Abstract
Early death (ED) is still the major obstacle to cure in acute promyelocytic leukemia (APL). Most studies focus on 30-day ED; however, little is known on predictors of death before starting APL treatment (very early death — VED) and on predictors of 7-day ED, the period with most deaths due to thrombohemorrhagic diathesis. We hypothesized whether the severity of the coagulopathy of APL could predict VED and 7-day ED. We also aimed to evaluate other characteristics associated with these outcomes. We undertook a retrospective, single-center observational study including newly diagnosed APL patients admitted to our institution between January 2000 and November 2022. Baseline demographical, clinical, and laboratorial data were collected. Statistical analysis was performed using Stata. One hundred four patients were included. The VED rate was 4.8%. A DIC Score ≥ 7 (p = 0.045), serum creatinine > 1.5 mg/dL (p < 0.001%), a DIC Score ≥ 6 within 24 h (p = 0.009), and mechanical ventilation (p < 0.001) were associated with VED. The 7-day ED rate was 12.5%. High-risk (p = 0.007) and hypogranular APL (p = 0.029), DIC Score at diagnosis (p = 0.047), DIC Score ≥ 7 (p = 0.043), DIC Score ≥ 6 within 24 h (p = 0.025), PT prolongation > 6 s (p = 0.002), and creatinine > 1.5 mg/dL (p = 0.004) were associated with 7-day ED. However, only elevated creatinine emerged as an independent predictor of 7-day ED (OR 21.4; p = 0.008). Our study shows that in patients with APL, an elevated creatinine at diagnosis strongly predicts for 7-day ED. A DIC Score ≥ 7 and a Score that remains ≥ 6 within 24 h and a serum creatinine > 1.5 mg/dL significantly associated with VED.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute promyelocytic leukemia (APL) has evolved from a grim prognosis to being the most curable subtype of acute leukemia today. Currently, the main obstacle to cure is still the significant risk of early death (ED) despite advances in targeted therapy and supportive care [1].
ED is commonly defined as death occurring within 30 days of APL diagnosis, and its incidence rate ranges from 0 to 8% in clinical trials [2, 3] to 29–32% in real-world registries [4, 5]. Even harder to estimate is the incidence of very early death (VED), occurring in newly diagnosed patients who expire before having the chance of starting all-transretinoic acid (ATRA), since these cases are underreported and excluded from clinical trials [6]. Thus, knowledge on the characteristics of these patients and on predictors of VED in APL is sorely lacking.
Most published studies in ED in APL focus on predictors of all-cause mortality during the first 30 days of APL. Bleeding is the main cause of ED and the key threat during the first week of APL diagnosis, as opposed to deaths caused by infection, differentiation syndrome, and other causes unrelated to APL’s thrombohemorrhagic diathesis, which rise beyond the first week [7]. Considering that three-quarters of all EDs occur during the first week of APL diagnosis [4], establishing the particular predictors of 7-day ED could have the most impact on refining routine care of APL patients during the hazardous first week of disease.
Since bleeding in APL is related to disseminated intravascular coagulation (DIC) and hyperfibrinolysis induced by leukemic cells, one could question whether more severe changes in coagulation parameters associate with life-threatening early bleeding and death in APL. Our group previously reported that a stable or increasing DIC Score of the International Society for Thrombosis over 48 h is associated with ED in APL patients [8].
Henceforth, we hypothesized whether the severity of the coagulopathy of APL, reflected by a higher DIC Score at diagnosis and within 24 h, could predict VED and 7-day ED. Secondly, we aimed to identify other baseline characteristics which could predict these impending catastrophic outcomes to improve current care and decrease VED and ED rates.
Methods
We performed a retrospective, single-center observational study, in which clinical records of all APL patients consecutively admitted to our institution between January 2000 and November 2022 were collected and reviewed after our local institution’s Ethics Committee approval. Diagnosis was suspected on observation of the peripheral blood smear and prompted immediate ATRA administration if the patient was able to take the capsules. APL was later confirmed by fluorescence in situ hybridization detection of t(15;17) or by identification of a PML-RARα transcript. All patients received blood products according to international guideline recommendations [9] — fresh frozen plasma to a target INR of < 1.3, platelet transfusions if platelets < 50 × 109/L and fibrinogen concentrate if serum fibrinogen < 150 mg/dL. All patients who started ATRA also began differentiation syndrome prophylaxis with prednisolone 0.5 mg/kg, as per local protocol.
Patient baseline demographics, blood work results including coagulation parameters, place of first medical evaluation, and APL characteristics were collected. The DIC Score of the International Society for Thrombosis and Hemostasis was calculated at diagnosis and up to 24 h later for each patient [10]. Very early death (VED) was defined as death occurring before initiation of APL-targeted treatment with ATRA, whereas 7-day ED was defined as death occurring within 7 days of APL diagnosis.
Statistical analysis was performed using Stata (version 13), using chi-square test and Mann–Whitney test for differences between VED versus remaining patients and between 7-day ED versus survivors beyond the first week of diagnosis. Logistic regression analysis was used to evaluate predictors of VED and of 7-day ED. A p value < 0.05 was considered statistically significant.
Results
VED, before initiation of APL treatment
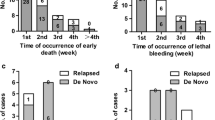
A total of 104 patients were included, with a median age of 47 years (17–84). In this cohort, 5 patients died due to APL-related bleeding before starting ATRA, all within 36 h of hospital admission (VED rate of 4.8%). Regarding the type of fatal bleed, 3 patients succumbed to intracranial hemorrhage, 1 to alveolar hemorrhage, and 1 to bleeding peptic ulcers unresponsive to cauterization through upper gastrointestinal endoscopy.
The remaining 99 patients in this cohort began treatment with ATRA 45 mg/m2 divided in two daily doses: 82 combined with chemotherapy, 16 with arsenic trioxide and 1 as monotherapy.
Table 1 summarizes the baseline characteristics of these 5 patients. All patients who died before ATRA administration were male, aged between 32 and 67 years. High-risk APL was diagnosed in 3 patients, while 2 had intermediate-risk disease. Most patients (4 out of 5) were referred from the emergency department of non-specialized hospitals with a suspected acute leukemia, and APL was confirmed upon arrival at our institution. Two patients were already under mechanical ventilation on arrival to our center due to impaired level of consciousness caused by intracranial bleeding at disease presentation.
The baseline differences between the VED group and remaining patients are depicted in Table 2. The patients who died before ATRA frequently presented with a DIC Score above 7 (60.0% vs 21.2%, p = 0.045) and maintained a DIC Score ≥ 6 within 24 h (100% vs 49.5%; p = 0.027). Concomitant acute renal failure with a serum creatinine > 1.5 mg/dL was also more common (60.0% vs 7.1%, p < 0.001%), and VED patients were also more likely to be mechanically ventilated before arrival to our tertiary hospital (40.0% vs 0%, p < 0.001). There were no differences regarding age, APL risk, leukocyte blood count, and coagulation parameters between the two groups.
Early death (ED), within 7 days of admission
Among the cohort of 104 patients, a total of 13 patients died within 7 days of APL diagnosis (7-day ED rate of 12.5%). Adding to the 5 patients who died before ATRA administration, 5 patients were treated with ATRA plus idarubicin, 2 patients with 7 + 3 plus ATRA (due to initial negative FISH assay for t(15;17) but subsequent PML-RARα detection by RT-PCR), while 1 patient was intended to be treated with ATRA plus idarubicin but expired before idarubicin administration.
While all patients who succumbed before ATRA died due to bleeding, this was not the case for all the patients with 7-day ED. Bleeding was still the main cause of death (6 due to intracranial bleeding, 1 to alveolar hemorrhage, and 1 to upper gastrointestinal bleeding), whereas 2 patients died due to thrombotic complications (1 with pulmonary embolism and 1 with acute myocardial infarction) and 2 patients succumbed to sudden cardiac arrest of uncertain etiology.
Comparison of the baseline differences between the group of 7-day ED versus all other patients is depicted in Table 3. In the 7-day ED group, high-risk APL (61.5% vs 25.3%, p = 0.007) and hypogranular variant APL (23.1% vs 4.4%, p = 0.016) were significantly more frequent, median leukocyte count was higher (p = 0.008), and median platelet was lower (p = 0.028) at diagnosis. Regarding coagulation profile differences, patients dying within the first week were more likely to have a baseline DIC Score ≥ 7 (p = 0.035), a PT prolongation above 6 s (p < 0.001), and a DIC Score ≥ 6 in the second coagulation assessment within 24 h of APL suspicion (p = 0.011). This 7-day ED patients also had a higher LDH (p = 0.009) and a serum creatinine above 1.5 mg/dL (p = 0.001).
As demonstrated in Table 4A, the following factors were identified to be significantly associated with 7-day ED by univariate logistic regression: high-risk APL (OR 4.3, p = 0.007), hypogranular APL (OR 6.2, p = 0.029), DIC Score at diagnosis (OR 1.6, p = 0.047), DIC Score ≥ 7 (OR 3.5, p = 0.043), DIC Score ≥ 6 in the second coagulation assessment within 24 h of APL suspicion (OR 5.0, p = 0.025), PT prolongation above 6 s from control (OR 7.8, p = 0.002), and creatinine above 1.5 mg/dL (OR 7.5, p = 0.004).
Building a multivariate analysis model despite the low number of events (Table 4B), the only independent predictor of 7-day ED was a serum creatinine > 1.5 mg/dL, which confers more than 21-times increased odds of ED within 7 days (OR 21.4, p = 0.008).
Discussion
This study identified an elevated baseline serum creatinine as the only independent predictor of 7-day ED, which also was significantly associated with VED. A serum creatinine > 1.5 mg/dL at diagnosis increased 21 times the odds of death within 7 days of APL diagnosis, and was present in 60% of patients with VED (versus 7.1%; p < 0.001).
The mechanisms behind acute renal failure in newly diagnosed APL may be several, such as microvascular thrombosis in the kidneys in the context of DIC [11], tumor lysis syndrome, or kidney hypoperfusion caused by distributive or hemorrhagic shock. Renal failure can also occur due to differentiation syndrome or to nephrotoxic drugs such as certain antibiotics, but these are frequent causes of renal failure later in APL treatment and not at diagnosis. Other published studies focusing on 30-day ED have also identified elevated serum creatinine as a marker of poorer prognosis [4, 12], so renal failure appears to be associated with worse outcomes in APL not only at diagnosis and in the early days of disease as we have shown, but also during the whole of induction treatment.
One of the hypotheses we aimed to test in this study was whether the severity of the coagulopathy of APL — which we defined as a higher DIC Score at diagnosis as well as the persistence of a high DIC Score within 24 h of disease — could predict VED and 7-day ED.
Regarding VED, while there was no statistically significant difference between the two groups in the individual coagulation baseline variables included in the DIC Score, a Score ≥ 7 was significantly associated with VED. A higher score in APL patients may thus reflect a more severe underlying coagulopathy. Additionally, the association of VED with the persistence of a high DIC Score within 24 h of disease suggests that the DIC Score may serve as a clinical tool in guiding more aggressive blood product transfusions in order to diminish the score of APL patients.
As for the impact of coagulation abnormalities on 7-day ED, a DIC Score ≥ 7 and a DIC Score ≥ 6 in the second coagulation assessment within 24 h of APL suspicion were also associated with death. Moreover, the DIC Score itself at diagnosis conferred 1.6 increased odds of 7-day ED per each 1-point Score increase, and the only coagulation parameter associated with ED was a PT prolongation above 6 s from control. These findings could suggest a potential role of these surrogates for severe coagulopathy in predicting 7-day ED, to be confirmed in a larger cohort. On multivariate analysis, only an elevated serum creatinine was significantly associated with ED.
Very few studies have focused on death before APL-specific treatment. To our knowledge, our present study and a study from Italy [13] are the only published papers focusing on predictors of death before APL treatment, which we defined as VED. In 2010, this Italian study reported 5 patients with fatal hemorrhagic complications before starting ATRA plus chemotherapy and found that these patients more frequently had delayed diagnosis, altered coagulation values, leukocytosis, a high peripheral blast count, and phenotypic expression of CD2 [13]. No logistic regression analysis was reported on this dataset. A real-life study from Brazil reported 7 patients with APL who died before receiving chemotherapy but who were given ATRA by enteric tube, who were mostly female and presented with high-risk disease, of whom 6 succumbed to intracranial or pulmonary bleeding [14].
In our cohort, the patients with VED were more likely to have altered coagulation values (as reflected by a DIC Score above 7 and a DIC Score ≥ 6 within 24 h of diagnosis), elevated creatinine, and to be mechanically ventilated before arrival to our center.
The fatal cases in our cohort reflect the difficulty of treating APL patients already in a critically ill condition upon hospital arrival due to a catastrophic disease presentation, which not only excludes their participation in trials but also does not allow delivery of standard APL therapy. Urgent treatment with ATRA is paramount upon APL suspicion since it counteracts the biochemical profile of coagulopathy-inducing atypical promyelocytes [15]. However, treatment with ATRA may be hindered for several reasons. First, patients may be unable to swallow capsules due to decreased alertness, because of intracranial bleeding, multiorgan dysfunction, or sedation for mechanical ventilation. In these scenarios, ATRA could be given via a nasogastric tube placed with precaution, but the size of the capsules and the inability to crush them can hamper their nasogastric administration. There are anecdotal reports on heating ATRA capsules in water until they melt [16], or dissolving ATRA with water and mineral oil into a slurry which can be more easily swallowed or administered via the tube [17]. The second scenario is that of patients under nil per os because of active gastric bleeding. These rare situations constitute a need for a commercialized intravenous formulation of ATRA, which has been studied previously as a liposomal formulation that was effective in inducing APL complete remission [18].
In our institution’s cohort, the mortality rate before starting treatment was 4.8%, which is comparable to that reported in the previously cited Italian single-center study (4.7%) [13]. In a Swedish population study, among the 29% of patients who died within 30 days of APL diagnosis, 35% never received ATRA, yielding a VED rate of approximately 10.5% [12]. These numbers show that death before APL treatment is frequent, underreported and probably underestimated, and preventing VED represents one of the few unmet needs in the field of APL.
In conclusion, while most ED studies in APL focus on 30-day mortality, our study shed light on predictors of VED and 7-day ED which are mediated mostly by the thrombohemorrhagic diathesis of APL. We identified a serum creatinine > 1.5 mg/dL, DIC Score ≥ 7, and a DIC Score ≥ 6 in the second coagulation assessment within 24 h of APL suspicion as being significantly associated with VED (with the statistical limitation of a small number of deaths defined as VED). High-risk APL, increasing DIC Score at diagnosis, a DIC Score ≥ 7, a DIC Score ≥ 6 in the second coagulation assessment within 24 h of APL suspicion, PT prolongation above 6 s from control, creatinine above 1.5 mg/dL, and hypogranular APL were identified as predictors of 7-day ED, with elevated creatinine emerging as the sole independent prognostic factor for death.
We highlight these potential prognostic factors to aid clinicians in recognizing patients with high risk of VED and 7-day ED, particularly an elevated baseline serum creatinine which is the only independent predictor of 7-day ED. The presence of these factors can contribute to considering alternative ways to deliver ATRA in unstable patients, and to intensifying renal support and disrupted hemostasis correction through intensive blood product support, in the hopes of overcoming one of the remaining obstacles to cure in APL.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Stahl M, Tallman MS (2019) Acute promyelocytic leukemia (APL): remaining challenges towards a cure for all. Leuk Lymphoma 60(13):3107–3115
Lo-Coco F, Avvisati G, Vignetti M, Thiede C, Orlando SM, Iacobelli S et al (2013) Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med 369(2):111–121
Lengfelder E, Haferlach C, Saussele S, Haferlach T, Schultheis B, Schnittger S et al (2009) High dose ara-C in the treatment of newly diagnosed acute promyelocytic leukemia: long-term results of the German AMLCG. Leukemia 23(12):2248–2258
Lehmann S, Ravn A, Carlsson L, Antunovic P, Deneberg S, Möllgrd L et al (2011) Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia 25(7):1128–1134
Jácomo RH, Melo RAM, Souto FR, de Mattos ER, de Oliveira CT, Fagundes EM et al (2007) Clinical features and outcomes of 134 Brazilians with acute promyelocytic leukemia who received ATRA and anthracyclines. Haematologica Italy 92:1431–2
Micol JB, Raffoux E, Boissel N, Lengliné E, Canet E, Daniel MT et al (2014) Management and treatment results in patients with acute promyelocytic leukaemia (APL) not enrolled in clinical trials. Eur J Cancer 50(6):1159–1168
de la Serna J, Montesinos P, Vellenga E, Rayón C, Parody R, León A et al (2008) Causes and prognostic factors of remission induction failure in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and idarubicin. Blood 111(7):3395–3402
Brioso Infante J, Esteves G, Martins H, Medeiros J, Alves D, Lopes C et al (2020) Disseminated Intravascular Coagulation Score evolution in 48 hours predicts early death in newly-diagnosed chemotherapy-treated acute promyelocytic leukemia patients. Blood [Internet]. 136:9. Available from: https://www.sciencedirect.com/science/article/pii/S0006497118702401. Accessed 19 July 2023
Sanz MA, Fenaux P, Tallman MS, Estey EH, Löwenberg B, Naoe T et al (2019) Management of acute promyelocytic leukemia: updated recommendations from an expert panel of the European LeukemiaNet. Blood 133(15):1630–1643
Toh CH, Hoots WK (2007) The scoring system of the scientific and standardisation committee on disseminated intravascular coagulation of the international society on thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost 5(3):604–606
Wada H, Matsumoto T, Suzuki K, Imai H, Katayama N, Iba T et al (2018) Differences and similarities between disseminated intravascular coagulation and thrombotic microangiopathy. Thromb J 16:14
Lehmann S, Ravn A, Carlsson L, Antunovic P, Deneberg S, Möllgård L et al (2011) Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the swedish adult acute leukemia registry. Leukemia 25(7):1128–1134
Breccia M, Latagliata R, Cannella L, Minotti C, Meloni G, Lo-Coco F (2010) Early hemorrhagic death before starting therapy in acute promyelocytic leukemia: association with high white blood cell count, late diagnosis and delayed treatment initiation. Haematologica 95(5):853–854
da Silva WF, da Rosa LI, Marquez GL, Bassolli L, Tucunduva L, Silveira DRA et al (2019) Real-life outcomes on acute promyelocytic leukemia in Brazil - early deaths are still a problem. Clin Lymphoma Myeloma Leuk. 19(2):e116-22
Stein E, McMahon B, Kwaan H, Altman JK, Frankfurt O, Tallman MS (2009) The coagulopathy of acute promyelocytic leukaemia revisited. Best Pract Res Clin Haematol [Internet]. 22(1):153–63. https://doi.org/10.1016/j.beha.2008.12.007
Bargetzi MJ, Tichelli A, Gratwohl A, Speck B (1996) Oral All-transretinoic acid administration in intubated patients with acute promyelocytic leukemia. Schweiz Med Wochenschr 126(45):1944–1945
Przybylski DJ, Jared JR, Fallon MJ (2021) Extemporaneous compounding and administration of tretinoin slurry for acute promyelocytic leukemia. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract 27(7):1779–1783
Douer D, Estey E, Santillana S, Bennett JM, Lopez-Bernstein G, Boehm K et al (2001) Treatment of newly diagnosed and relapsed acute promyelocytic leukemia with intravenous liposomal all-trans retinoic acid. Blood 97(1):73–80
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JI and JFL. The first draft of the manuscript was written by JI and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of Centro Académico de Medicina de Lisboa in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Infante, J., Esteves, G., Raposo, J. et al. Predictors of very early death in acute promyelocytic leukemia: a retrospective real-world cohort study. Ann Hematol 102, 3031–3037 (2023). https://doi.org/10.1007/s00277-023-05422-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05422-z