Abstract
The VEXAS syndrome, a genetically defined autoimmune disease, associated with various hematological neoplasms has been attracting growing attention since its initial description in 2020. While various therapeutic strategies have been explored in case studies, the optimal treatment strategy is still under investigation and allogeneic cell transplantation is considered the only curative treatment. Here, we describe 2 patients who achieved complete molecular remission of the underlying UBA1 mutant clone outside the context of allogeneic HCT. Both patients received treatment with the hypomethylating agent azacitidine, and deep molecular remission triggered treatment de-escalation and even cessation with sustained molecular remission in one of them. Prospective studies are necessary to clarify which VEXAS patients will benefit most from hypomethylating therapy and to understand the variability in the response to different treatment strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first description in 2020, the VEXAS syndrome (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic), a genetically defined auto-inflammatory disease associated with hematological abnormalities, has gained increasing attention [1]. With 1:4000–1:14000 cases in the general population [2], the disease prevalence is much higher than initially expected. Clinical inflammatory manifestations are variable and often resistant to conventional immunosuppressive treatments. The majority of patients exhibit hematological abnormalities, including myelodysplastic neoplasm (MDS), macrocytic anemia, monoclonal gammopathy, and multiple myeloma [3]. Disease pathogenesis is linked to a loss of UBA1 function by acquired somatic mutations, most frequently affecting methionine 41 (p.M41) of the UBA1 gene, which codes for the E1 enzyme that regulates protein ubiquitination. Reduced ubiquitination mediates activation of the innate immune system and synthesis of proinflammatory cytokines, such as interleukin (IL)-1, IL-6, IL-8, interferon, and tumor necrosis factor alpha [1], which contribute to the inflammatory phenotype of VEXAS syndrome.
Various therapeutic strategies have been described in case studies, ranging from steroids over azacitidine [4, 5] to ruxolitinib [6] and allogeneic hematopoietic cell transplantation (alloHCT) [7, 8]. The latter has been considered the only curative treatment option so far. Here we report for the first time complete molecular clearance of the underlying UBA1 mutation in two VEXAS patients (Table 1) who underwent treatment with the hypomethylating agent azacitidine (5-Aza), leading to treatment de-escalation. Written informed consent for clinical follow-up and detailed molecular diagnostics were obtained from both patients before treatment start.
Case description
Patient 1
A 72-year-old man presented with a 6-month history of recurrent fever, arthralgias, nodular erythema, enlarged mesenterial lymph nodes, macrocytic anemia, night sweats, and 10 kg of weight loss. Lymph node biopsy showed no pathological findings. He was started on prednisolone 1 mg/kg and initially responded well but remained steroid-dependent at 20 mg/day. Colchicine, dapsone, and interleukin-1 blockade had no longer-lasting benefit. Instead, the patient developed further deterioration with pneumonitis and respiratory impairment, leading to wheelchair mobility.
A bone marrow biopsy in 3/2019 revealed MDS with increased blasts (MDS-IB1) and del(20q), while molecular alterations were not detected (note that UBA1 was not analyzed at this time). According to the Molecular International Prognostic Scoring System (IPSS-M), a moderate-high-risk MDS was diagnosed, with autoinflammatory features. Due to severe symptoms and steroid dependence, treatment with the hypomethylating agent (HMA) azacitidine 75 mg subcutaneously on days 1–7 every 28 days was initiated. The autoinflammatory symptoms resolved after 2 cycles, and blood counts normalized after 4 cycles. Notably, steroids could be discontinued during the first 2 cycles.
After the description of VEXAS syndrome in 2020 [1], we retrospectively sequenced DNA from initial diagnosis by next-generation sequencing (NGS) and identified an UBA1 (c.118-1G > C) mutation. Longitudinal molecular follow-up using ultradeep NGS with a detection limit of 0.1% [9] revealed complete clearance of this UBA1-mutant clone in the bone marrow 6 months after treatment start. At this timepoint, also MDS del(20q) was in complete cytogenetic remission.
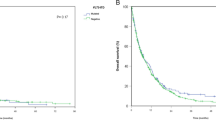
Due to the rapid response, 5-Aza treatment was reduced to 5 days and cycle administration extended to every 6–8 weeks. Treatment was ultimately discontinued in March 2023. As of October 2023, the patient continues to demonstrate ongoing hematological, clinical, and molecular remission (see Fig. 1).
Variant allele frequencies (VAF) of the UBA1 mutation during azacitidine treatment. Left: UBA1 VAF in CD34-selected peripheral blood (pB) during the first 6 treatment cycles. Right: UBA1 VAF in unsorted BM cells. Ultradeep NGS with a detection limit of 0.1%9 was used for longitudinal molecular follow-up. Patient 1 (yellow) achieved complete eradication of the UBA1 clone 6 months after azacitidine start. Follow-up assessments in patient 2 (blue) identified complete molecular remission at month 21 after treatment start
Patient 2
In 2019, a 68-year-old male patient was referred with progressive arthralgias, weight loss, and recurrent fever episodes over the past 2 years. He had a history of spontaneous deep vein thrombosis of the leg 2 years before (low molecular weight heparins were already stopped) and mild macrocytic anemia. High-dose steroids provided temporary relief, while the use of methotrexate, azathioprine, and interleukin-1 blockade, which were initially prescribed for suspected polymyalgia rheumatica, did not yield significant improvement. At the time of presentation, high fever episodes were present, along with erythematous subcutaneous nodules, confirmed as Sweet syndrome through biopsy. A PET-CT scan revealed no signs of malignancy or vasculitis but showed significant bone marrow activation. Bone marrow biopsy revealed MDS-IB1 (WHO 2022), without cytogenetic abnormalities. Molecular analysis identified a low level TET2 mutation (VAF 0.9%). Diagnosis of MDS with very low risk (according to IPSS-M) and autoinflammatory symptoms was made and azacitidine 75mg on days 1-7 subcutaneously was initiated due to severe clinical course. HMA treatment led to a rapid clinical response with complete regression of the rash and joint symptoms. Steroids could be tapered off during the first 2 cycles.
NGS resequencing detected the UBA1 p.M41T (c.122 T > C) mutation confirming VEXAS syndrome and follow-up assessments identified complete molecular remission at month 21 after treatment start, in accordance with complete molecular remission of the underlying MDS. This observation prompted dose reduction of 5-Aza to 5-day cycles every 8 weeks. However, at the 30-month follow-up, a low-level UBA1 mutation (VAF 0.013%) temporarily reappeared. Since then, the patient has consistently been in complete clinical, hematological, and molecular remission.
Results and discussion
Longitudinal molecular monitoring of the UBA1-mutated clone during 5-Aza therapy revealed complete molecular remission 6 months (patient 1) and 21 months (patient 2) after treatment start.
To our knowledge, this is the first report describing complete molecular clearance of the UBA1-mutant clone in two VEXAS patients outside the context of alloHCT. While some authors have reported the suppression of the UBA1-mutant clone after HMA therapy [10], complete molecular clearance had not been observed until yet.
To further corroborate the depth of remission, we performed molecular monitoring using ultradeep NGS with a detection limit of 0.1% (median coverage > 100,000 reads) in CD34-selected peripheral blood (pB) (Fig. 1), which has a calculated overall sensitivity of 0.01–0.001% [9], indicating a very deep molecular clearance of the mutation.
Azacitidine, a hypomethylating agent approved for high-risk MDS and commonly recommended for patients with MDS and autoinflammatory features [4], has already been successfully used to treat autoinflammatory symptoms in VEXAS syndrome [4, 5]. Besides direct cytotoxic effects, azacitidine modulates the cytokine profile with downregulation of proinflammatory cytokines and impacts the bone marrow microenvironment [11], which might contribute to its positive effect on autoinflammatory sequelae.
In our patients, azacitidine treatment not only resulted in clinical and hematological remissions but also induced complete molecular eradication of the underlying UBA1-mutated clone, below the detection limit of our method, clearly documenting the profound and specific effect on the mutant population.
Notably, steroids could be tapered within 2 months of treatment indicating that 5-Aza alone was sufficient to maintain remission in these patients. Nevertheless, the underlying mechanism by which 5-Aza impacts the UBA1 clonal burden is not clear, although direct cytotoxic effects have been described and a synthetic lethal interaction with the UBA1 clone has been speculated [12]. Prospective studies are necessary to clarify which VEXAS patients will benefit mostly from hypomethylating therapy, since different mutations may lead to differences in prognosis, phenotype, or even treatment responses.
To date, the three most common mutations in VEXAS syndrome impact methionine 41 in exon 3 of the UBA1 gene, namely p.M41Thr (c.122 T > C), p.M41Val (c.121A > G), and p.M41Leu (c.121A > C) [1]. In addition, non-M41 gene mutations have been described, such as splice site mutations at exon 3 (c.118-2A > C, c.118-1G > C, c.118-9_118-2del) and mutations affecting codon 56 (c.167C > T) [13, 14]. In our case, patient 2 exhibited the common p.M41Thr mutation, while patient 1 who successfully discontinued HMA therapy had the UBA1 (c.118-1G > C) mutation, affecting the splice region at exon 3. Recently, Georgin-Lavialle [15] has described that the UBA1 p.M41Leu mutation is associated with a milder phenotype and a better 5-year survival rate compared to p.M41Val and p.M41Thr. However, a clear genotype-phenotype correlation, or even a correlation of certain mutations with responses to specific treatment strategies, has not yet been established.
The deep molecular response observed in our patients prompted us to consider treatment de-escalation with dose reduction of 5-Aza from 7 to 5 days, followed by treatment cycle extension to every 6 to 8 weeks, and ultimately treatment discontinuation in patient 1 after 44 months. Notably, he remained in sustained complete molecular remission 6 months after treatment discontinuation. However, the second patient temporarily exhibited a very low-level UBA1 mutation at month 30 during 5-Aza therapy, suggesting the persistence of UBA1-mutated cells in the quiescent stem cell pool, similar to the “leukemia stem cell persistence” observed in chronic myeloid leukemia [16]. Further prospective studies are necessary to clarify whether low-level minimal residual disease (MRD) or even complete clearance can guide safe treatment de-escalation. Close MRD monitoring in those patients is essential. Indeed, NGS in CD34+ -enriched pB cells provides a more sensitive detection of MRD compared to unsorted BM cells, as recently described [9, 17].
Co-mutations in VEXAS syndrome predominantly involve epigenetic regulators and splicing factors. DNMT3A and TET2, well-known for their association with inflammatory conditions, were the most commonly observed [18]. We also detected a low-level TET2 co-mutation in one of our patients, which may be indicative of clonal hematopoiesis due to its low VAF. However, due to multilineage dysplasia, increased blast cell count, and cytopenia, the diagnosis of MDS was established.
Of note, in both patients, 5-Aza not only addressed the VEXAS syndrome but also achieved complete remission of the associated MDS disease, including hematological, cytogenetic (case 1), and molecular (case 2) aspects. Neither additional myeloid mutations nor novel cytogenetic alterations could be observed during the follow-up phase. The exact relationship between the UBA1-mutant clone and the initiation of MDS is yet to be determined. It remains uncertain whether the myeloid neoplasm is primarily driven by the UBA1-mutant clone or whether the highly inflammatory microenvironment promotes clonal selection.
In addition to azacitidine, further treatment approaches have been described in small VEXAS cohorts. Among them, the JAK1/2 inhibitor ruxolitinib is considered one of the most promising, which has successfully alleviated symptoms of VEXAS syndrome; however, no molecular remissions have been reported thus far. Indeed, a recent publication reported an increase in UBA1 burden under ruxolitinib, despite a highly favorable clinical response [8].
In conclusion, detailed molecular monitoring of two VEXAS syndrome patients who underwent HMA therapy revealed complete eradication of the UBA1 clone along with significant clinical and hematologic responses. Thus, hypomethylating agents might be an interesting alternative, at least for a proportion of patients, not eligible for alloHCT. Clearly, this report is based on a limited number of cases, and prospective studies are required to validate these findings and identify which VEXAS patients will benefit most from HMA.
Data availability
No datasets were generated or analysed during the current study.
References
Beck DB, Ferrada MA, Sikora KA et al (2020) Somatic mutations in UBA1 and severe adult-onset autoinflammatory disease. N Engl J Med. 383(27):2628–2638. https://doi.org/10.1056/NEJMoa2026834
Beck DB, Bodian DL, Shah V et al (2023) Estimated prevalence and clinical manifestations of UBA1 variants associated with VEXAS syndrome in a clinical population. JAMA 329(4):318–324. https://doi.org/10.1001/jama.2022.24836
Obiorah IE, Patel BA, Groarke EM et al (2021) Benign and malignant hematologic manifestations in patients with VEXAS syndrome due to somatic mutations in UBA1. Blood Adv 5(16):3203–3215. https://doi.org/10.1182/bloodadvances.2021004976
Mekinian A, Zhao LP, Chevret S et al (2022) A phase II prospective trial of azacitidine in steroid-dependent or refractory systemic autoimmune/inflammatory disorders and VEXAS syndrome associated with MDS and CMML. Leukemia 36(11):2739–2742. https://doi.org/10.1038/s41375-022-01698-8
Comont T, Heiblig M, Rivière E et al (2022) Azacitidine for patients with vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic syndrome (VEXAS) and myelodysplastic syndrome: data from the French VEXAS registry. Br J Haematol 196(4):969–974. https://doi.org/10.1111/bjh.17893
Heiblig M, Ferrada MA, Koster MJ et al (2022) Ruxolitinib is more effective than other JAK inhibitors to treat VEXAS syndrome: a retrospective multicenter study. Blood. 140(8):927–931. https://doi.org/10.1182/blood.2022016642
Gurnari C, McLornan DP (2022) Update on VEXAS and role of allogeneic bone marrow transplant: considerations on behalf of the Chronic Malignancies Working Party of the EBMT. Bone Marrow Transplant 57(11):1642–1648. https://doi.org/10.1038/s41409-022-01774-8
Gurnari C, Pascale MR, Vitale A et al (2023) Diagnostic capabilities, clinical features, and longitudinal UBA1 clonal dynamics of a nationwide VEXAS cohort. Am J Hematol. https://doi.org/10.1002/ajh.27169
Stasik S, Burkhard-Meier C, Kramer M et al (2022) Deep sequencing in CD34+ cells from peripheral blood enables sensitive detection of measurable residual disease in AML. Blood Adv 6(11):3294–3303. https://doi.org/10.1097/HS9.0000000000000661
Raaijmakers MHGP, Hermans M, Aalbers A, Rijken M, Dalm VASH, van Daele P (2021) Azacytidine treatment for VEXAS syndrome. Hemasphere 5(12):e661. https://doi.org/10.1097/HS9.0000000000000661
Wenk C, Garz AK, Grath S et al (2018) Direct modulation of the bone marrow mesenchymal stromal cell compartment by azacitidine enhances healthy hematopoiesis. Blood Adv. 2(23):3447–3461. https://doi.org/10.1182/bloodadvances.2018022053
Heiblig M, Patel BA, Groarke EM, Bourbon E, Sujobert P (2021) Toward a pathophysiology inspired treatment of VEXAS syndrome. Semin Hematol. 58(4):239–246. https://doi.org/10.1053/j.seminhematol.2021.09.001
Battipaglia G, Vincenzi A, Falconi G et al (2023) New scenarios in vacuoles, E1 enzyme, X linked, autoinflammatory, somatic (VEXAS) syndrome: evolution from myelodysplastic syndrome to acute myeloid leukemia. Curr Res Transl Med 71(2):103386. https://doi.org/10.1016/j.retram.2023.103386
Templé M, Kosmider O (2022) VEXAS syndrome: a novelty in MDS landscape. Diagnostics (Basel). 12(7):1590. https://doi.org/10.3390/diagnostics12071590
Georgin-Lavialle S, Terrier B, Guedon AF et al (2022) Further characterization of clinical and laboratory features in VEXAS syndrome: large-scale analysis of a multicentre case series of 116 French patients. Br J Dermatol. 186(3):564–574. https://doi.org/10.1111/bjd.20805
Holyoake TL, Vetrie D (2017) The chronic myeloid leukemia stem cell: stemming the tide of persistence. Blood. 129(12):1595–1606. https://doi.org/10.1182/blood-2016-09-696013
Martin R, Acha P, Ganster C et al (2018) Targeted deep sequencing of CD34+ cells from peripheral blood can reproduce bone marrow molecular profile in myelodysplastic syndromes. Am J Hematol. 93(6):E152–E154. https://doi.org/10.1002/ajh.25089
Gutierrez-Rodrigues F, Kusne Y, Fernandez J et al (2023) Spectrum of clonal hematopoiesis in VEXAS syndrome. Blood 142(3):244–259. https://doi.org/10.1182/blood.2022018774
Acknowledgements
We thank the patients for generously granting us the permission to share their cases.
Author information
Authors and Affiliations
Contributions
KS was responsible for conceptualization, patient treatment, and data interpretation, and wrote the draft. KSG contributed to conceptualization, reviewed the paper, and made insightful clinical points. MB designed the figure, discussed the results, and made insightful clinical points. CG and DH provided study material and molecular data, reviewed the manuscript, and gave feedback. JAG, EB, MA, MU, MBo and KT were involved in patient treatment, reviewed the manuscript, and gave feedback. CT was responsible for conceptualization, provided and analyzed molecular data, interpreted results, and wrote the draft. All authors participated in the discussion, reviewed, and approved the final version of the article.
Corresponding author
Ethics declarations
Ethical approval
Data were collected under written informed consent (according to the principles of the Helsinki Declaration) as part of the HMA-NGS study, which has been approved by the Institutional Ethics Committee of each participating center. Both patients gave their consent to publish their data.
Competing interests
KS served on advisory boards and received lecture fees from BMS/Celgene and Novartis. KSG received honoraria from BMS, Jazz Pharmaceuticals, and Abbvie. MA served on advisory boards for Novartis. MB served on advisory boards and received lecture fees from Jazz Pharmaceuticals and served on advisory boards from FarmaTrust. MB received travel compensation from DKMS. DH received research funding from BMS, Jazz Pharmaceuticals, and lecture fees from BMS/Celgene, Jazz Pharmaceuticals, and Novartis; he served on advisory boards for BMS, Novartis, Jazz Pharmaceuticals, Gilead, Takeda, and Hexal. CT is co-owner and CEO of AgenDix GmbH. CT has received lecture fees and/or participated in advisory boards from Novartis, Jazz Pharmaceuticals, Astellas, Janssen, and Illumina. CT has received research funding from Novartis and Bayer. CG, JAG, EB, and MU declare no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sockel, K., Götze, K., Ganster, C. et al. VEXAS syndrome: complete molecular remission after hypomethylating therapy. Ann Hematol 103, 993–997 (2024). https://doi.org/10.1007/s00277-023-05611-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05611-w