partial remission (PR). Treatment failure was defined as a death of indeterminate cause occurring within the 7 days after HMA initiation. Transfusion independence, for red blood cells (RBC) or for platelets, was defined as no transfusion for more than two consecutive HMA courses for transfusion-dependent patients at HMA initiation[40, 41]. Hematological improvement for neutrophils was defined by an at-least 100% increase and an absolute increase > 0.5 G/L of the absolute neutrophil count, occurring at any point during HMA treatment for patients who had a grade 3 or 4 neutropenia at HMA beginning[41].
All statistical tests were two-tails and Alpha-risk was fixed at 5%. Analyses were performed using R.4.1.1. for Mac (R Core Team 2021, R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients and CBF-AML characteristics at HMA initiation
We identified 81 patients who received at least one dose of azacitidine or decitabine for CBF-AML treatment. Thirteen patients were not included due to missing data. Respectively 8 and 11 patients were excluded for receiving HMA for post-ASCT prophylactic therapy, and for receiving concomitant anti-leukemic therapies (tyrosine-kinase inhibitors, venetoclax, gemtuzumab-ozogamicin or donor lymphocyte infusions). Therefore, 49 patients were included for final analysis. At HMA onset, median age was 63 years (range 23–86) for the whole cohort, with a sex ratio (female/male) of 1.04. Twelve patients (24%) had secondary AML, mostly due to prior chemotherapy and/or radiotherapy for solid tumor or lymphoid malignancy. Eight patients (16%) experienced an extra-medullar and/or a central nervous system involvement of CBF-AML. Patients and CBF-AML characteristics at HMA initiation are summarized in Table 1.
HMA treatment indication and modalities
Median time between diagnosis and HMA therapy initiation was 215 days, with a very wide range, from 1 day to more than 14 years for a patient who experienced a late CBF-AML relapse. HMA were used as frontline treatment for 20 patients (41%) with a median delay before treatment introduction of 16 days (range 1–91). While most of these patients were treated with HMAs because of their age (median age 74.5 years in this group), four patients under 65 years of age received HMAs as first-line treatment because of severe comorbidities contraindicating intensive chemotherapy (severe obesity, ischemic heart disease, septic shock), or because of patient choice. On the other hand, 29 patients (59%) received HMAs as second-line or more (after failure of intensive chemotherapy, for R/R CBF-AML), with a median time from diagnosis to HMA treatment of 476 days (range 104–5393) (Table 1). This group included 24 patients with cytologic CBF-AML relapse and 5 patients with molecular relapse or progression.
A total of 344 cycles of HMA were analyzed. Forty-six patients received subcutaneous injections of azacitidine and 3 received decitabine intravenously. The median number of HMA cycles administered was 5 (range 1–36), with a median of respectively 6 (range 1–36) and 4 cycles (range 1–20) for patients who received HMA therapy as frontline treatment and for R/R CBF-AML. Most of patients received azacitidine at standard dose of 75 mg/m2/d for 7 days (consecutive or not), except for one patient who received reduced doses of 60 mg/m2/d from the 3rd cycle due to hematological toxicity. All administered courses of decitabine were at 20 mg/m2/d for 5 days. As expected, for patients who received at least two cycles, median delay between consecutive HMA cycles was 28 days.
In most cases, treatment was stopped for progressive disease (n = 34; 69%). Other reasons for HMA discontinuation were patient’s choice (n = 4; 8%), complete response with undetectable MRD (n = 3; 6%), switch for intensive therapy, including allogeneic stem cell transplant (n = 3; 6%), non-hematologic toxicity (n = 2; 4%), death (n = 2; 4%), and a prostate cancer progression (n = 1; 2%).
Effectiveness of HMA treatment
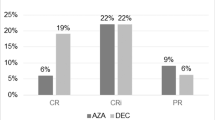
Eight patients were excluded from this analysis as their therapeutic response was not assessable according to the ELN 2017 criteria. Of the remaining 41 patients, 20 responded to HMA treatment, giving an overall response rate (ORR) of 49%. Best response was CRMRD- in 4 patients, CR in 10 patients, and CRi in 6 patients. Median time to response was 112 days (range 28–183), corresponding to 4 HMA cycles (range 1–6). According to HMA indication, the ORR was respectively 69% (11/16) and 36% (9/25) for patients who received HMA as frontline therapy or for R/R CBF-AML (Chi-squared test, p = 0.041). For the 21 non-responding patients, best response was stable disease (n = 7), progressive disease (n = 10), treatment failure (n = 2), hematologic relapse (n = 1) or molecular progression (n = 1). Table 2 compares clinical, biological and HMA treatment characteristics for responders and non-responders. Different characteristics between responders and non-responders were number of therapeutic lines prior HMA introduction and the total number of received HMA cycles.
At HMA initiation, 32 patients were RBC and/or platelet transfusion-dependent (65%). For RBC, 32 patients (65%) were transfusion-dependent prior to HMA introduction, of whom 9 became transfusion-independent (28%). The median number of HMA courses before RBC transfusion-independency was 3 (range 2–5). For platelets, 27 patients (55%) were transfusion-dependent prior to HMA introduction, of whom 9 became transfusion-independent (33%). The median number of HMA courses before platelet transfusion-independency was 3 (range 3–4). Twenty-one patients had a grade 3 or 4 neutropenia (43%) at HMA initiation, and hematological-improvement for neutrophils was noticed for 10 patients (48%).
Survival analysis
At the end of follow-up, 7 patients were still alive (14%). After a median follow-up of 72.3 months (95%CI: 31.3-NR), median overall survival (OS) was 10.6 months (95%CI: 8.3–16.3) for the total cohort, with a one-year OS at 46.0% (95%CI: 33.9–62.5) (Fig. 1a). Median EFS was 6.9 months (95%CI: 5.7–10.1), with a 1-year EFS of 26.2% (95%CI: 15.6–44.1) (Fig. 1b). Median overall survival when HMA were used at diagnosis was 13.0 months (95%CI: 8.4–24.1), and 9.6 months (95%CI: 5.7–16.3) when used as second-line therapy or more (log-rank test, p = 0.6) (Supplemental Fig. 1). Nevertheless, OS was significantly different according to CBF-AML status at HMA introduction with a 1-year OS of 55.0% (95%CI: 37.0–81.8) for diagnosis, 30.9% (95%CI: 16.7–57.0) for hematologic relapse and 80.0% (95%CI: 51.6–100) for molecular relapse or progression (log-rank test, p = 0.0095) (Fig. 1c). Moreover, response to HMA treatment significantly improved OS compared to non-responding patients, with a respectively one-year OS of 75.0% (95%CI: 58.2–96.6) and 15.3% (95%CI: 5.4–43.3) (log-rank test, p < 0.0001) (Fig. 1d).
Kaplan–Meier survival curves. a. OS survival curve for the total cohort. b. EFS survival curve for the total cohort. c. OS survival curve according to AML status at HMA onset: diagnosis (black line), hematologic relapse (grey line) or molecular relapse or progression (dashline). d. OS survival curve for HMA responders (black line) or non-responders (grey line)
Among baseline parameters, CBF-AML status at HMA initiation (diagnosis vs. hematological relapse vs. molecular relapse or progression), platelets count (per 10 G/L) and medullar blast percentage were associated with OS in univariate analysis (p < 0.1) (Supplemental Table 1). These parameters were therefore included in multivariate analysis, which demonstrated that hematological relapse status was significantly associated with shorter OS for patients treated with HMA (HR: 2.13; 95%CI: 1.04–4.36; p = 0.038) (Fig. 2).
Safety of HMA treatment
As expected, most frequently reported adverse events (AEs) were cytopenia. Forty-two patients (86%) experienced at least one episode of grade 3 or 4 cytopenia during HMA courses. Grade 3 or 4 neutropenia, anemia and thrombocytopenia occurred in respectively 67%, 69% and 65% of patients. Three and 5 patients became respectively RBC and platelets transfusion-dependent during HMA treatment. At least one episode of febrile neutropenia was reported in 24 patients (49%), of which three died of septic shock. Most of the clinically documented infections involved lung, ENT (Ear, Nose, Throat) or skin. Bleeding symptoms were noted in 12 patients (24%). Most of them were mild skin or mucosal hemorrhages, but one patient died from cerebral bleeding.
Declared non-hematological AEs were mostly mild. Most common were skin reaction at injection site (49%), nausea and/or vomiting (27%), diarrhea (8%) and constipation (8%). Other non-hematological AEs occurred in less than 5% of patients. It should be noted that two patients died after the onset of non-febrile dyspnea of unknow cause. Both of them were receiving their first course of HMA for newly diagnosed CBF-AML. Pulmonary leukostasis and tumor lysis syndrome were discarded in both cases.
Discussion
Even if CBF-AML are classified as favorable prognosis when treated with intensive chemotherapy, reported 5-year relapse rate remains high, with no consensus about the best second-line therapy. Hypomethylating agents are an interesting therapeutic option for patients experiencing R/R AML [42, 43], or for frail patients who cannot handle intensive chemotherapy [44]. Nevertheless, CBF-AML patients were excluded from the phase III clinical trials evaluating the efficacy of azacitidine or decitabine for high-risk MDS or AML [28,29,30,31,32]. CBF-AML were also excluded from the recent QUAZAR AML-001 study which demonstrated that maintenance with oral azacitidine CC-486 prolongs OS and RFS in patients with AML in first remission after intensive chemotherapy who were not candidates for allogeneic stem cell transplant [45]. In this retrospective study, we report an overall response rate of 49% for CBF-AML patients treated with azacitidine or decitabine with a median delay to response of 4 HMA cycles. Median overall survival when HMA were used upfront was 13.0 months (95%CI: 8.4–24.1), and 9.6 months (95%CI: 5.7–16.3) when used as second-line therapy or more for R/R CBF-AML. Response was significantly associated with improved OS with a 1-year OS of 75.0% for responders vs. 15.3% for non-responders (p < 0.0001). As expected, HMA toxicity was consistent with the well-known safety profile of HMA published in prospective studies in other AML subtypes [31, 46]. To our knowledge, this is the largest real-life cohort published about effectiveness of HMA in CBF-AML subgroup.
The epigenetic abnormalities and the effectiveness of HMA in the subset of CBF-AML has been widely suggested by pre-clinical studies, especially in AML with t(8;21). Indeed, it has been demonstrated that the aberrant fusion protein RUNX1::RUNX1T1 was able to recruit a transcriptional repressor complex including DNA methyltransferase 1 (DNMT1) and histone deacetylases (HDACs), leading to chromatin remodeling, silencing of several genes involved in normal hematopoiesis and differentiation blockage in CBF-AML with t(8;21) [8, 9, 47]. The in vitro exposition of leukemic cells expressing this fusion protein to DNMT inhibitors (such as decitabine or azacitidine) led to restoration of normal gene expression and cell differentiation, especially when combined with HDAC inhibitors. Moreover, mutations in epigenetic regulators, and especially genes involved in DNA methylation (such as TET2 or DNMT3A), are significantly enriched in RUNX1::RUNX1T1 CBF-AML, and play a key role in leukemogenesis process [48, 49]. A recent study even suggested that these mutations are associated with shorter OS [50]. On the other hand, very few epigenetic regulator genes were found mutated in CBF-AML with inv(16). Nevertheless, aberrant DNA methylation has also been described in this specific subtype of AML. A recent study demonstrated that the fusion protein CBFB::MYH11 impairs the normal interaction between DNMT3A and RUNX1, leading to the hypomethylation and the hyperexpression of genes involved in AML progression [51]. It has also been demonstrated that the promotor of another RUNX family gene, RUNX3, was frequently hypermethylated in CBF-AML with inv(16) [52]. Despite these data suggesting impaired epigenetic mechanisms in CBF-AML, very few were published about clinical HMA efficiency in this AML subgroup.
In a retrospective study about R/R CBF-AML, Khan et al.included 6 patients who received HMA as first salvage therapy [27]. They reported a CR rate of 16.7% (n = 1/6), which is consistent with the low ORR we reported (36%, n = 9/25). In their study, the median OS was shorter, but not statistically different from patients who received high dose chemotherapy as salvage treatment. This result might be due to the small number of patients treated with HMA. Moreover, three published studies examined the role of HMA maintenance after intensive chemotherapy. First, in a prospective study, Blum et al.reported results about 46 young adults with CBF-AML in CR1 who received decitabine maintenance after high-dose chemotherapy without ASCT [53]. One-year disease-free survival (DFS) was 80%, and did not statistically differ from reported DFS in non-CBF-AML patients. Senapati et al.reported in a prospective study that decitabine maintenance in CBF-AML patients in CR1 after intensive chemotherapy with persistent molecular disease led to complete molecular response in 52% of cases (n = 12/23) [54]. Nevertheless, even if the median molecular relapse free-survival in responders was 93.9 months, there was no difference in overall survival between responders and non-responders to HMA therapy. Finally, Ragon et al.reported retrospective results about 23 CBF-AML patients receiving azacitidine maintenance after chemotherapy [55]. The authors concluded that patients with low levels of MRD might benefit from HMA maintenance to prolong survival, especially for those who experienced MRD reduction after two cycles of HMA therapy. These studies and our suggest that HMA could be of therapeutic interest in the setting of CBF-AML.
Nevertheless, multiple bias and limits might be discussed about our study. First, the number of patients is low and the population heterogeneous, HMA treatment for CBF-AML remaining a rare situation in clinical practice. Among all the adult CBF-AML patients we screened, about 8% only received HMA treatment at any time during AML evolution, although we limited exclusion criteria to prevent selection bias. Secondly, retrospective studies imply a bias in data collection and analysis. To avoid declaration heterogeneity, we retrospectively re-assessed AML status at HMA initiation and response status after all HMA courses according to published recommendations [38], allowing a reproducible evaluation between all patients. Response was assessable after about one third of all HMA courses. Indeed, if clinical or blood evaluation may be sufficient to assess progressive disease, bone marrow aspiration is mandatory to reach a conclusion of complete or partial remission [38]. Therefore, because of the low proportion of patients who benefited from bone marrow evaluation, we might have underestimated the ORR. The toxicity assessment may also have been underestimated due to retrospective data collection, but it is unlikely that the safety profile of HMA is different in the CBF-AML subgroup compared to the others.
Finally, it has to be noted that HMA are not used as monotherapy anymore for AML treatment. The study VIALE-A demonstrated that association of azacitidine with BCL2 inhibitor venetoclax improves patients OS, leading to the recent approval of this combination for newly diagnosed AML in intensive chemotherapy ineligible patients [32]. Nevertheless, CBF-AML were also excluded from this study, and no clue is currently available for the efficacy of azacitidine + venetoclax combination in this AML subgroup, with the exception of one case report [56]. HMA may also be associated with other drugs whose anti-leukemic activity in CBF-AML have been suggested, such as gemtuzumab-ozogamicin [26, 57], or tyrosine-kinase inhibitors dasatinib [58, 59] or midostaurin [60].
Conclusion
In conclusion, our study highlights that hypomethylating agents are a well-tolerated therapeutic option for R/R CBF-AML and for patients who cannot handle intensive chemotherapy. Although the efficacy of HMA appears similar in CBF-AML to that reported in other subtypes of AML, our results seem suboptimal in the context of this AML subset associated with a "favorable" prognosis. HMA efficacy might be improved if combined with other therapies such as BCL-2 inhibitor venetoclax, or tyrosine-kinase inhibitors in CBF-AML.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AEs:
-
Adverse events
- AML:
-
Acute myeloid leukemia
- ASCT:
-
Allogeneic stem cell transplant
- CBF:
-
Core binding factor
- CR:
-
Complete remission
- CRi:
-
Complete remission with incomplete hematologic recovery
- CRMRD- :
-
Complete remission with undetectable measurable residual disease
- DFS:
-
Disease-free survival
- ELN:
-
European LeukemiaNet
- EFS:
-
Event-free survival
- DNMT:
-
DNA methyltransferases
- HDAC:
-
Histone deacetylases
- HMA:
-
Hypomethylating agent
- MRD:
-
Measurable residual disease
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- PR:
-
Partial remission
- RBC:
-
Red blood cells
- RFS:
-
Relapse-free survival
- RT-qPCR:
-
Real-time quantitative polymerase chain reaction
- R/R:
-
Relapsed / refractory
References
Dohner H, Weisdorf DJ, Bloomfield CD (2015) Acute Myeloid Leukemia. N Engl J Med 373:1136–1152
Grimwade D, Hills RK, Moorman AV et al (2010) Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 116:354–365
Papaemmanuil E, Gerstung M, Bullinger L et al (2016) Genomic Classification and Prognosis in Acute Myeloid Leukemia. N Engl J Med 374:2209–2221
Dohner H, Wei AH, Appelbaum FR et al (2022) Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 140:1345–1377
Miyoshi H, Kozu T, Shimizu K et al (1993) The t(8;21) translocation in acute myeloid leukemia results in production of an AML1-MTG8 fusion transcript. Embo J 12:2715–2721
Liu P, Tarle SA, Hajra A et al (1993) Fusion between transcription factor CBF beta/PEBP2 beta and a myosin heavy chain in acute myeloid leukemia. Science 261:1041–1044
Claxton DF, Liu P, Hsu HB et al (1994) Detection of fusion transcripts generated by the inversion 16 chromosome in acute myelogenous leukemia. Blood 83:1750–1756
Liu S, Shen T, Huynh L et al (2005) Interplay of RUNX1/MTG8 and DNA methyltransferase 1 in acute myeloid leukemia. Cancer Res 65:1277–1284
Gozzini A, Santini V (2005) Butyrates and decitabine cooperate to induce histone acetylation and granulocytic maturation of t(8;21) acute myeloid leukemia blasts. Ann Hematol 84(Suppl 1):54–60
Sakakura C, Yamaguchi-Iwai Y, Satake M et al (1994) Growth inhibition and induction of differentiation of t(8;21) acute myeloid leukemia cells by the DNA-binding domain of PEBP2 and the AML1/MTG8(ETO)-specific antisense oligonucleotide. Proc Natl Acad Sci U S A 91:11723–11727
Zhen T, Cao Y, Ren G et al (2020) RUNX1 and CBFbeta-SMMHC transactivate target genes together in abnormal myeloid progenitors for leukemia development. Blood 136:2373–2385
Bloomfield CD, Lawrence D, Byrd JC et al (1998) Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype. Cancer Res 58:4173–4179
Prebet T, Boissel N, Reutenauer S et al (2009) Acute myeloid leukemia with translocation (8;21) or inversion (16) in elderly patients treated with conventional chemotherapy: a collaborative study of the French CBF-AML intergroup. J Clin Oncol 27:4747–4753
Lowenberg B, Pabst T, Vellenga E et al (2011) Cytarabine dose for acute myeloid leukemia. N Engl J Med 364:1027–1036
Nguyen S, Leblanc T, Fenaux P et al (2002) A white blood cell index as the main prognostic factor in t(8;21) acute myeloid leukemia (AML): a survey of 161 cases from the French AML Intergroup. Blood 99:3517–3523
Schoch C, Kern W, Schnittger S et al (2004) The influence of age on prognosis of de novo acute myeloid leukemia differs according to cytogenetic subgroups. Haematologica 89:1082–1090
Hoyos M, Nomdedeu JF, Esteve J et al (2013) Core binding factor acute myeloid leukemia: the impact of age, leukocyte count, molecular findings, and minimal residual disease. Eur J Haematol 91:209–218
Prabahran A, Tacey M, Fleming S et al (2018) Prognostic markers in core-binding factor AML and improved survival with multiple consolidation cycles of intermediate-/high-dose cytarabine. Eur J Haematol.
Boissel N, Leroy H, Brethon B et al (2006) Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia 20:965–970
Paschka P, Marcucci G, Ruppert AS et al (2006) Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol 24:3904–3911
Duployez N, Marceau-Renaut A, Boissel N et al (2016) Comprehensive mutational profiling of core binding factor acute myeloid leukemia. Blood 127:2451–2459
Itzykson R, Duployez N, Fasan A et al (2018) Clonal interference of signaling mutations worsens prognosis in core-binding factor acute myeloid leukemia. Blood 132:187–196
Yin JA, O’Brien MA, Hills RK et al (2012) Minimal residual disease monitoring by quantitative RT-PCR in core binding factor AML allows risk stratification and predicts relapse: results of the United Kingdom MRC AML-15 trial. Blood 120:2826–2835
Jourdan E, Boissel N, Chevret S et al (2013) Prospective evaluation of gene mutations and minimal residual disease in patients with core binding factor acute myeloid leukemia. Blood 121:2213–2223
Willekens C, Blanchet O, Renneville A et al (2016) Prospective long-term minimal residual disease monitoring using RQ-PCR in RUNX1-RUNX1T1-positive acute myeloid leukemia: results of the French CBF-2006 trial. Haematologica 101:328–335
Hospital MA, Prebet T, Bertoli S et al (2014) Core-binding factor acute myeloid leukemia in first relapse: a retrospective study from the French AML Intergroup. Blood 124:1312–1319
Khan M, Cortes J, Qiao W et al (2018) Outcomes of Patients With Relapsed Core Binding Factor-Positive Acute Myeloid Leukemia. Clin Lymphoma Myeloma Leuk 18:e19–e25
Silverman LR, Demakos EP, Peterson BL et al (2002) Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol 20:2429–2440
Fenaux P, Gattermann N, Seymour JF et al (2010) Prolonged survival with improved tolerability in higher-risk myelodysplastic syndromes: azacitidine compared with low dose ara-C. Br J Haematol 149:244–249
Kantarjian HM, Thomas XG, Dmoszynska A et al (2012) Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol 30:2670–2677
Dombret H, Seymour JF, Butrym A et al (2015) International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood 126:291–299
DiNardo CD, Jonas BA, Pullarkat V et al (2020) Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N Engl J Med 383:617–629
Vey N, Coso D, Bardou VJ et al (2004) The benefit of induction chemotherapy in patients age > or = 75 years. Cancer 101:325–331
Grimwade D, Walker H, Harrison G et al (2001) The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood 98:1312–1320
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127:2391–2405
CTCAE. Common terminology criteria for adverse events (CTCAE) version 5.0. In. 2017, November 27. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf
CNIL. Recherches dans le domaine de la santé : Le nouveau chapitre IX est applicable. In. 2017, June 30. https://www.cnil.fr/fr/recherches-dans-le-domaine-de-la-sante-la-cnil-adopte-de-nouvelles-mesures-de-simplification
Dohner H, Estey E, Grimwade D et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
Schuurhuis GJ, Heuser M, Freeman S et al (2018) Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood 131:1275–1291
Cheson BD, Greenberg PL, Bennett JM et al (2006) Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 108:419–425
Platzbecker U, Fenaux P, Ades L et al (2019) Proposals for revised IWG 2018 hematological response criteria in patients with MDS included in clinical trials. Blood 133:1020–1030
Itzykson R, Thepot S, Berthon C et al (2015) Azacitidine for the treatment of relapsed and refractory AML in older patients. Leuk Res 39:124–130
Schroeder T, Rautenberg C, Haas R et al (2018) Hypomethylating agents for treatment and prevention of relapse after allogeneic blood stem cell transplantation. Int J Hematol 107:138–150
Dombret H, Itzykson R (2017) How and when to decide between epigenetic therapy and chemotherapy in patients with AML. Hematol Am Soc Hematol Educ Program 2017:45–53
Wei AH, Dohner H, Pocock C et al (2020) Oral Azacitidine Maintenance Therapy for Acute Myeloid Leukemia in First Remission. N Engl J Med 383:2526–2537
Fenaux P, Mufti GJ, Hellstrom-Lindberg E et al (2009) Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 10:223–232
Serrano E, Carnicer MJ, Lasa A et al (2008) Epigenetic-based treatments emphasize the biologic differences of core-binding factor acute myeloid leukemias. Leuk Res 32:944–953
Faber ZJ, Chen X, Gedman AL et al (2016) The genomic landscape of core-binding factor acute myeloid leukemias. Nat Genet 48:1551–1556
Christen F, Hoyer K, Yoshida K et al (2019) Genomic landscape and clonal evolution of acute myeloid leukemia with t(8;21): an international study on 331 patients. Blood 133:1140–1151
Jahn N, Terzer T, Strang E et al (2020) Genomic heterogeneity in core-binding factor acute myeloid leukemia and its clinical implication. Blood Adv 4:6342–6352
Liu P, Liu JP, Sun SJ et al (2021) CBFB-MYH11 Fusion Sequesters RUNX1 in Cytoplasm to Prevent DNMT3A Recruitment to Target Genes in AML. Front Cell Dev Biol 9:675424
Estecio MR, Maddipoti S, Bueso-Ramos C et al (2015) RUNX3 promoter hypermethylation is frequent in leukaemia cell lines and associated with acute myeloid leukaemia inv(16) subtype. Br J Haematol 169:344–351
Blum W, Sanford BL, Klisovic R et al (2017) Maintenance therapy with decitabine in younger adults with acute myeloid leukemia in first remission: a phase 2 Cancer and Leukemia Group B Study (CALGB 10503). Leukemia 31:34–39
Senapati J, Shoukier M, Garcia-Manero G et al (2022) Activity of decitabine as maintenance therapy in core binding factor acute myeloid leukemia. Am J Hematol 97:574–582
Ragon BK, Daver N, Garcia-Manero G et al (2017) Minimal residual disease eradication with epigenetic therapy in core binding factor acute myeloid leukemia. Am J Hematol 92:845–850
Levato L, Gianfelici V, Caglioti F et al (2020) Sustained Complete Remission with Incomplete Hematologic Recovery (CRi) in a Patient with Relapsed AML and Concurrent BCR-ABL1 and CBFB Rearrangement Treated with a Combination of Venetoclax and 5-Azacytidine. Chemotherapy 65:51–53
Borthakur G, Cortes JE, Estey EE et al (2014) Gemtuzumab ozogamicin with fludarabine, cytarabine, and granulocyte colony stimulating factor (FLAG-GO) as front-line regimen in patients with core binding factor acute myelogenous leukemia. Am J Hematol 89:964–968
Boissel N, Renneville A, Leguay T et al (2015) Dasatinib in high-risk core binding factor acute myeloid leukemia in first complete remission: a French Acute Myeloid Leukemia Intergroup trial. Haematologica 100:780–785
Paschka P, Schlenk RF, Weber D et al (2018) Adding dasatinib to intensive treatment in core-binding factor acute myeloid leukemia-results of the AMLSG 11–08 trial. Leukemia 32:1621–1630
Voso MT, Larson RA, Jones D et al (2020) Midostaurin in patients with acute myeloid leukemia and FLT3-TKD mutations: a subanalysis from the RATIFY trial. Blood Adv 4:4945–4954
Acknowledgements
Not applicable
Funding
No funding was used for this study.
Author information
Authors and Affiliations
Contributions
Designed research; LG, ER.
Performed research; LG.
Collected data; LG.
Analyzed and interpreted data; LG.
Performed statistical analysis; LG, JJT.
Wrote/reviewed the manuscript; All authors.
Approved manuscript; All authors.
Corresponding author
Ethics declarations
Ethics approval
According to French laws and national guidelines, retrospective studies using data from medical charts only require a declaration to the “Commission Nationale Informatique & Libertés” (CNIL, declaration number 2761316). There was therefore no requirement for a declaration to an ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Keypoint
Hypomethylating agents have moderate clinical activity in core binding factor-AML.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gabellier, L., Peterlin, P., Thepot, S. et al. Hypomethylating agent monotherapy in core binding factor acute myeloid leukemia: a French multicentric retrospective study. Ann Hematol 103, 759–769 (2024). https://doi.org/10.1007/s00277-024-05623-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05623-0