Abstract
Autologous stem cell transplantation (ASCT) is the standard therapy for patients with transplant-eligible multiple myeloma (TEMM). However, the ideal depth of response required before ASCT and the impact of residual tumor cells in the stem cell collection (SCC) on survival remains unclear. Here we collected data of 89 patients with TEMM undergoing ASCT and analyzed the minimal residual disease of SCC (cMRD) and bone marrow (BM) (mMRD) before transplantation. Before ASCT, 31.5% and 76.4% of patients achieved MRD negativity in BM and SCC, respectively. Tumor cells were less in SCC samples than that in BM samples. Neoplastic cells in SCC could be observed in patients with different responses after induction therapy, and there were no significant differences in the percentage and level of cMRD among these subgroups (P > 0.05). No correlation was found between the cMRD status and the response patients achieved after ASCT (P > 0.05). The median follow-up was 26.8 months. mMRD negativity before ASCT was associated with longer PFS (55.9 vs. 27.1 months; P = 0.009) but not OS (not reached vs. 58.9 months; P = 0.115). Patients with different cMRD statuses before ASCT experienced similar PFS (40.5 vs. 76.4 months for negativity vs. positivity; P = 0.685) and OS (not reached vs. 58.8 months for negativity vs. positivity; P = 0.889). These results suggested that detectable cMRD does not significantly predict the inferior post-ASCT response or shorter survival, and patients are eligible to undergo ASCT upon achieving partial response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is the second most common hematological malignancy associated with monoclonal plasma cells (PCs). In recent years, novel treatment options for MM have become widely available, leading to substantial improvement in response and prognosis [1]. The IFM 2013-04 trial [2] was the first to verify the significant and synergistic activity of a proteasome inhibitor (PI) combined with an immunomodulatory drug (IMiD), and the prospective randomized phase 3 trial SWOG S0777 [3] has demonstrated the superior efficacy and survival benefit of the VRd regimen (bortezomib, lenalidomide, and dexamethasone), and the combination regimen has been incorporated into front-line induction therapy for MM [4, 5]. Although these novel drugs have the potential to significantly improve patient survival, several studies have highlighted the irreplaceable role of autologous stem cell transplantation (ASCT) in transplant-eligible patients with MM (TEMM) [6, 7].
Most clinical guidelines recommend ASCT for patients who have achieved partial response (PR), and previous studies [8, 9] also revealed that prolonging the induction therapy duration or additional pre-ASCT salvage chemotherapy could deepen the depth of the pre-ASCT response but it was not associated with survival benefits. However, whether it would result in the presence of tumor cells within the stem cell collection (SCC) in patients failing to achieve complete response (CR) and its impact on patient outcome remain to be elucidated. Some studies have focused on the prognostic value of the MRD of SCC (cMRD) prior to the transplantation, but no consensus has been reached [10, 11].
In this study, we aimed to evaluate the effect of minimal residual disease (MRD) in patients with TEMM by comparing the number of tumor cells in SCC and bone marrow (BM) samples obtained before ASCT. We also aimed to investigate the effect of MRD in SCC samples on treatment responses and survival.
Materials and methods
Patients
We analyzed the clinical data of 89 patients with MM who underwent ASCT at our hospital between January 1, 2013, and June 1, 2021. All patients were included in a prospective, non-randomized clinical trial (BDH 2008/02), and the treatment regimen has been described in previous studies [12, 13].
The enrolled patients in our data all received PIs-based induction therapy. After attaining PR at minimum after at least four cycles, patients underwent ASCT followed by maintenance. All patients underwent melphalan treatment after induction with granulocyte colony-stimulating factor (G-CSF) administered for mobilization. Plerixafor was used in cases of suboptimal mobilization and collection. The minimum CD34+ stem cell dose for collection was 2 × 106 CD34+ cells/kg, and the optimal target was 4 × 106 CD34+ cells/kg. Responses were assessed in accordance with International Myeloma Working Group (IMWG) criteria [14]. In our study, the best response was defined as the deepest response during follow-up. Time from ASCT to disease progression was defined as progression-free survival (PFS) and time from ASCT to death as overall survival (OS).
Fluorescence in situ hybridization and flow cytometry analysis
CD138+ PC enrichment and fluorescence in situ hybridization (FISH) analyses were performed as previously described [15]. The routine panel included evaluations for 13q14 deletion, 17p deletion, 1q21 gain/amplification, t(11;14), t(4;14), t(14;16), and t(14;20). Positive cutoff levels were defined as 10% for translocation and 20% for numerical abnormalities [16]. High-risk cytogenetic abnormalities (CAs) were defined as the presence of del(17p), t(4;14), or t(14;16) [17]. MRD was evaluated via multiparameter flow cytometry with a sensitivity of 1 × 10−5 using two combinations of 8-color monoclonal antibodies as previously described [18].
Statistical analysis
Two-sided chi-square tests and Fisher’s exact tests were used to assess differences between categorical variables. Wilcoxon tests and Mann–Whitney U tests were used to assess differences between continuous variables. Survival outcomes were analyzed using the Kaplan–Meier method and compared using the log-rank test. The Cox proportional hazard model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). Statistical analyses were performed using SPSS version 26 (IBM, Armonk, NY, USA) and R Studio version 4.1.2. P < 0.05 was considered statistically significant. For significant values in univariate analysis (P < 0.10), the Cox proportional hazards model was used to identify independent predictive factors.
Results
Patient characteristics
A total of 89 patients were included in the analysis. The baseline characteristics are presented in Supplementary Table S1. The median age of the patients was 54 years (range, 37–69 years), and 62.9% were male. FISH identified high-risk CAs in 24 patients (27.0%). Before ASCT, the percentages of patients with mMRD− and cMRD− were 31.5% and 76.4%, respectively. The baseline characteristics of patients with different MRD statuses in SCC and BM were similar (Table 1).
Tumor cells in the SCC and BM
Regardless of the sensitivity used for cMRD evaluation, the percentage of patients with MRD positivity in the BM was much higher than that with positivity in the SCC (69.6% vs. 24.4% for the sensitivity of 10−6, 68.5% vs. 23.3% for the sensitivity of 10−5, and 57.3% vs. 12.2% for the sensitivity of 10−4; P < 0.001; Supplementary Table S2). As for the numeric level of tumor cells in BM and SCC samples, the distribution of the detectable monoclonal PCs was 48.4% vs. 77.3% for the 101–102 level and 51.6% vs. 22.7% for the 103–105 level (P = 0.019; Supplementary Table S2).
Plerixafor, a CXC chemokine receptor 4 (CXCR4) antagonist, is widely used in clinical practice as a stem cell-mobilizing agent. CXCR4 is expressed not only on BM progenitor cells but also on various types of tumor cells [19, 20]. Supplementary Table S3 shows a comparison of cMRD status according to plerixafor use. Plerixafor was used during the mobilization of hematopoietic stem cells in 33 patients. Notably, the frequency of residual clonal PCs in SCC was similar between the plerixafor and non-plerixafor groups (24.2% vs. 23.2%; P = 0.912), and there was no significant difference in the median level of cMRD (0.008% with plerixafor and 0.01% without plerixafor; P = 0.920).
Correlation between response and cMRD
The response of patients at stem cell collecting and after transplantation is shown in Table 2. Although the percentages of patients achieving at least very good PR (≥VGPR, 76.1% vs. 52.4%; P = 0.037) and CR (≥CR, 49.2% vs. 23.8%; P = 0.040) were higher among patients with cMRD− than those among patients with cMRD+ before collection, the rates of deep response after ASCT were similar between the cMRD+ and cMRD− groups (P > 0.1; Table 2), which was in contrast with the findings observed for patients with different mMRD statuses.
Residual tumor cells were observed in the SCC in 20.5% and 25.0% of patients who attained CR/sCR or VGPR after induction therapy, respectively. Although a higher percentage (38.5%) of cMRD+ was observed in patients with PR before ASCT, there were no significant differences among the three subgroups (P = 0.126; Fig. 1A). Similarly, we observed no significant differences in the level of cMRD among patients with PR, VGPR, and CR/sCR (P = 0.568; Fig. 1B). Because of the relatively higher percentage of cMRD+ in patients achieving PR, we then analyzed post-ASCT response of these patients. Approximately 29.9% (26/87) of the enrolled patients achieved PR after induction therapy, with 10 and 16 patients exhibiting cMRD+ and cMRD−, respectively, and both groups achieved similar deep response rate for post-ASCT response (40% vs. 43.7% for VGPR or better, 10% vs. 12.5% for CR or better) and the best response during the follow-up (60% vs. 66.6% for VGPR or better; 30% vs. 20% for CR or better, Supplementary Table S4).
Presence (A) and level (B) of clonal plasma cells according to the response after induction therapy. MRD, minimal residual disease; SCC, stem cell collection; cMRD, minimal residual disease in stem cell collection; CR, complete response; sCR, stringent complete response; VGPR, very good partial response; PR, partial response
Prognostic value of post-induction and post-ASCT responses
The median duration of follow-up was 26.8 months (15.1–105.1 months). Supplementary Figure S1 shows the results of the survival analysis for patients with different responses before and after ASCT. Pre-ASCT response lacked a survival benefit for PFS (P = 0.195; Supplementary Figure S1A) and OS (P = 0.168; Supplementary Figure S1B). In contrast, post-ASCT response was identified as a significant predictor of survival. Better responses were associated with increase in both PFS (not reached vs. 42.6 vs. 27.1 vs. 30.1 for sCR vs. CR vs. VGPR vs. PR; P = 0.011; Supplementary Figure S1C) and OS (not reached vs. not reached vs. 58.6 vs. 41.6 for sCR vs. CR vs. VGPR vs. PR; P = 0.007; Supplementary Figure S1D). Similar results were obtained for best response and mMRD status during follow-up (Fig. 2), with median PFS of 27.2 months among patients with VGPR or less, 24.7 months among patients with mMRD+ CR, and 55.9 months among patients with mMRD− CR (P < 0.001; Fig. 2A). The median OS was 41.6 months in the VGPR or less group and not reached in the other two CR subgroups (P = 0.006; Fig. 2B).
Survival curves according to the best response and MRD status after ASCT in all patients. PFS (A) and OS (B) in patients achieving ≤VGPR, MRD+ CR, and MRD− CR. MRD, minimal residual disease; ASCT, autologous stem cell transplantation; PFS, progression-free survival; OS, overall survival; VGPR, very good partial response; CR, complete response
Prognostic value of cMRD and mMRD
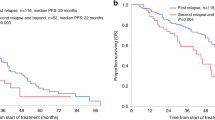
Negative mMRD before ASCT was associated with longer PFS (55.9 vs. 27.1 months; P = 0.009; Fig. 3A); however, no significant difference was observed in the OS according to pre-ASCT mMRD status (not reached vs. 58.9 months for mMRD− vs. mMRD+; P = 0.115; Fig. 3B). Median PFS (40.5 vs. 76.4 months for cMRD− vs. cMRD+; P = 0.685; Fig. 3C) and OS (not reached vs. 58.8 months for cMRD− vs. cMRD+; P = 0.889; Fig. 3D) did not significantly differ according to cMRD status before ASCT.
Kaplan–Meier survival analysis for patients with multiple myeloma according to MRD status in the BM (A, B) and SCC (C, D) before ASCT. MRD, minimal residual disease; SCC, stem cell collection; BM, bone marrow; cMRD, minimal residual disease in stem cell collection; mMRD, minimal residual disease in the bone marrow; ASCT, autologous stem cell transplantation
Multivariate Cox regression analysis was performed to examine associations among the variables sex, International Staging System (ISS) stage, cytogenetic risk, lactate dehydrogenase (LDH), mMRD, cMRD, response at day 100 after ASCT, and best response during follow-up. None of these factors demonstrated independent significance for OS (P ≥ 0.05). LDH level and the best response during follow-up remained significant prognostic factors for PFS. However, pre-ASCT cMRD exerted no influence on patient outcomes (Table 3).
Discussion
As a standard of care, ASCT has provided substantial benefit for patients with TEMM, resulting in a deeper response and survival improvement [7, 21, 22]. Sufficient evidence has demonstrated the significant prognostic value of a deep response and mMRD− following ASCT [23, 24]. Although many studies have investigated the clinical value of mMRD for predicting survival, relatively few have focused on cMRD before ASCT. Furthermore, studies evaluating the association between SCC contamination and outcomes have yielded contradictory results [10, 25, 26]. Whether it would lead to the presence of tumor cells in the collection when patients have not achieved CR and whether cMRD+ is associated with an increased risk of progression remains to be elucidated.
In this study, tumor cells were detected in BM in 68.5% of the patients, but only 23.6% of the patients exhibited tumor cells in the SCC, and the presence of latter was not correlated with the baseline characteristics of the cohort. Thereafter, we compared the tumor cells in the SCC and BM according to different sensitivities and numeric levels, which yielded similar results that the tumor cells were less common in the SCC than that in the BM. MM cells are drastically affected by the BM milieu for its dependence on the protection and immunosuppressive effect provided by the tumor microenvironment (TME), which favors tumor cell immune escape and drug resistance, thus promoting disease progression [20]. This may explain why there were more MM cells in the BM than in circulation. We also investigated whether MM cells could be mobilized into the circulation using plerixafor and found that the application of plerixafor did not increase the percentage of MRD-positive collections, while the level of neoplastic plasma cells in the collection in plerixafor group was higher than that in no-plerixafor group. A previous study reported a significant increase in the mobilization of MM cells from the BM to circulation, but the study was only in vivo without clinical data analysis [27]. This phenomenon was explained as a surrogate marker for the disruption of adhesion, and the authors suggested that plerixafor enhanced bortezomib-induced tumor reduction. Based on these results, we conclude that the addition of plerixafor to G-CSF treatment is a safe mobilizing regimen for patients with MM.
Our findings indicated that although patients with cMRD− obtained superior response prior to ASCT, the difference of response between patients with different cMRD statuses was not observed after the transplantation, demonstrating that graft contamination had no impact on ASCT. Besides, the inferior response did not increase the presence or level of tumor cells in the SCC. Patients who achieved PR before ASCT and those with VGPR or better response before ASCT both showed evidence of cMRD positivity. Evaluation of conventional response cannot accurately reflect the level of mMRD accurately even if patients have achieved CR. Therefore, it is highly probable that clonal PCs may still exist in the BM and mobilized into the peripheral blood.
As reported in previous studies [8, 9], our study revealed the same conclusion that the depth of the pre-ASCT response provided less survival benefit than the post-ASCT response. Vij et al. [8] reported that salvage therapy such as those with novel agent combinations and additional pre-ASCT salvage chemotherapy improved the depth of response but was not associated with survival benefits for patients achieving a suboptimal response (less than PR) to initial induction therapy. This is in contrast with the findings for acute leukemia, in which a deep response is necessary before transplantation. In our study, the post-ASCT and best responses were significantly associated with survival. These findings suggested that the post-ASCT response was a more important indicator of survival than the pre-ASCT response, which is consistent with other studies demonstrating the clinical value of a superior response after ASCT [23, 28].
The MRD, a new criterion for assessing treatment response introduced by the IMWG in 2016 [14], has been a hot topic for a few years. Undetectable MRD in the BM, especially sustained MRD negativity, is considered a more valuable prognostic marker for longer PFS and OS than CR [23, 29, 30]. Our results also implicated that for patients with post-ASCT CR, undetectable mMRD indicates better survival benefit compared with mMRD positivity. Furthermore, we found that mMRD status before ASCT can be considered a predictor of PFS, consistent with the findings of previous studies in our center. However, the correlation between pre-ASCT mMRD status and OS was not found statistically significant, but there was a stratified trend in survival curves, which may be related to the inclusion of limited data, the relatively short duration of follow-up and great prognosis of patients with ASCT. However, pre-ASCT mMRD negativity was not an independent prognostic factor for PFS in the COX multivariate analysis, which may be related to the short follow-up and positive impact of ASCT on tumor burden in BM [31].
Some studies have focused on the prognostic value of cMRD prior to the transplantation; however, no consensus has been reached. Our study demonstrated that the presence of tumor cells in the SCC had no effect on survival among patients with MM undergoing ASCT. We further verified these results by comparing cMRD status among patients with different responses before and after ASCT. This phenomenon may be related to the inactivation or death of MM cells in the frozen stock solution following apheresis due to their high dependence on the TME. A phase 3 clinical trial [10] in 2001 aimed on purging of autologous peripheral-blood stem cells using CD34 selection demonstrated that CD34 selection could significantly reduce myeloma cell contamination in SCC, but it did not reduce the risk of disease progression. Also, Boccadoro et al. [32] and Ho et al. [25] reported that the relevance was not found between tumor cells in the SCC and survival in their studies. However, some studies have yielded contradictory findings. In 1997, a study revealed that when monoclonal PCs in the blood stem cell harvest increase to 0.2 × 106/L, it could predict a shortened relapse-free survival [33]. However, the number of patients enrolled in this research was only 33, and the patients did not undergo ASCT until progression occurred, also the tumor cells in the BM and the heavy tumor burden may have contributed to the disease progression as well. The study of Wuillème et al. [34] highlighted the impact of neoplastic PCs in the peripheral blood on the day of stem cell collection using flow cytometric detection, revealing that patients in MRD negativity group showed longer PFS and OS. However, the number of patients included in this study was only 75 and more patients with MRD negativity received the tandem transplantation.
Our study has some limitations. First, the limited cohort size may have had some impact on the analysis, and updated data are therefore required to verify our conclusions. Second, for the lack of the related data, there was no comparison between the MRD of collection and the MRD of graft. Last, this was a real-world retrospective study conducted at a single center and there may be selection bias for patients.
Conclusion
Our results provide new insight suggesting that the level of tumor cells in the SCC of patients before transplantation is significantly less than that in the BM, and this study reveals the similar level of tumor cells in SCC for patients with different responses before ASCT. Detectable cMRD (with the sensitivity of 1 × 10−5) does not significantly predict the inferior post-ASCT response or shorter survival, highlighting the feasibility of ASCT in patients who have attained PR.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
van de Donk NWCJ, Pawlyn C, Yong KL (2021) Multiple myeloma. Lancet 397(10272):410–427. https://doi.org/10.1016/s0140-6736(21)00135-5
Moreau P, Hulin C, Macro M, Caillot D, Chaleteix C, Roussel M, Garderet L, Royer B, Brechignac S, Tiab M, Puyade M, Escoffre M, Stoppa AM, Facon T, Pegourie B, Chaoui D, Jaccard A, Slama B, Marit G et al (2016) VTD is superior to VCD prior to intensive therapy in multiple myeloma: results of the prospective IFM2013-04 trial. Blood 127(21):2569–2574. https://doi.org/10.1182/blood-2016-01-693580
Durie BGM, Hoering A, Abidi MH, Rajkumar SV, Epstein J, Kahanic SP, Thakuri M, Reu F, Reynolds CM, Sexton R, Orlowski RZ, Barlogie B, Dispenzieri A (2017) Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet 389(10068):519–527. https://doi.org/10.1016/s0140-6736(16)31594-x
Mikhael J, Ismaila N, Cheung MC, Costello C, Dhodapkar MV, Kumar S, Lacy M, Lipe B, Little RF, Nikonova A, Omel J, Peswani N, Prica A, Raje N, Seth R, Vesole DH, Walker I, Whitley A, Wildes TM, Wong SW, Martin T (2019) Treatment of multiple myeloma: ASCO and CCO Joint Clinical Practice Guideline. J clin oncol 37(14):1228–1263. https://doi.org/10.1200/jco.18.02096
Kumar SK, Callander NS, Adekola K, Anderson L, Baljevic M, Campagnaro E, Castillo JJ, Chandler JC, Costello C, Efebera Y, Faiman M, Garfall A, Godby K, Hillengass J, Holmberg L, Htut M, Huff CA, Kang Y, Hultcrantz M, Larson S, Liedtke M, Martin T, Omel J, Shain K, Sborov D, Stockerl-Goldstein K, Weber D, Keller J, Kumar R (2020) Multiple myeloma, version 3.2021, NCCN Clinical Practice Guidelines in oncology. J natl compr canc netw 18(12):1685–1717. https://doi.org/10.6004/jnccn.2020.0057
Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT, Pezzatti S, Caravita T, Cerrato C, Ribakovsky E, Genuardi M, Cafro A, Marcatti M, Catalano L, Offidani M, Carella AM, Zamagni E, Patriarca F, Musto P, Evangelista A, Ciccone G, Omedé P, Crippa C, Corradini P, Nagler A, Boccadoro M, Cavo M (2014) Autologous transplantation and maintenance therapy in multiple myeloma. N engl j med 371(10):895–905. https://doi.org/10.1056/NEJMoa1402888
Attal M, Lauwers-Cances V, Hulin C, Leleu X, Caillot D, Escoffre M, Arnulf B, Macro M, Belhadj K, Garderet L, Roussel M, Payen C, Mathiot C, Fermand JP, Meuleman N, Rollet S, Maglio ME, Zeytoonjian AA, Weller EA, Munshi N, Anderson KC, Richardson PG, Facon T, Avet-Loiseau H, Harousseau JL, Moreau P (2017) Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N engl j med 376(14):1311–1320. https://doi.org/10.1056/NEJMoa1611750
Vij R, Kumar S, Zhang MJ, Zhong X, Huang J, Dispenzieri A, Abidi MH, Bird JM, Freytes CO, Gale RP, Kindwall-Keller TL, Kyle RA, Landsburg DJ, Lazarus HM, Munker R, Roy V, Sharma M, Vogl DT, Wirk B, Hari PN (2015) Impact of pretransplant therapy and depth of disease response before autologous transplantation for multiple myeloma. Biol blood marrow transplant 21(2):335–341. https://doi.org/10.1016/j.bbmt.2014.10.023
Chakraborty R, Muchtar E, Kumar SK, Buadi FK, Dingli D, Dispenzieri A, Hayman SR, Hogan WJ, Kapoor P, Lacy MQ, Leung N, Warsame R, Kourelis T, Gonsalves W, Gertz MA (2018) Impact of duration of induction therapy on survival in newly diagnosed multiple myeloma patients undergoing upfront autologous stem cell transplantation. Br j haematol 182(1):71–77. https://doi.org/10.1111/bjh.15244
Stewart AK, Vescio R, Schiller G, Ballester O, Noga S, Rugo H, Freytes C, Stadtmauer E, Tarantolo S, Sahebi F, Stiff P, Meharchard J, Schlossman R, Brown R, Tully H, Benyunes M, Jacobs C, Berenson R, White M, DiPersio J, Anderson KC, Berenson J (2001) Purging of autologous peripheral-blood stem cells using CD34 selection does not improve overall or progression-free survival after high-dose chemotherapy for multiple myeloma: results of a multicenter randomized controlled trial. J clin oncol 19(17):3771–3779. https://doi.org/10.1200/jco.2001.19.17.3771
Pasvolsky O, Milton DR, Rauf M, Ghanem S, Masood A, Mohamedi AH, Tanner MR, Bashir Q, Srour S, Saini N, Lin P, Ramdial J, Nieto Y, Tang G, Lee HC, Patel KK, Kebriaei P, Thomas SK, Weber DM, Orlowski RZ, Rezvani K, Champlin R, Shpall EJ, Lin P, Qazilbash MH (2023) Impact of clonal plasma cells in autografts on outcomes in high-risk multiple myeloma patients. Blood cancer j 13(1):68. https://doi.org/10.1038/s41408-023-00842-6
An G, Yan Y, Xu Y, Mao X, Liu J, Fan H, Wang Q, Du C, Li Z, Yi S, Lv R, Deng S, Sui W, Fu M, Hao M, Huang W, Zou D, Zhao Y, Yuan C et al (2020) Monitoring the cytogenetic architecture of minimal residual plasma cells indicates therapy-induced clonal selection in multiple myeloma. Leukemia 34(2):578–588. https://doi.org/10.1038/s41375-019-0590-x
An G, Xu Y, Shi L, Shizhen Z, Deng S, Xie Z, Sui W, Zhan F, Qiu L (2014) Chromosome 1q21 gains confer inferior outcomes in multiple myeloma treated with bortezomib but copy number variation and percentage of plasma cells involved have no additional prognostic value. Haematologica 99(2):353–359. https://doi.org/10.3324/haematol.2013.088211
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, Munshi N, Lonial S, Bladé J, Mateos M-V, Dimopoulos M, Kastritis E, Boccadoro M, Orlowski R, Goldschmidt H, Spencer A, Hou J, Chng WJ, Usmani SZ, Zamagni E, Shimizu K, Jagannath S, Johnsen HE, Terpos E, Reiman A, Kyle RA, Sonneveld P, Richardson PG, McCarthy P, Ludwig H, Chen W, Cavo M, Harousseau J-L, Lentzsch S, Hillengass J, Palumbo A, Orfao A, Rajkumar SV, Miguel JS, Avet-Loiseau H (2016) International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet oncol 17(8):e328–e346. https://doi.org/10.1016/s1470-2045(16)30206-6
An G, Li Z, Tai YT, Acharya C, Li Q, Qin X, Yi S, Xu Y, Feng X, Li C, Zhao J, Shi L, Zang M, Deng S, Sui W, Hao M, Zou D, Zhao Y, Qi J, Cheng T, Ru K, Wang J, Anderson KC, Qiu L (2015) The impact of clone size on the prognostic value of chromosome aberrations by fluorescence in situ hybridization in multiple myeloma. Clin cancer res 21(9):2148–2156. https://doi.org/10.1158/1078-0432.CCR-14-2576
Ross FM, Avet-Loiseau H, Ameye G, Gutiérrez NC, Liebisch P, O’Connor S, Dalva K, Fabris S, Testi AM, Jarosova M, Hodkinson C, Collin A, Kerndrup G, Kuglik P, Ladon D, Bernasconi P, Maes B, Zemanova Z, Michalova K et al (2012) Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders. Haematologica 97(8):1272–1277. https://doi.org/10.3324/haematol.2011.056176
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, Richardson P, Caltagirone S, Lahuerta JJ, Facon T, Bringhen S, Gay F, Attal M, Passera R, Spencer A, Offidani M, Kumar S, Musto P, Lonial S, Petrucci MT, Orlowski RZ, Zamagni E, Morgan G, Dimopoulos MA, Durie BG, Anderson KC, Sonneveld P, San Miguel J, Cavo M, Rajkumar SV, Moreau P (2015) Revised international staging system for multiple myeloma: a report from international myeloma working group. J clin oncol 33(26):2863–2869. https://doi.org/10.1200/JCO.2015.61.2267
Yan Y, Mao X, Liu J, Fan H, Du C, Li Z, Yi S, Xu Y, Lv R, Liu W, Deng S, Sui W, Wang Q, Zou D, Wang J, Cheng T, Zhan F, Tai YT, Yuan C, Du X, Qiu L, Anderson KC, An G (2019) The impact of response kinetics for multiple myeloma in the era of novel agents. Blood adv 3(19):2895–2904. https://doi.org/10.1182/bloodadvances.2019000432
Wang J, Tannous BA, Poznansky MC, Chen H (2020) CXCR4 antagonist AMD3100 (plerixafor): from an impurity to a therapeutic agent. Pharmacol res 159:105010. https://doi.org/10.1016/j.phrs.2020.105010
García-Ortiz A, Rodríguez-García Y, Encinas J, Maroto-Martín E, Castellano E, Teixidó J, Martínez-López J (2021) The role of tumor microenvironment in multiple myeloma development and progression. Cancers (Basel) 13(2). https://doi.org/10.3390/cancers13020217
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K, Brown J, Drayson MT, Selby PJ (2003) High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N engl j med 348(19):1875–1883. https://doi.org/10.1056/NEJMoa022340
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF, Casassus P, Maisonneuve H, Facon T, Ifrah N, Payen C, Bataille R (1996) A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Français du Myélome. N engl j med 335(2):91–97. https://doi.org/10.1056/nejm199607113350204
Lahuerta JJ, Paiva B, Vidriales MB, Cordón L, Cedena MT, Puig N, Martinez-Lopez J, Rosiñol L, Gutierrez NC, Martín-Ramos ML, Oriol A, Teruel AI, Echeveste MA, de Paz R, de Arriba F, Hernandez MT, Palomera L, Martinez R, Martin A, Alegre A, De la Rubia J, Orfao A, Mateos MV, Blade J, San-Miguel JF (2017) Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J clin oncol 35(25):2900–2910. https://doi.org/10.1200/jco.2016.69.2517
Cavo M, San-Miguel J, Usmani SZ, Weisel K, Dimopoulos MA, Avet-Loiseau H, Paiva B, Bahlis NJ, Plesner T, Hungria V, Moreau P, Mateos MV, Perrot A, Iida S, Facon T, Kumar S, van de Donk N, Sonneveld P, Spencer A et al (2022) Prognostic value of minimal residual disease negativity in myeloma: combined analysis of POLLUX, CASTOR, ALCYONE, and MAIA. Blood 139(6):835–844. https://doi.org/10.1182/blood.2021011101
Ho J, Yang L, Banihashemi B, Martin L, Halpenny M, Atkins H, Sabloff M, McDiarmid SA, Huebsch LB, Bence-Bruckler I, Giulivi A, Allan DS (2009) Contaminating tumour cells in autologous PBSC grafts do not influence survival or relapse following transplant for multiple myeloma or B-cell non-Hodgkin’s lymphoma. Bone marrow transplant 43(3):223–228. https://doi.org/10.1038/bmt.2008.318
Waszczuk-Gajda A, Feliksbrot-Bratosiewicz M, Król M, Snarski E, Drozd-Sokołowska J, Biecek P, Król M, Lewandowski Z, Peradzyńska J, Jędrzejczak WW, Dwilewicz-Trojaczek J (2018) Influence of clonal plasma cell contamination of peripheral blood stem cell autografts on progression and survival in multiple myeloma patients after autologous peripheral blood stem cell transplantation in long-term observation. Transplant proc 50(7):2202–2211. https://doi.org/10.1016/j.transproceed.2018.02.131
Azab AK, Runnels JM, Pitsillides C, Moreau AS, Azab F, Leleu X, Jia X, Wright R, Ospina B, Carlson AL, Alt C, Burwick N, Roccaro AM, Ngo HT, Farag M, Melhem MR, Sacco A, Munshi NC, Hideshima T et al (2009) CXCR4 inhibitor AMD3100 disrupts the interaction of multiple myeloma cells with the bone marrow microenvironment and enhances their sensitivity to therapy. Blood 113(18):4341–4351. https://doi.org/10.1182/blood-2008-10-186668
Kapoor P, Kumar SK, Dispenzieri A, Lacy MQ, Buadi F, Dingli D, Russell SJ, Hayman SR, Witzig TE, Lust JA, Leung N, Lin Y, Zeldenrust SR, McCurdy A, Greipp PR, Kyle RA, Rajkumar SV, Gertz MA (2013) Importance of achieving stringent complete response after autologous stem-cell transplantation in multiple myeloma. J clin oncol 31(36):4529–4535. https://doi.org/10.1200/jco.2013.49.0086
Goicoechea I, Puig N, Cedena MT, Burgos L, Cordón L, Vidriales MB, Flores-Montero J, Gutierrez NC, Calasanz MJ, Ramos MM, Lara-Astiaso D, Vilas-Zornoza A, Alignani D, Rodriguez I, Sarvide S, Alameda D, Garcés JJ, Rodriguez S, Fresquet V et al (2021) Deep MRD profiling defines outcome and unveils different modes of treatment resistance in standard- and high-risk myeloma. Blood 137(1):49–60. https://doi.org/10.1182/blood.2020006731
Diamond B, Korde N, Lesokhin AM, Smith EL, Shah U, Mailankody S, Hultcrantz M, Hassoun H, Lu SX, Tan C, Rustad EH, Maura F, Maclachlan K, Peterson T, Derkach A, Devlin S, Landau HJ, Scordo M, Chung DJ, Shah GL, Lahoud O, Thoren K, Murata K, Ramanathan L, Arcila ME, Ho C, Roshal M, Dogan A, Giralt SA, Landgren O (2021) Dynamics of minimal residual disease in patients with multiple myeloma on continuous lenalidomide maintenance: a single-arm, single-centre, phase 2 trial. Lancet haematol 8(6):e422–e432. https://doi.org/10.1016/s2352-3026(21)00130-7
Bal S, Dhakal B, Silbermann RW, Schmidt TM, Dholaria B, Giri S, Chhabra S, Medvedova E, Godby KN, D’Souza A, Hall AC, Hardwick P, Omel J, Cornell RF, Hari P, Callander NS, Costa LJ (2022) Impact of autologous hematopoietic cell transplantation on disease burden quantified by next-generation sequencing in multiple myeloma treated with quadruplet therapy. Am j hematol 97(9):1170–1177. https://doi.org/10.1002/ajh.26640
Boccadoro M, Omedé P, Dominietto A, Palumbo A, Bringhen S, Giaretta F, Ortolano B, Triolo S, Pileri A (2000) Multiple myeloma: the number of reinfused plasma cells does not influence outcome of patients treated with intensified chemotherapy and PBPC support. Bone marrow transplant 25(1):25–29. https://doi.org/10.1038/sj.bmt.1702085
Gertz MA, Witzig TE, Pineda AA, Greipp PR, Kyle RA, Litzow MR (1997) Monoclonal plasma cells in the blood stem cell harvest from patients with multiple myeloma are associated with shortened relapse-free survival after transplantation. Bone marrow transplant 19(4):337–342. https://doi.org/10.1038/sj.bmt.1700670
Wuillème S, Lok A, Robillard N, Dupuis P, Stocco V, Migné H, Dusquesne A, Touzeau C, Tiab M, Béné MC, Moreau P (2016) Assessment of tumoral plasma cells in apheresis products for autologous stem cell transplantation in multiple myeloma. Bone marrow transplant 51(8):1143–1145. https://doi.org/10.1038/bmt.2016.74
Funding
This investigation was supported by the International Cooperation Projects of National Natural Science Foundation (grant 81920108006, to L. Qiu), CAMS Innovation Fund for Medical Sciences (CIFMS) (grant 2022-I2M-1-022, to L. Qiu), and the National Natural Science Foundation (grant 81630007, to L. Qiu; grants 82270218 and 81670202, to G. An).
Author information
Authors and Affiliations
Contributions
JX analyzed data, interpreted the results, and drafted the manuscript; JX, WY, HF, JL, and LL collected data and performed patient follow-up; CD, SD, WS, YX, and GA acquired data and managed patients; GA suggested manuscript revisions; LQ and GA designed the study, revised the manuscript critically, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All patients were included in a prospective, non-randomized clinical trial (BDH 2008/02) approved by the Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Science & Peking Union Medical College, and the study was conducted in accordance with the local ethics committee and the Declaration of Helsinki.
Patient consent
Written informed consent was obtained from the patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, J., Yan, W., Fan, H. et al. Impact of residual tumor cells in the stem cell collection on multiple myeloma patients receiving autologous stem cell transplantation. Ann Hematol 102, 3195–3204 (2023). https://doi.org/10.1007/s00277-023-05427-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05427-8