Abstract
Cytomegalovirus (CMV) reactivation following allogeneic hematopoietic stem cell transplantation (allo-HSCT) remains a challenging problem, and the impact on the risk of overall mortality (OM) and non-relapse mortality (NRM) in patients following allo-HSCT is still controversial. Utilizing the evidence mapping method, we aimed to assess the effect of CMV infection on outcomes of patients post-transplantation and identify research gaps through systematic reviews (SRs) and clinical studies. PubMed, EMBASE, Web of Science, and Cochrane library databases were searched from inception until 5 July 2022 to identify relevant literature. After systematic literature screening and data extraction, evidence mapping of the effects of CMV reactivation on patients post-allo-HSCT was conducted. Three SRs and 22 clinical studies were included. In one SR, CMV reactivation was associated with an increased risk of mortality (HR 1.46; 95% CI, 1.24–1.72; P ≤ 0.001). In two SRs, CMV reactivation was associated with NRM. One SR reported CMV reactivation was potentially associated with significant protection against relapse in patients with acute myelocytic leukemia (AML), but no significant correlation with graft-versus-host disease (GVHD) was found. Lastly, in one SR CMV reactivation significantly increased the risk of invasive fungal disease (IFD). Most clinical articles reported that CMV reactivation increased the risk of renal dysfunction, poor graft function, re-hospitalization, and bacterial infections. CMV reactivation following allo-HSCT is associated with an increased risk of OM, NRM, IFD, and renal dysfunction, as well as a reduced risk of relapse in patients with AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a potentially lifesaving treatment for patients with hematologic malignancies. However, viral infections remain an important cause of morbidity and mortality following allo-HSCT, especially cytomegalovirus (CMV) reactivation [1], which can occur both early and late post-HSCT [2, 3]. Patients who undergo allo-HSCT are more susceptible to CMV reactivation due to their immunocompromised state. A retrospective study also showed that CMV reactivation was associated with an increased risk of acute graft-versus-host disease (GVHD) in patients who received anti-thymocyte globulin-containing conditioning regimens [4]. Additionally, patients with hematological diseases such as acute myeloid leukemia (AML) and who were post-allo-HSCT are most susceptible to invasive fungal disease (IFD) after CMV reactivation [5]. Patients post-allo-HSCT with CMV seropositivity do not have a better prognosis than patients who have not undergone all-HSCT, despite advances in the diagnosis and management of CMV [3]. However, research findings have been inconsistent [6, 7]. Reactivation [8] of CMV is defined as a new occurrence of CMV antigenemia or CMV DNA in the blood (DNAemia) for patients with CMV-IgG (þ) [9]. Several single-center studies have demonstrated a link between CMV serology/early reactivation of the virus (before 100 days after HCT (D100)) and a reduction in the incidence of relapse of hematological disease [10, 11]. One study of 266 patients with acute myeloid leukemia (AML) who were post-allo-HSCT showed a reduction in the risk of leukemic relapse after early replicative of CMV reactivation, while data from 9469 patients who received a bone marrow or peripheral blood transplantation showed that reactivation of CMV remains a risk factor for poor post-transplant outcomes and does not protect against relapse [3]. In 2019, a meta-analysis of 24 eligible studies with 37,021 patients concluded that while patients with CMV replication who were post-allo-HSCT had a significantly lower risk of relapse, the risk of non-relapse mortality (NRM) was increased [12]. Furthermore, CMV replication was not associated with overall survival (OS) or GVHD disease for patients with AML. Another meta-analysis of 26 studies limited to the English language—17 studies comprising 10, 221 patients evaluated the association between CMV reactivation and the risk of overall mortality (OM), and 14 studies of 18,238 patients assessed the relationship between active CMV reactivation and risk of NRM—reported that patients post-allo-HSCT were at increased risk of OM and NRM after CMV reactivation [13]. However, the increased risk of OM might be offset by an increased risk of NRM. Both meta-analyses had a degree of heterogeneity that could have impacted the reliability of the results. Nonetheless, the above findings suggest controversy still exists about the impact of CMV reactivation on the risk of OM and NRM in patients post-allo-HSCT. Because more evidence has emerged from SRs and primary studies about patient outcomes, this study conducted evidence mapping of the published literature to further investigate the risks associated with CMV reactivation following allo-HSCT.
Materials and methods
This meta-analysis was performed following the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. This evidence mapping was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY protocol: 2,022,110,032).
Data sources and literature search
Search strategy and eligibility criteria
Relevant publications were searched by two independent researchers using the PubMed, EMBASE, Web of Science, and Cochrane library databases from inception to 5 July 2022, with the following combination of words, “hematopoietic cell,” “hematopoietic stem,” “transplant,” and “Cytomegalovirus,” limited to the English language. The search strategy used in each database is presented in Online Resource 1. The eligibility criteria were (1) patients undergoing allo-HSCT procedures; (2) patients infected with CMV; (3) systematic reviews (SRs), observational studies, or clinical trials; (4) when two or more studies from the same institution had overlapping populations and assessed the same outcome, the study with the largest number of patients was selected for analysis; (5) studies that reported the correlation between CMV reactivation and primary outcome (OM) or secondary outcomes (NRM, hematologic disease relapse, GVHD, IFD, renal dysfunction, poor graft function, re-hospitalization, and bacterial infections); and (6) because of the level of evidence, the results of systematic reviews were preferentially included and analyzed for each outcome.
Study selection
Two authors independently screened the titles and abstracts and then reviewed the full texts that met the above-mentioned criteria. Any discrepancies were discussed until a consensus was achieved. Data from published literature was included, while conference abstracts or gray literature was excluded because the data were not peer-reviewed. Furthermore, if outcomes had been reported by SRs, the clinical studies were not searched.
Data extraction
Data from each study were extracted independently by two separate reviewers. Any disagreements were resolved by discussion with the assistance of a third party if necessary. Baseline characteristics included the type of study, country, number of patients, number of deaths, type of population (allo-HSCT modality), length of follow-up, median age, frequency and duration of CMV monitoring, the method employed for such a purpose (PCR or CMV pp65 antigenemia), type of sample for CMV DNA monitoring, the threshold for initiation of PET, and number of patients with and without CMV reactivation. OM and/or NRM are reported as risk ratio (RR) or hazard ratio (HR) with 95% confidence intervals (CIs).
Quality assessment
At least two independent investigators applied the Quality In Prognosis Studies (QUIPS) tool to assess the risk of bias in the primary studies. Discrepancies were discussed with another investigator and resolved by discussion. The following 6 domains were included: study participation, study attrition, prognostic factor measurements, outcome measurements, study confounding and statistical analysis, and reporting. The Risk of Bias in Systematic Reviews and the Assessment of Multiple Systematic Reviews (AMSTAR) 2 tool were used to evaluate the risk of bias and quality of included articles.
Data synthesis and analysis
The frequency or percentage descriptive statistics was used to analyze the data in this study. Excel was utilized to show the methodological quality results of included studies. A summary of interest outcomes was tabulated based on the different outcome measures.
Results
Results of study selection
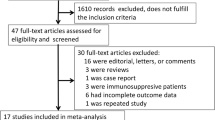
A total of 429 relevant reports were retrieved for SRs, with 3 SRs [12,13,14] included after the screening. Furthermore, a total of 2983 relevant reports were retrieved for clinical primary studies, and 22 clinical studies [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] were ultimately included after screening (Fig. 1a and b).
Baseline characteristics
The baseline characteristics of the included SRs are presented in Table 1. The 3 SRs were published between 2014 and 2021 (from China, Spanish, and Thailand, respectively), with sample sizes ranging from 7642 to 36,665 cases and which reported the outcomes of OM, NRM, IFD, and disease relapse after allo-HSCT. The baseline characteristics of the included clinical studies are presented in Table 2. The 22 included studies were published between 2005 and 2022 (8 from Asia, 13 from Western countries, and one not available), with sample sizes ranging from 30 to 1825 cases. There were 2 case–control studies and 20 cohort studies that reported the outcomes of renal dysfunction, poor graft function, re-hospitalization, and bacterial infections.
The results of the quality of the included studies
Results of the AMSTAR 2 assessment are shown in Online Resource 2. For each AMSTAR 2 item, among the 16 items, nine items were rated as “Yes” (items 1, 3, 5, 6, 11, 13, 14, 15, and 16) for Giménez 2019 [13], nine items were rated as “Yes” (items 1, 3, 5, 9, 11, 13, 14, 15, and 16) for Chuleerarux 2021 [14], eight items were rated as “Yes” (items 1, 5, 6, 9, 11, 14, 15, and 16) for Zhang 2019 [12]. In addition, included primary clinical studies whose overall risk bias was all assessed with “Moderate” are shown in Online Resource 3.
Primary outcome
All-cause mortality
One SR [13] included 16 studies comprising 10,097 patients published in 2019 reported the outcomes of all-cause mortality and showed that CMV reactivation was associated with an increased risk of OM (HR 1.46; 95% CI, 1.24–1.72; P ≤ 0.001) (Table 3, Fig. 2).
Secondary outcome
Non-relapse mortality (NRM)
Two SRs reported the outcomes of non-relapse mortality. One study [13] included 11 studies comprising 8618 patients published in 2019 and reported that CMV reactivation was associated with NRM (HR 1.41; 95% CI, 1.08–1.83; P = 0.01). Another study [12] included three studies consisting of 13,274 patients published in 2019 and reported that CMV replication was an independent risk factor for increased non-relapse mortality for AML (HR 1.64; 95% CI, 1.46–1.85; P < 0.001) and ALL (HR 1.92; 95% CI, 1.57–2.34; P < 0.001) (Table 3, Fig. 2).
Hematologic disease relapse
One SR [12] included 21 studies that reported the outcome of hematologic disease relapse. The meta-analysis published in 2019 included 36,665 patients and reported there might be a significant correlation between disease relapse and CMV replication (HR 0.74; 95% CI, 0.63–0.87; P < 0.001). And there was a significant protection against relapse observed in the AML patients (HR 0.64; 95% CI, 0.50–0.83; P < 0.001) (Table 3, Fig. 2).
Graft-versus-host disease (GVHD)
One SR [12] included 5 studies with 11,745 patients and evaluated the relationship between CMV reactivation and GVHD. There was no association between CMV replication and GVHD for AML-aGVHD (HR 0.87 (0.55–1.39; P = 0.564), AML-cGVHD (HR 0.88 (0.38–2.03); P = 0.758), and ALL-aGVHD (HR 1.24 (0.98–1.57); P = 0.078) (Table 3, Fig. 2).
Invasive fungal disease (IFD)
One SR [14] published in 2021 included 12 studies with 7642 patients and evaluated the relationship between CMV reactivation and IFD. CMV reactivation significantly increased the risk of IFD (HR 2.575; 95% CI, 1.775–3.737; P < 0.001) (Table 3, Fig. 2).
Renal dysfunction, poor graft function, re-hospitalization, and bacterial infections
Three studies [18, 23, 33] included 815 patients and support that CMV reactivation increases the risk of renal dysfunction in patients after allo-HSCT (Table 4, Fig. 3). Seven studies [21, 22, 24, 25, 31, 32, 35] support that CMV reactivation increases the risk of poor graft function, while two studies [16, 19] showed no association between CMV reactivation and poor graft function (Table 4, Fig. 3). Three studies [17, 29, 33] support that CMV reactivation increases the risk of re-hospitalization, but two studies [25, 36] found no association between CMV reactivation and re-hospitalization (Table 4, Fig. 3). Four of six studies [15, 20, 27, 28, 30, 34] support that CMV reactivation increases the risk of bacterial infections (Table 4, Fig. 3).
Discussion
The effect of CMV reactivation post-allo-HSCT, especially the indirect effect, is multifaceted, and the related studies are intricate. This is the first evidence mapping study in this field that provides a more comprehensive assessment of the progress made and the current status of the field. The results suggest that CMV reactivation is associated with an increased risk of OM and NRM for patients after allo-HSCT. Furthermore, CMV reactivation might be associated with an increased risk of IFD, renal dysfunction, poor graft function, bacterial infections, and re-hospitalization. Finally, CMV reactivation might be protective against hematologic disease relapse.
CMV reactivation is one of the most common causes of morbidity and mortality following allo-HSCT and occurs primarily within the first 100 days post-transplantation. Despite advances in the diagnosis and prevention of CMV reactivation, previous studies have reported a significantly lower median survival rate and increased overall mortality in patients with reactivation following transplantation [37,38,39,40]. One SR included 17 studies comprising 10,221 patients showed CMV reactivation was significantly associated with an increased risk of OM. Furthermore, the use of preemptive antiviral therapy led to a twofold increase risk in the risk of OM [13]. Thus, based on the available evidence, CMV reactivation is associated with an increased risk of OM. Most studies found a significant correlation between CMV reactivation after transplantation and an increase in NRM [41, 42]. Two SRs included in the systematic review provided sufficient data to support that CMV reactivation was significantly associated with an increased risk of NRM [12, 13].
Several recent studies have reported that CMV reactivation following allo-HCT reduced the risk of early relapse in patients with AML but was not associated with a reduced risk in patients with other diseases [42]. Results, however, have been inconsistent. One study from the Center for International Blood and Marrow Transplant Research (CIBMTR) Database showed that CMV reactivation after allo-HCT was not associated with relapse in patients with AML [3]. Furthermore, the results from European Conference on Infections in Leukemia (ECIL) [43] and American Society of Transplantation and Cellular Therapy (ASTCT)[44] also found no association between CMV reactivation and relapse in patients after allo-HCT. The SR published in 2019 showed a significantly lower relapse risk after allo-HSCT in patients with AML and CMV replication [12]. The above studies suggest that the correlation between CMV reactivation and tumor recurrence is still highly controversial. Furthermore, the mechanisms underlying the reduction in the rate of relapse are unclear. Repeated environmental influences such as CMV have profound effects on immune homeostasis and the immune system in general, especially on T cells that are involved in anti-tumor immunity [45]. One recent study reported that aside from CMV-CTL reconstitution, CMV reactivation could affect WT1-specific CD8 + T cell reconstitution following allo-HSCT, potentially contributing to the remission or relapse of AML. Moreover, although CMV-CTL reconstitution may be beneficial in reducing CMV activation, it may be detrimental to immune reconstitution. CMV-CTL reconstitution is often accompanied by a reduction in naive T cells and a stronger immune response, both of which also reflect the possible correlation between CMV and GVHD and the increased risk of subsequent opportunistic infections [46]. Patients with both aGVHD and CMV reactivation had significantly higher NRM and poorer OS [10, 47]. Because infections with CMV and GVHD are the most common complications and account for most of the deaths following allo-HSCT, it is necessary to clarify the relationship between GVHD and CMV reactivation after allo-HSCT. Although the SR showed no association between CMV replication and GVHD [12], one study consisting of 515 patients who underwent allo-HSCT between 1993 and 2008 showed that during phases of CMV replication, patients were at increased risk of developing acute GVHD [48].
IFD is another important infectious complication that cannot be ignored. IFD may be caused by CMV reactivation or side effects of antiviral drugs. Although several previous studies demonstrated that CMV reactivation was a risk factor for IFD, other studies reported conflicting results [5, 49,50,51]. Other factors that must be considered are transplant-related factors, use of corticosteroids, neutropenia induced by anti-CMV drugs such as ganciclovir, and/or the adverse effects on host immunity by CMV itself [51]. Additionally, most studies included in the evidence mapping research support that CMV reactivation is associated with an increased risk of renal dysfunction, poor graft function, and bacterial infections in allo-HSCT recipients. Foscarnet, which is used to treat ganciclovir-resistant CMV infections, is efficacious but also associated with nephrotoxicity, with rates as high as 60% during therapy due primarily to acute tubulointerstitial nephritis, which can lead to renal dysfunction [52]. Furthermore, side effects of drugs given for complications of CMV, for example, aminoglycosides given for neutropenic fever due to poor graft function, can lead to severely reduced kidney function [53]. Poor graft function is a life-threatening complication following allo-HSCT. Prabahran and his colleagues [25] demonstrated that CMV viremia [OR 2.43; 95% CI, 1.53–3.88; P < 0.001] was significantly associated with the development of poor graft function. CMV infection in patients following allo-HSCT has been shown to decrease the expression of bone stroma secretion factors and lead to poor graft function [54]. Other reasons for poor graft function included the use of ganciclovir, number of infused CD34 + cells, presence of HLA antibodies, and GVHD [55].
Infection is one of the most common complications in patients with allo-HSCT, with the most common infection being bacteremia, especially gram-negative bacteremia [56]. Approximately one-fifth of patients post-HSCT develop bacteremia concurrently with CMV reactivation [57]. While risk factors for bacterial infection vary, levofloxacin prophylaxis in HSCT recipients is associated with the emergence of fluoroquinolone-resistant gram-negative bacteria [58]. Recently, valganciclovir and ganciclovir have been successfully used for the prevention and treatment of CMV reactivation, although it is associated with serious side effects such as leukopenia, which can lead to bacterial infections [59]. One randomized controlled trial of 565 patients who received either letermovir or placebo from 2014 to 2016 found that prophylactic letermovir treatment significantly reduced the risk of clinically significant CMV reactivation compared to placebo [60]. A previous study demonstrated through week 24 post-transplantation, all-cause mortality rate was 15.0% in the letermovir group versus 18.2% in the placebo group; with rates of 26.5% and 40.9%, respectively, through week 48 [61].
Conclusion
The impact of CMV reactivation post-allo-HSCT is substantial and is associated with an increased risk of OM, NRM, IFD, hematologic disease relapse, renal dysfunction, re-hospitalization, poor graft function, and bacterial infections. A proactive and adequate course of therapy to prevent CMV is necessary. Further attention needs to be paid to the value of using letermovir for CMV prophylaxis and to improving the prognosis of patients with CMV reactivation post-allo-HSCT in the future.
Data availability
The original contributions presented in this study are included in the article/Online Resource material. Further inquiries can be directed to the corresponding author.
References
Ljungman P et al (2019) Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis 19(8):e260–e272
Green ML et al (2016) Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol 3(3):e119–e127
Teira P et al (2016) Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood 127(20):2427–2438
Liu YC et al (2012) Cytomegalovirus infection and disease after allogeneic hematopoietic stem cell transplantation: experience in a center with a high seroprevalence of both CMV and hepatitis B virus. Ann Hematol 91(4):587–595
Yong MK, Slavin MA, Kontoyiannis DP (2018) Invasive fungal disease and cytomegalovirus infection: is there an association? Curr Opin Infect Dis 31(6):481–489
Manjappa S et al (2014) Protective effect of cytomegalovirus reactivation on relapse after allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients is influenced by conditioning regimen. Biol Blood Marrow Transplant 20(1):46–52
Nakamura R et al (2004) Persisting posttransplantation cytomegalovirus antigenemia correlates with poor lymphocyte proliferation to cytomegalovirus antigen and predicts for increased late relapse and treatment failure. Biol Blood Marrow Transplant 10(1):49–57
Elmaagacli AH et al (2011) Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood 118(5):1402–1412
Jerry Teng CL et al (2021) Cytomegalovirus management after allogeneic hematopoietic stem cell transplantation: a mini-review. J Microbiol Immunol Infect 54(3):341–348
Jang JE et al (2015) Early CMV replication and subsequent chronic GVHD have a significant anti-leukemic effect after allogeneic HSCT in acute myeloid leukemia. Ann Hematol 94(2):275–282
Ito S et al (2013) CMV reactivation is associated with a lower incidence of relapse after allo-SCT for CML. Bone Marrow Transplant 48(10):1313–1316
Zhang YL et al (2019) Cytomegalovirus infection is associated with AML relapse after allo-HSCT: a meta-analysis of observational studies. Ann Hematol 98(4):1009–1020
Gimenez E et al (2019) Cytomegalovirus (CMV) infection and risk of mortality in allogeneic hematopoietic stem cell transplantation (Allo-HSCT): a systematic review, meta-analysis, and meta-regression analysis. Am J Transplant 19(9):2479–2494
Chuleerarux N et al (2022) The association of cytomegalovirus infection and cytomegalovirus serostatus with invasive fungal infections in allogeneic haematopoietic stem cell transplant recipients: a systematic review and meta-analysis. Clin Microbiol Infect 28(3):332–344
Beswick J et al (2018) Incidence and risk factors for nontuberculous mycobacterial infection after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 24(2):366–372
Chen J et al (2022) Primary graft failure following allogeneic hematopoietic stem cell transplantation: risk factors, treatment and outcomes. Hematology 27(1):293–299
De Miguel C et al (2018) Clinical impact and burden of CMV infection on the use of resources in allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 24(3):S388
Deconinck E et al (2005) Cytomegalovirus infection and chronic graft-versus-host disease are significant predictors of renal failure after allogeneic hematopoietic stem cell transplantation. Haematologica 90(4):569–570
Hama A et al (2020) Risk factors for secondary poor graft function after bone marrow transplantation in children with acquired aplastic anemia. Pediatr Transplant 24(7):e13828
Lavallée C et al (2017) Risk factors for the development of Clostridium difficile infection in adult allogeneic hematopoietic stem cell transplant recipients: a single-center study in Québec, Canada. Transplant Infect Dis Off J Transplant Soc 19(1)
Lin F et al (2022) The incidence, outcomes, and risk factors of secondary poor graft function in haploidentical hematopoietic stem cell transplantation for acquired aplastic anemia. Front Immunol 13
Lv WR et al (2021) Haploidentical donor transplant is associated with secondary poor graft function after allogeneic stem cell transplantation: a single-center retrospective study. Cancer Med 10(23):8497–8506
Madsen K et al (2020) Incidence, outcomes and predictors of acute kidney injury post allogeneic stem cell transplant. Blood. 136((Madsen K.; Chen S.; Pasic I.) Hans Messner Allogeneic Transplant Program, Division of Medical Oncology and Haematology, Princess Margaret Cancer Centre, University Health Network, Toronto, Canada): p. 16–17.
Masouridi Levrat S et al (2016) Impact of different methods of T-cell depletion on poor graft function incidence after allogeneic hematopoietic stem cell transplantation. Bone marrow transplantation. 51((Masouridi Levrat S.; Simonetta F.; Tirefort Y.; Tsopra O.; Dantin C.; Beauverd Y.; Simon A.; Polchlopeck K.; Stephan C.; Chalandon Y.) Hematology, Geneva University Hospitals, Geneva, Switzerland): p. S429-S430.
Prabahran A et al (2021) Evaluation of risk factors for and subsequent mortality from poor graft function (PGF) post allogeneic stem cell transplantation. Leuk Lymphoma 62(6):1482–1489
Prabahran AA et al (2021) Recurrent CMV viremia portends poor prognosis and results in significant resource utilization in patients with poor graft function post allogeneic stem cell transplantation. Blood 138((Prabahran A.A.; Chee L.C.Y.; Koldej R.M.; Ritchie D.) ACRF Translational Research Laboratory, The Royal Melbourne Hospital, Parkville, Australia): p. 4854.
Sano H et al (2017) African American race is a newly identified risk factor for postengraftment blood stream infections in pediatric allogeneic blood and marrow transplantation. Biol Blood Marrow Transplant 23(2):357–360
Saullo JL et al (2020) Cytomegalovirus in allogeneic hematopoietic transplantation: impact on costs and clinical outcomes using a preemptive strategy. Biol Blood Marrow Transplant 26(3):568–580
Schelfhout J et al (2020) Impact of cytomegalovirus complications on resource utilization and costs following hematopoietic stem cell transplant. Curr Med Res Opin 36(1):33–41
Skert C et al (2014) A specific Toll-like receptor profile on T lymphocytes and values of monocytes correlate with bacterial, fungal, and cytomegalovirus infections in the early period of allogeneic stem cell transplantation. Transpl Infect Dis 16(5):697–712
Sun Y, Huang XJ (2019) Virus reactivation and low dose of CD34+ cell were associatied with secondary poor graft function within the first 100 days after allogeneic stem cell transplantation. Bone marrow transplantation, 54((Sun Y.; Huang X.-J.) Peking University People's Hospital, Peking University Institute of Hematology, Beijing Key Laboratory of Hematopoietic Stem Cell Transplantation, Beijing, China): p. 265–266.
Sun YQ et al (2019) Virus reactivation and low dose of CD34+ cell, rather than haploidentical transplantation, were associated with secondary poor graft function within the first 100 days after allogeneic stem cell transplantation. Ann Hematol 98(8):1877–1883
Teschner D et al (2022) Cytomegalovirus infection and rehospitalization rates after allogeneic hematopoietic stem cell and solid organ transplantation: a retrospective cohort study using German claims data. Infection 50(6):1543–1555
Vinuesa V et al (2016) Lack of evidence for a reciprocal interaction between bacterial and cytomegalovirus infection in the allogeneic stem cell transplantation setting. Transplant Int Off J Eur Soc Organ Transplant 29(11):1196–1204
Xiao Y et al (2014) Risk-factor analysis of poor graft function after allogeneic hematopoietic stem cell transplantation. Int J Med Sci 11(6):652–657
Yamagishi Y et al (2019) Risk factors and survival impact of readmission after single-unit cord blood transplantation for adults. Int J Hematol 109(1):115–124
Sousa H et al (2014) Cytomegalovirus infection in patients who underwent allogeneic hematopoietic stem cell transplantation in Portugal: a five-year retrospective review. Biol Blood Marrow Transplant 20(12):1958–1967
Takenaka K et al (2015) Cytomegalovirus reactivation after allogeneic hematopoietic stem cell transplantation is associated with a reduced risk of relapse in patients with acute myeloid leukemia who survived to day 100 after transplantation: the Japan Society for Hematopoietic Cell Transplantation Transplantation-related Complication Working Group. Biol Blood Marrow Transplant 21(11):2008–2016
Haidar G, Boeckh M, Singh N (2020) Cytomegalovirus infection in solid organ and hematopoietic cell transplantation: state of the evidence. J Infect Dis 221(Suppl 1):S23-s31
Eberhardt KA et al (2023) CMV-IgG pre-allogeneic hematopoietic stem cell transplantation and the risk for CMV reactivation and mortality. Bone Marrow Transplant
Elmaagacli AH, Koldehoff M (2016) Cytomegalovirus replication reduces the relapse incidence in patients with acute myeloid leukemia. Blood 128(3):456–459
Green ML et al (2013) CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood 122(7):1316–1324
Maschmeyer G et al (2022) Infectious complications of targeted drugs and biotherapies in acute leukemia. Clinical practice guidelines by the European Conference on Infections in Leukemia (ECIL), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organization for Research and Treatment of Cancer (EORTC), the International Immunocompromised Host Society (ICHS) and the European Leukemia Net (ELN). Leukemia 36(5):1215–1226
Yong MK et al (2021) American Society for Transplantation and Cellular Therapy Series: #4 - Cytomegalovirus treatment and management of resistant or refractory infections after hematopoietic cell transplantation. Transplant Cell Ther 27(12):957–967
Luo XH et al (2018) The impact of inflationary cytomegalovirus-specific memory T cells on anti-tumour immune responses in patients with cancer. Immunology 155(3):294–308
Luo XH et al (2022) Different recovery patterns of CMV-specific and WT1-specific T cells in patients with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation: Impact of CMV infection and leukemia relapse. Front Immunol 13:1027593
Fan ZY et al (2022) CMV infection combined with acute GVHD associated with poor CD8+ T-cell immune reconstitution and poor prognosis post-HLA-matched allo-HSCT. Clin Exp Immunol 208(3):332–339
Cantoni N et al (2010) Evidence for a bidirectional relationship between cytomegalovirus replication and acute graft-versus-host disease. Biol Blood Marrow Transplant 16(9):1309–1314
Shi JM et al (2015) Invasive fungal infection in allogeneic hematopoietic stem cell transplant recipients: single center experiences of 12 years. J Zhejiang Univ Sci B 16(9):796–804
Atalla A et al (2015) Risk factors for invasive mold diseases in allogeneic hematopoietic cell transplant recipients. Transpl Infect Dis 17(1):7–13
Yong MK et al (2017) Cytomegalovirus reactivation is associated with increased risk of late-onset invasive fungal disease after allogeneic hematopoietic stem cell transplantation: a multicenter study in the current era of viral load monitoring. Biol Blood Marrow Transplant 23(11):1961–1967
Pierce B et al (2018) Safety and efficacy of foscarnet for the management of ganciclovir-resistant or refractory cytomegalovirus infections: a single-center study. Transpl Infect Dis 20(2):e12852
Halouzková BA et al (2022) Dosing of aminoglycosides in chronic kidney disease and end-stage renal disease patients treated with intermittent hemodialysis. Kidney Blood Press Res 47(7):448–458
Zaucha-Prazmo A et al (2005) Cytomegalovirus (CMV) infections in children undergoing hematopoetic stem cell transplantation. Pediatr Hematol Oncol 22(4):271–276
Kong Y (2019) Poor graft function after allogeneic hematopoietic stem cell transplantation-an old complication with new insights(☆). Semin Hematol 56(3):215–220
Girmenia C et al (2017) Incidence, risk factors and outcome of pre-engraftment gram-negative bacteremia after allogeneic and autologous hematopoietic stem cell transplantation: an Italian prospective multicenter survey. Clin Infect Dis 65(11):1884–1896
Öksüz L et al (2022) The association of CMV infection with bacterial and fungal infections in hematopoietic stem cell transplant recipients: a retrospective single-center study. New Microbiol 45(1):40–50
Wang CH et al (2018) Characteristics comparisons of bacteremia in allogeneic and autologous hematopoietic stem cell-transplant recipients with levofloxacin prophylaxis and influence on resistant bacteria emergence. J Microbiol Immunol Infect 51(1):123–131
Khawaja F et al (2023) Cytomegalovirus infection in transplant recipients: newly approved additions to our armamentarium. Clin Microbiol Infect 29(1):44–50
Marty FM et al (2017) Letermovir Prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med 377(25):2433–2444
Marty FM et al (2020) Outcomes of patients with detectable CMV DNA at randomization in the phase III trial of letermovir for the prevention of CMV infection in allogeneic hematopoietic cell transplantation. Am J Transplant 20(6):1703–1711
Acknowledgements
The collection and assembly of data and statistical expertise were provided by Sai Zhao, Yang Zhang, and Zhaoyuan Liu from Systematic Review Solutions, Ltd.
Funding
This study was funded by MSD China.
Author information
Authors and Affiliations
Contributions
Xiaojin Wu, Depei Wu, Jie Liu and Xiao Ma proposed the research idea. Tiemei Song, Jie Liu, and Yi Sun acquired and analyzed the data and wrote the paper. All authors revised the manuscript and approved all versions including the final version. All authors were responsible for the accuracy and integrity of all aspects of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
All authors have read and approved the final submitted manuscript and agree to be accountable for the work.
Conflict of interest
Although Jie Liu and Yi Sun were employees of MSD China, all of the authors declare there are no conflicts of interest related to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
1. The impact of cytomegalovirus (CMV) reactivation on the risk of overall mortality (OM) and non-relapse mortality (NRM) in patients following allogeneic hematopoietic stem cell transplantation (allo-HSCT) is still controversial.
2. This is the first evidence mapping study in this field that provides a more comprehensive assessment of the progress made and the current status of the evidence.
3. The study concluded that CMV reactivation following allo-HSCT is associated with an increased risk of OM, NRM, invasive fungal disease (IFD), and renal dysfunction.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, X., Ma, X., Song, T. et al. The indirect effects of CMV reactivation on patients following allogeneic hematopoietic stem cell transplantation: an evidence mapping. Ann Hematol 103, 917–933 (2024). https://doi.org/10.1007/s00277-023-05509-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05509-7