Abstract
Acute promyelocytic leukemia (APL) is a highly curable hematologic malignancy in the era of all-trans retinoic acid (ATRA) combination treatment. However, only a modest change in early mortality rate has been observed despite the wide availability of ATRA. In addition to the clinical characteristics of APL patients, studies on the hospital volume-outcome relationship and the physician volume-outcome relationship remained limited. We aim to evaluate the association between hospital and physician volume and the early mortality rate among APL patients. The patients were collected from Taiwan’s National Health Insurance Research Database (NHIRD). Early mortality is defined as death within 30 days of diagnosis. Patients were categorized into four groups according to individual cumulative hospital and physician volume. The risk of all-cause mortality in APL patients with different cumulative volume groups was compared using a Cox proportional hazard model. The probability of overall survival was estimated using the Kaplan–Meier method. All 741 patients were divided into four quartile volume groups. In the multivariate analysis, only physician volume was significantly associated with early mortality rate. The physician volume of the highest quartile was a protective factor for early mortality compared with the physician volume of the lowest quartile (HR 0.10, 95% CI 0.02–0.65). Hospital characteristics were not associated with early mortality. In the sensitivity analyses, the results remained consistent using two other different definitions of early mortality. Higher physician volume was independently associated with lower early mortality, while hospital volume was not. Enhancing the clinical expertise of low-volume physicians may ensure better outcomes.
Similar content being viewed by others
Introduction
Acute promyelocytic leukemia (APL) is a subtype of acute myeloid leukemia (AML) accounting for 10 to 15% of newly diagnosed AML cases annually [1]. The specific chromosomal translocation is characterized by a translocation between the promyelocytic leukemia (PML) gene on chromosome 15 and the retinoic acid receptor α (RARA) gene on chromosome 17 [2]. The disease is characterized by severe coagulopathy, causing fatal hemorrhagic complications. In the mid-1990s, the revolutionized all-trans retinoic acid (ATRA) differentiation therapy [3,4,5,6] significantly improved 30-day early mortality by ameliorating coagulopathy and bleeding events from 26% (1988–1995) to 14% (2004–2011) [7, 8]. Since then, APL has evolved from a rapidly fatal disease to a highly curable condition with a cure rate exceeding 80% [9].
Over the past several decades, the mortality rate in the first 4–6 weeks has been reported to be less than 5% in well-designed clinical trials [10]. However, these patients were carefully selected and might not reflect the real-world situation [11]. In population-based analyses, the early mortality rate remains high (29%, median 4 days) [12]. The causes of death in these patients include delayed disease identification and lack of initial proactive treatment, leading to fatal bleeding events [13, 14]. A study reported that induction mortality was 9% among 732 patients. The major categories of mortality in induction failure were primarily hemorrhage death (5%), followed by infection (2.3%), and differentiation syndrome (1.4%) [15]. The life-threatening coagulopathy before and during induction therapy has always been the major concern of treatment failure among APL patients [1, 16, 17].
While most studies have focused on the association between clinical features and survival rate, few studies have examined the volume of treatment facilities or the effect of physician volume. Intuitively, medical centers with higher volumes were more likely to see better prognosis [18, 19]. However, previous studies usually used hospital volume to speculate on physician volume indirectly. With APL patients, the physician’s ability to recognize the disease and initiate ATRA timely is regarded as the key factor in patient outcome [20, 21]. There are also limited studies investigating the independent role of physicians in treating APL and its association with early mortality. To fill this knowledge gap, we performed a nationwide population-based study to identify the impact of hospital volume and physician volume on real-world APL patients.
Materials and methods
Data source
This is a nationwide population-based retrospective cohort study. We collected data from the National Health Insurance Research Database (NHIRD). Initiated on March 1, 1995, NHIRD served as Taiwan’s single-payer mandatory insurance system. The database of this program covers more than 99.9% of the population in Taiwan. To protect patient confidentiality, data were retrieved and analyzed by on-site analysis at the Health and Wellness Data Science Center via remote connection to the Ministry of Health and Welfare server. The NHIRD contains information on the demographic characteristics of hospitals and physicians, ambulatory care, admissions, procedures, diagnoses, and prescribed medications. The diagnosis coding system was used following the International Classification of Diseases (ICD) revision 9th and 10th system to classify diagnostic, health services utilization, and death data.
Study population
Patients enrolled in this study were newly diagnosed with APL and registered in the Registry for Catastrophic Illness Patients (RCIP) between January 1, 2000, and December 31, 2017, in Taiwan. RCIP includes people who have severe diseases, including cancer, and they receive a co-payment waiver under the NHI program by using ICD-9-CM codes 205–207. Not included are 205.1 (chronic myeloid leukemia), 206.1 (chronic monocytic leukemia), and 207.1 (chronic erythremia), and ICD-10-CM codes C92–C94 (not including C92.1, C93.1 [chronic myelomonocytic leukemia], and C94.1 [chronic erythremia]). Furthermore, the enrolled patients should receive ATRA or ATO for more than 1 week after diagnosis to avoid coding errors. Patients diagnosed at age < 20 or with antecedent cancer before the diagnosis of APL were excluded.
Variables
The primary endpoint of the study was 30-day mortality. The information on the date and cause of death is contained in the National Cause of Death Data. We define the cumulative physician volume as the total number of APL patients treated by each hematologist before treating the index patient. The definition of cumulative hospital volume is the total number of APL patients treated in this hospital right before treating the index patient. Each patient’s provider could have had different values of physician volume and hospital volume. According to the cumulative numbers of physicians and hospitals, all patients were stratified into four quartiles: lowest, middle-low, middle-high, and highest. Patient information such as age, sex, comorbidities (hypertension, diabetes mellitus, dyslipidemia, cerebrovascular accident, coronary artery disease, chronic kidney disease, and bleeding history), urbanization, and socioeconomic status were analyzed.
Furthermore, provider baseline characteristics such as hospital ownership, hospital region, accreditation level of hospital, physician age, physician sex, and physician experience were also included in the analysis.
Statistical analysis
The categorical variables were expressed as counts and proportions. We performed Pearson’s chi-squared test or Fisher’s exact test to analyze the differences between categorical variables, while the Mann–Whitney U test was used for continuous variables. The probability of overall survival (OS) was measured using the Kaplan-Meier method from the time of diagnosis to death or last follow-up. A log-rank test provided additional estimates of the group differences. Cox proportional hazard models were constructed to determine whether there were significant differences in all-cause mortality risk between different patients’ cumulative volume groups. In the multivariate analysis, we used the frailty model for Cox regression to adjust for physician-level random effects. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for risk factors.
Early mortality was defined as death within 30 days after APL diagnosis. We performed a sensitivity analysis to assess the influence of different definitions of early mortality, which were 60- and 90-day mortality, and adjusted for patient and physician characteristics. All statistical tests were two-sided, and the significance level was set at 0.05. All data were analyzed with SAS 9.4 software (SAS Institute Inc., Cary, NC) and STATA statistical software, version 15.1 (StataCorp, College Station, TX). The present study was approved by the Institutional Review Board at Taipei Veterans General Hospital (no. 2019-07-054BC).
Results
Clinical characteristics of the study population
Our study cohort included 874 patients with newly diagnosed APL between January 1, 2000, and December 31, 2018, a 19-year time span. Patients younger than age 20 (n = 67) or those with antecedent cancer (n = 66) were excluded. A total of 741 patients with APL were eligible for the study (Fig. 1).
The patients’ baseline characteristics are shown in Table 1. The median age at diagnosis was 47 (range 20 to 88). A total of 429 patients (57.9%) were less than 50 years of age, and 53.6% were male. The majority of patients were treated in medical centers (88.5%). The median cumulative volume was 8 (IQR 4–13) for physicians and 30 (IQR 13–58) for hospitals. A total of 187 physicians included for analysis were classified into four degrees of volume, including lowest, middle-low, middle-high, and highest. Patients treated by physicians with higher physician volume were more likely to be treated in medical centers (75.4%, 86.0%, 94.9%, and 96.6%, respectively, from the first to fourth quartile, p < 0.001). Higher physician-volume groups were more likely to be treated by physicians over 45 years old (32.8%, 35.5%, 44.4%, and 51.9%, respectively, from the first to fourth quartile, p < 0.001). The treatment of this cohort involved 364 patients (49.1%) treated with physicians whose experience was ≥ 5 years. Patients in the higher physician-volume group were more likely to be treated by experienced (≥ 5 years) physicians (4.4%, 27.3%, 67.4%, and 90.9%, respectively, from the 1st to the 4th quartile, p < 0.001). There were only eight patients in the lowest physician volume group (4.4% of 183 patients) treated by experienced physicians, 47 patients in the middle-low physician volume group (27.3% of 172 patients), 120 patients in the middle-high physician volume group (67.4% of 178), and 189 patients in the highest physician volume group (90.9% of 208).
Higher hospital volume tended to have a higher proportion of public ownership (26.6%, 35.2%, 42.6%, and 54.8%, respectively, from the first to fourth quartile) (Supplementary Table 1). There was also a higher percentage of patients treated in medical centers with higher hospital volume (62%, 90.7%, 100%, and 100%, respectively, from the first to the fourth quartile). All the patients in the middle-high and the highest hospital volume were treated in medical centers. The characteristics of patients treated by the lowest hospital volume had fewer risks of dyslipidemia, but other comorbidities were similar among all volumes of hospitals. Higher-volume hospitals tended to have more patients treated by experienced physicians (16.4%, 38.9%, 67.2%, and 72.9%, respectively, from the first to fourth quartile).
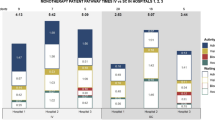
Overall survival and risk factors of mortality
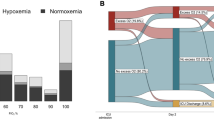
In univariate analysis, the highest quartile physician volume was a significant protective factor for 30-day early mortality (HR 0.17, 95% CI 0.04–0.79; p = 0.023). In contrast, hospital volume, location, and medical center status were not associated with early mortality. In the multivariate analysis, after adjusting for patient and physician characteristics, patients treated by the highest physician volume saw a protective factor in 30-day mortality (HR 0.10, 95% CI 0.02–0.65) (Table 2). In the sensitivity analysis, we used two other alternative follow-up durations of mortality, which were 60- and 90-day mortality. The findings for these durations were comparable to those for 30-day mortality, with adjusted HR 0.06 (95% CI 0.01–0.39; p = 0.003) in 60-day mortality and adjusted HR 0.08 (95% CI 0.02–0.37; p = 0.001) in 90-day mortality, respectively, in Table 3. When examining the long-term effect over a period of 5 years, the middle-high-volume physician group did not exhibit a significant reduction in 30- or 90-day early mortality. However, they did show improved long-term outcomes, with reduced 5-year mortality rates (adjusted HR 0.48, 95% CI 0.26–0.90; p = 0.021). The highest physician volume was a significantly predictor of 5-year survival (adjusted HR 0.27, 95% CI 0.13–0.58; p = 0.001). The Kaplan–Meier curves show that patients in the higher physician volume group had significantly better 3-month overall survival (log-rank test p = 0.016, Fig. 2B), while there was no survival difference between patients in different hospital volume groups (log-rank test p = 0.181, Fig. 2A).
Discussion
In this nationwide population-based cohort, we investigated the early mortality of newly diagnosed APL patients who received therapy in different hospitals and with different physician volumes. Our study reveals that patients in the higher-physician volume group, not hospital volume, were associated with reduced early mortality. Consistent with the initial discovery that higher physician volume was independently associated with lower early mortality. The effects persisted across the early and 5-year endpoints. These results emphasize that the physician’s role appears to have both short- and long-term benefits for acute promyelocytic leukemia patients in APL treatment.
We included 741 patients with newly diagnosed APL in the study. In Table 1, it can be seen that a relatively higher portion of patients were treated in medical centers (88.5%), and only 11.5% of the patients were treated in non-medical centers. In Taiwan, which is affected by the national medical system, patients can get treatment in medical centers without referral and have good healthcare accessibility [22]. Therefore, most patients in Taiwan were treated in medical centers (67–84%) [23]. On the contrary, studies in Western countries investigating the association between care location and hematological malignancies have shown that more patients were treated in community hospitals (75%) than medical centers (25%) [24]. The disparate conditions may make it hard to clarify the impact between facilities’ resources and physicians’ experiences. In our study, the cumulative hospital volume was not associated with early mortality. This was different from previous literature’s findings. Ho et al.’s study noted that AML patients who were treated in high-volume designated cancer centers had a 53% reduction in the odds of death compared to those treated in low-volume hospitals (OR 0.46, CI 0.40–0.54) at 60 days of diagnosis [24]. Another study on APL reported that patients who were treated at academic medical centers had lower 30-day mortality (22% vs. 25%, p = 0.03). However, the explanation was attributed to experts’ appropriate initial care in the early stages of APL [25].
APL is one of the most highly curable cancers, with a complete remission rate of 80–90%. The risk of early death ranges from 17.3 to 29% in population-based analyses [12, 26]. Previous studies have reported that the differences in early death rates between medical providers might indicate delayed diagnosis and inadequate access to care [26, 27]. As shown in Table 2, we found that the highest physician volume demonstrates a negative association with early mortality rates. Experienced physicians are highly vigilant in recognizing the disease and managing early complications. Similar to those with acute coronary syndrome (ACS), clinical outcomes can be dramatically improved once ACS has been identified and treated with early intervention [28]. For patients undergoing primary percutaneous coronary intervention (PCI), the risk-adjusted mortality rate for high-volume physicians was 3.8% versus 6.5% for low-volume physicians (OR 0.58, 95% CI 0.39–0.86) [28, 29]. Similarly, with well-trained clinicians, the APL outcome discrepancy may become less evident between medical providers [30, 31].
In Fig. 2, survival in APL patients and physician volumes appear to stabilize 2 months after the initial diagnosis. Similar results were found in studies examining outcomes in APL patients. They found that survival declined sharply in the first 2 months after APL diagnosis due to hemorrhage complications but declined at a much lower rate afterward [26]. Early mortality continues to be a primary reason for decreased survival probability [13].
Historically, the physician-outcome relationship has been investigated in several diseases. A study found increased 1-year mortality rates in low-volume physician groups among heart failure patients (HR 8.64, 95% CI 2.07–36.0)[32]. With gastric cancer, a higher surgeon volume was associated with a lower 30-day mortality rate (OR 0.94, 95% CI 0.90–0.97) [33]. With colorectal cancer, however, with differences in the volume thresholds, benefits due to physicians have been inconsistently observed [34]. With hematologic malignancies, limited studies have investigated the physician-outcome relationship. Common pitfalls of the previous studies, including lack of comprehensive adjustment and physician volume, were not analyzed independently and might confound with hospital volume [24, 35, 36]. Our study, so far, is the first to demonstrate the independent physician volume effect on APL patients’ early mortality rate. The results are further consistently confirmed in different definitions of early mortality.
This study had several limitations. Due to data constraints, omitted variables might likely be another source of bias. Certain clinical information, such as white blood cell count, disseminated intravascular coagulation profile, treatment response, as well as other behavioral variables like body mass index and smoking history, were not included in our analysis as controlled variables. However, we had considered all relevant factors that could potentially confound the results with a comprehensive multivariable analysis. Second, our study lacked cytogenetic and mutation data. Therefore, in addition to the ICD diagnosis code, we required patients to receive at least 1 week of ATRA or ATO for inclusion to avoid coding errors. Third, inevitably, in the retrospective study design, selection bias could occur and might be related to the outcome. However, to the best of our knowledge, this study remains the first Asian population-based study to show real-world outcomes of APL patients.
In summary, physician volume independently improves APL patient outcomes by reducing early mortality, while hospital volume does not. These results highlight that applying quality improvement and physician training can be essential to improving APL treatment outcomes.
References
Chen C, Huang X, Wang K, Chen K, Gao D, Qian S (2018) Early mortality in acute promyelocytic leukemia: potential predictors. Oncol Lett 15(4):4061–4069. https://doi.org/10.3892/ol.2018.7854
Tallman MS, Altman JK (2009) How I treat acute promyelocytic leukemia. Blood 114(25):5126–5135. https://doi.org/10.1182/blood-2009-07-216457
Huang ME, Ye YC, Chen SR, Chai JR, Lu JX, Zhoa L, Gu LJ, Wang ZY (1988) Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia. Blood 72(2):567–572
Jacomo RH, Melo RA, Souto FR, de Mattos ER, de Oliveira CT, Fagundes EM, Bittencourt HN, Bittencourt RI, Bortolheiro TC, Paton EJ, Bendlin R, Ismael S, Chauffaille Mde L, Silva D, Pagnano KB, Ribeiro R, Rego EM (2007) Clinical features and outcomes of 134 Brazilians with acute promyelocytic leukemia who received ATRA and anthracyclines. Haematologica 92(10):1431–1432. https://doi.org/10.3324/haematol.10874
Chen Y, Kantarjian H, Wang H, Cortes J, Ravandi F (2012) Acute promyelocytic leukemia: a population-based study on incidence and survival in the United States, 1975-2008. Cancer 118(23):5811–5818. https://doi.org/10.1002/cncr.27623
Tallman MS, Andersen JW, Schiffer CA, Appelbaum FR, Feusner JH, Ogden A, Shepherd L, Willman C, Bloomfield CD, Rowe JM, Wiernik PH (1997) All-trans-retinoic acid in acute promyelocytic leukemia. N Engl J Med 337(15):1021–1028. https://doi.org/10.1056/NEJM199710093371501
Guru Murthy GS, Szabo A, Michaelis L, Carlson KS, Runaas L, Abedin S, Atallah E (2020) Improving outcomes of acute promyelocytic leukemia in the current era: analysis of the SEER Database. J Natl Compr Cancer Netw 18(2):169–175. https://doi.org/10.6004/jnccn.2019.7351
Abrahao R, Ribeiro RC, Medeiros BC, Keogh RH, Keegan TH (2015) Disparities in early death and survival in children, adolescents, and young adults with acute promyelocytic leukemia in California. Cancer 121(22):3990–3997. https://doi.org/10.1002/cncr.29631
Lo-Coco F, Avvisati G, Vignetti M, Thiede C, Orlando SM, Iacobelli S, Ferrara F, Fazi P, Cicconi L, Di Bona E, Specchia G, Sica S, Divona M, Levis A, Fiedler W, Cerqui E, Breccia M, Fioritoni G, Salih HR et al (2013) Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med 369(2):111–121. https://doi.org/10.1056/NEJMoa1300874
Iland HJ, Collins M, Bradstock K, Supple SG, Catalano A, Hertzberg M, Browett P, Grigg A, Firkin F, Campbell LJ, Hugman A, Reynolds J, Di Iulio J, Tiley C, Taylor K, Filshie R, Seldon M, Taper J, Szer J et al (2015) Use of arsenic trioxide in remission induction and consolidation therapy for acute promyelocytic leukaemia in the Australasian Leukaemia and Lymphoma Group (ALLG) APML4 study: a non-randomised phase 2 trial. Lancet Haematol 2(9):e357–e366. https://doi.org/10.1016/S2352-3026(15)00115-5
Dhakal P, Lyden E, Rajasurya V, Zeidan AM, Chaulagain C, Gundabolu K, Bhatt VR (2021) Early mortality and overall survival in acute promyelocytic leukemia: do real-world data match results of the clinical trials? Leuk Lymphoma 62(8):1949–1957. https://doi.org/10.1080/10428194.2021.1894651
Lehmann S, Ravn A, Carlsson L, Antunovic P, Deneberg S, Mollgard L, Derolf AR, Stockelberg D, Tidefelt U, Wahlin A, Wennstrom L, Hoglund M, Juliusson G (2011) Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia 25(7):1128–1134. https://doi.org/10.1038/leu.2011.78
Ho G, Li Q, Brunson A, Jonas BA, Wun T, Keegan THM (2018) Complications and early mortality in patients with acute promyelocytic leukemia treated in California. Am J Hematol 93(11):E370–E372. https://doi.org/10.1002/ajh.25252
Larson RA, Kondo K, Vardiman JW, Butler AE, Golomb HM, Rowley JD (1984) Evidence for a 15;17 translocation in every patient with acute promyelocytic leukemia. Am J Med 76(5):827–841. https://doi.org/10.1016/0002-9343(84)90994-x
de la Serna J, Montesinos P, Vellenga E, Rayon C, Parody R, Leon A, Esteve J, Bergua JM, Milone G, Deben G, Rivas C, Gonzalez M, Tormo M, Diaz-Mediavilla J, Gonzalez JD, Negri S, Amutio E, Brunet S, Lowenberg B, Sanz MA (2008) Causes and prognostic factors of remission induction failure in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and idarubicin. Blood 111(7):3395–3402. https://doi.org/10.1182/blood-2007-07-100669
Tallman MS, Andersen JW, Schiffer CA, Appelbaum FR, Feusner JH, Woods WG, Ogden A, Weinstein H, Shepherd L, Willman C, Bloomfield CD, Rowe JM, Wiernik PH (2002) All-trans retinoic acid in acute promyelocytic leukemia: long-term outcome and prognostic factor analysis from the North American Intergroup protocol. Blood 100(13):4298–4302. https://doi.org/10.1182/blood-2002-02-0632
Altman JK, Rademaker A, Cull E, Weitner BB, Ofran Y, Rosenblat TL, Haidau A, Park JH, Ram SL, Orsini JM Jr, Sandhu S, Catchatourian R, Trifilio SM, Adel NG, Frankfurt O, Stein EM, Mallios G, Deblasio T, Jurcic JG et al (2013) Administration of ATRA to newly diagnosed patients with acute promyelocytic leukemia is delayed contributing to early hemorrhagic death. Leuk Res 37(9):1004–1009. https://doi.org/10.1016/j.leukres.2013.05.007
Jillella AP, Arellano ML, Gaddh M, Langston AA, Heffner LT, Winton EF, McLemore ML, Zhang C, Caprara CR, Simon KS, Bolds SL, DeBragga S, Karkhanis P, Krishnamurthy SH, Tongol J, El Geneidy MM, Pati A, Gerber JM, Grunwald MR et al (2021) Comanagement strategy between academic institutions and community practices to reduce induction mortality in acute promyelocytic leukemia. JCO Oncol Pract 17(4):e497–e505. https://doi.org/10.1200/OP.20.00395
Pant M, Bhatt VR (2017) Early mortality and survival in older adults with acute myeloid leukemia. Int J Hematol Oncol 6(3):61–63. https://doi.org/10.2217/ijh-2017-0013
Breccia M, Latagliata R, Cannella L, Minotti C, Meloni G, Lo-Coco F (2010) Early hemorrhagic death before starting therapy in acute promyelocytic leukemia: association with high WBC count, late diagnosis and delayed treatment initiation. Haematologica 95(5):853–854. https://doi.org/10.3324/haematol.2009.017962
Rashidi A, Riley M, Goldin TA, Sayedian F, Bayerl MG, Aguilera NS, Vos JA, Goudar RK, Fisher SI (2014) Delay in the administration of all-trans retinoic acid and its effects on early mortality in acute promyelocytic leukemia: final results of a multicentric study in the United States. Leuk Res 38(9):1036–1040. https://doi.org/10.1016/j.leukres.2014.06.011
Wu TY, Majeed A, Kuo KN (2010) An overview of the healthcare system in Taiwan. London J Prim Care (Abingdon) 3(2):115–119. https://doi.org/10.1080/17571472.2010.11493315
Wang CY, Huang HH, Chen HM, Hsiao FY, Ko BS (2021) Real-world outcomes of patients with acute myeloid leukemia in Taiwan: a nationwide population-based study, 2011-2015. Clin Lymphoma Myeloma Leuk 21(8):e649–e657. https://doi.org/10.1016/j.clml.2021.03.010
Ho G, Wun T, Muffly L, Li Q, Brunson A, Rosenberg AS, Jonas BA, Keegan THM (2018) Decreased early mortality associated with the treatment of acute myeloid leukemia at National Cancer Institute-designated cancer centers in California. Cancer 124(9):1938–1945. https://doi.org/10.1002/cncr.31296
Stahl M, Tallman MS (2019) Acute promyelocytic leukemia (APL): remaining challenges towards a cure for all. Leuk Lymphoma 60(13):3107–3115. https://doi.org/10.1080/10428194.2019.1613540
Park JH, Qiao B, Panageas KS, Schymura MJ, Jurcic JG, Rosenblat TL, Altman JK, Douer D, Rowe JM, Tallman MS (2011) Early death rate in acute promyelocytic leukemia remains high despite all-trans retinoic acid. Blood 118(5):1248–1254. https://doi.org/10.1182/blood-2011-04-346437
Wong WF, LaVeist TA, Sharfstein JM (2015) Achieving health equity by design. JAMA 313(14):1417–1418. https://doi.org/10.1001/jama.2015.2434
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, American College of C, American Heart A, Canadian Cardiovascular S (2004) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol 44(3):671–719. https://doi.org/10.1016/j.jacc.2004.07.002
Srinivas VS, Hailpern SM, Koss E, Monrad ES, Alderman MH (2009) Effect of physician volume on the relationship between hospital volume and mortality during primary angioplasty. J Am Coll Cardiol 53(7):574–579. https://doi.org/10.1016/j.jacc.2008.09.056
Bewersdorf JP, Prozora S, Podoltsev NA, Shallis RM, Huntington SF, Neparidze N, Wang R, Zeidan AM, Davidoff AJ (2022) Practice patterns and real-life outcomes for patients with acute promyelocytic leukemia in the United States. Blood Adv 6(2):376–385. https://doi.org/10.1182/bloodadvances.2021005642
Rego EM, Kim HT, Ruiz-Arguelles GJ, Undurraga MS, Uriarte Mdel R, Jacomo RH, Gutierrez-Aguirre H, Melo RA, Bittencourt R, Pasquini R, Pagnano K, Fagundes EM, Chauffaille Mde L, Chiattone CS, Martinez L, Meillon LA, Gomez-Almaguer D, Kwaan HC, Garces-Eisele J et al (2013) Improving acute promyelocytic leukemia (APL) outcome in developing countries through networking, results of the International Consortium on APL. Blood 121(11):1935–1943. https://doi.org/10.1182/blood-2012-08-449918
Lee JE, Park EC, Jang SY, Lee SA, Choy YS, Kim TH (2018) Effects of physician volume on readmission and mortality in elderly patients with heart failure: nationwide cohort study. Yonsei Med J 59(2):243–251. https://doi.org/10.3349/ymj.2018.59.2.243
Ji J, Shi L, Ying X, Lu X, Shan F (2022) Associations of annual hospital and surgeon volume with patient outcomes after gastrectomy: a systematic review and meta-analysis. Ann Surg Oncol 29(13):8276–8297. https://doi.org/10.1245/s10434-022-12515-y
Hillner BE, Smith TJ, Desch CE (2000) Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol 18(11):2327–2340. https://doi.org/10.1200/JCO.2000.18.11.2327
Giri S, Pathak R, Aryal MR, Karmacharya P, Bhatt VR, Martin MG (2015) Impact of hospital volume on outcomes of patients undergoing chemotherapy for acute myeloid leukemia: a matched cohort study. Blood 125(21):3359–3360. https://doi.org/10.1182/blood-2015-01-625764
Go RS, Bartley AC, Al-Kali A, Shah ND, Habermann EB (2016) Effect of the type of treatment facility on the outcome of acute myeloid leukemia in adolescents and young adults. Leukemia 30(5):1177–1180. https://doi.org/10.1038/leu.2015.23
Funding
Open Access funding enabled and organized by National Yang Ming Chiao Tung University. This study was supported by grants from Taipei Veterans General Hospital (V111C-030 and V111B-030), the Ministry of Science and Technology (MOST 109-2314-B-A49A-503-MY2 and MOST 111-2314-B-A49-034-), the Taiwan Clinical Oncology Research Foundation, the Szu-Yuan Research Foundation of Internal Medicine, the Yen Tjing Ling Medical Foundation, Melissa Lee Cancer Foundation, and the Chong Hin Loon Memorial Cancer and Biotherapy Research Center, National Yang-Ming University. The funding sources had no role in the study design or conduct, or in the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
C-KT and C-JL had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. C-YW, C-KT, and C-MY designed the study. C-YW and C-MY acquired the data and performed the statistical analysis. C-YW, C-KT, C-MY, and C-JL provided the final interpretation of the results. C-YW, C-KT, and C-JL drafted the manuscript. C-YW, C-KT, and C-JL made critical revisions to the manuscript for important intellectual content. C-MY, C-KT, and C-JL provided administrative, technical, and material support. C-KT and C-JL were the study supervisors, act as guarantors, and accept responsibility for the integrity of the work as a whole. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent to participate
Patient consent was not required and the study was granted an exemption from ethical review by the Taipei Veterans General Hospital.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 26 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, CY., Yeh, CM., Tsai, CK. et al. The influence of hospital volume and physician volume on early mortality in acute promyelocytic leukemia patients. Ann Hematol 103, 1577–1586 (2024). https://doi.org/10.1007/s00277-024-05616-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05616-z