Abstract
We sought to evaluate the role of extramedullary disease (EMD) in sequential RIC retrospectively analyzing data of 144 high-risk AML patients undergoing HLA-matched transplantation. Median long-term follow-up was 11.6 years. Eighteen percent of patients (n = 26/144) presented with extramedullary AML (EM AML) or a history of EMD at time of transplantation. Overall relapse rate was 25% (n = 36/144) with 15% (n = 21/144) of all patients developing isolated BM relapse and 10% (n = 15/144) developing EM AML relapse with or without concomitant BM relapse (EM ± BM). Manifestation of EM relapse after transplantation occurred frequently at multiple sites and presented mostly as solid tumor mass. Only 3/15 patients with EM ± BM relapse showed a prior EMD manifestation. EMD prior to allogeneic transplantation had no impact on post-transplant OS when compared to non-EMD (median post-transplant OS 3.8 years versus 4.8 years; ns). Risk factors (p = < 0.1) for EM ± BM relapse included younger age and a higher number of prior intensive chemotherapies, whereas the presence of chronic GVHD was a protective factor. Median post-transplant OS (15.5 months vs. 15.5 months), RFS (9.6 months vs 7.3 months), and post-relapse OS (6.7 months vs. 6.3 months) were not significantly different between patients with isolated BM vs. EM ± BM relapse. Taken together, occurrence of EMD prior to as well as of EM ± BM AML relapse after transplantation was moderate, presenting mostly as solid tumor mass after transplantation. However, diagnosis of those does not seem to influence outcomes after sequential RIC. A higher number of chemotherapy cycles prior to transplantation was identified as recent risk factor for EM ± BM relapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a potential curative treatment option for patients with acute myeloid leukemia (AML) [1]. Despite the reduction of treatment-related mortality by the introduction of reduced-intensity conditioning (RIC) regimen and improvements in supportive treatments [2], relapse after allogeneic transplantation remains the most common cause that negatively affects long-term outcome [3], especially in patients suffering from high risk AML [4]. Whereas conventional conditioning regimens led to unsatisfying results in this patient cohort, sequential conditioning protocols, such as FLAMSA-RIC, have been successfully established [5, 6] enabling transplantation with acceptable toxicity profile and relapse rates. Thus, they advanced to standard of care at our and other institutions in high-risk, relapsed and refractory AML. Despite various analyses describing the feasibility and applicability throughout different donor transplantation settings [5, 7,8,9,10] and underlying diseases [11, 12], up to now, there is no study focusing on relapse pattern within this widespread used conceptual platform.
Relapse of AML after allo-HSCT can occur either as isolated relapse within the bone marrow (BM), or as extramedullary (EM) relapse either isolated or more frequently combined with concurrent relapse in the BM. EM AML relapse after allo-HSCT has been described with frequencies between 1 and 15% [13, 22] and up to 32% after haploidentical HSCT [23]. It remains controversial whether EM relapses after allogeneic HSCT yield a better [13, 15, 17] or a similar [16, 23] prognosis to relapses in the BM, mostly due to limitations caused by small patient numbers. Furthermore, little data is known regarding the features of AML with extramedullary disease (EMD), its relapse patterns and risk factors, as well as its impact on outcome when diagnosed prior to or after transplantation in a sequential RIC setting [5, 6, 10, 24].
The aim of our study was to assess the occurrence, the prognostic impact and risk factors for EM AML relapse development following a sequential-RIC allo-HSCT. Furthermore, we aimed to elucidate if differences in relapse disease presentation (BM relapse versus EMD with or without BM relapse) caused differences in outcomes, with a special focus on the role of a prior extramedullary manifestation and extramedullary relapse patterns.
Patients and methods
Patients
Analyses are based on patients with AML that underwent an HLA-matched allogeneic RIC-HSCT in our center between 2006 and 2010. All patients received sequential treatment based on FLAMSA (fludarabin (4 × 30 mg/m2), amasacrin (4 × 100 mg/m2), cytarabine (4 × 2000 mg/m2), followed by RIC composed of either total body irradiation (TBI) with 400 cGy or busulfan (Bu) (8 × 8 mg/kg). All patients received a GvHD prophylaxis with anti-thymocyte globulin (ATG, 3 × 10 mg/kg body weight or 3 × 20 mg/kg body weight in case of unrelated donors) plus cyclophosphamide (Cy) (2 × 40 mg/kg and 2 × 60 mg/kg in case of unrelated donors) followed by post-grafting immunosuppression with either cyclosporine A (CsA)/mycophenolate mofetil (MMF), tacrolimus/MMF or sirolimus/MMF or methotrexate (MTX).
Cytogenetic and molecular diagnostics
Cytogenetic and molecular analyses were performed in the leukemia diagnostic laboratory, following standard guidelines. For cytogenetic analyses ≥ 20 metaphases were assessed. Cytogenetic risk was defined according to the Medical Research Council (MRC) classification [25]. Mutations of NPM1, FLT3-ITD, FLT3-TKD and KMT2A-PTD (MLL-PTD) were assessed as previously published [26, 27].
Statistical methods
In our assessment for their potential prognostic impact on relapse risk, we included clinical parameters, disease parameters, therapeutic risk factors as well as post-transplant characteristics.
The following clinical and disease biology related variables were assessed: recipient age at time of allogeneic HSCT gender, ECOG status at allogeneic HSCT (0/1 versus (vs) 2), presence of prior EM manifestation, HCT-CI score (< 3 vs ≥ 3) [28], WBC at diagnosis, BM blasts at diagnosis, peripheral blasts at diagnosis, de novo vs. non de novo AML, FAB type, cytogenetic risk according to MRC, CN-AML vs. non-CN-AML, mutation status of NPM1, FLT3-ITD, FLT3-TKD, KMT2A-PTD, expression of T-cell markers, expression of CD56. Transplant-related variable included prior number of intensive chemotherapy cycles (continuous as well as < 2 vs ≥ 2), d16 blast clearance during induction treatment (< 10% vs ≥ 10%) [29], time from diagnosis to allogeneic HSCT, remission status before allogeneic HSCT (CR/CRi) vs. relapse/refractory disease vs. upfront allogeneic HSCT, donor characteristics such as HLA compatibility, donor type (related identical vs. unrelated identical vs. unrelated different), gender of donor/recipient, CMV state of donor/recipient, stem cell source (peripheral blood (PB) vs. BM), stem cell dose (CD34 + cells/kg), conditioning regimen and use of ATG 10 mg vs. 20 mg, GVHD prophylaxis (CsA/ MMF vs. others). Post-transplant characteristics that were assessed included: time from transplant until engraftment, time from transplant to relapse, time from transplant to onset of acute GVHD (aGVHD), acute and chronic GVHD (cGVHD) including severity grades as well as localization of aGVHD and cGVHD.
Statistical comparisons of risk factors between the types of relapses were assessed using the chi-square or Fisher exact test for categorical variables and the Kruskal–Wallis and Mann–Whitney U test for continuous factors. A binary logistic regression was performed to identify risk factors for dichotomous outcome parameters (EM relapse vs no EM relapse, BM relapse vs no BM relapse).
Post-transplant overall survival (OS) was defined as interval from date of allogeneic HSCT until death or last follow-up. Relapse free survival (RFS) was defined as time from allogeneic HSCT until relapse or last follow-up. Post-relapse overall survival was defined as interval from relapse after allogeneic HSCT and until death or last follow-up. Median follow-up time for survivors was calculated by the reverse Kaplan Meier method. Probabilities of post-transplant OS, RFS and post-relapse OS were calculated using the Kaplan–Meier method.
Results
Patient, disease, and transplant characteristics
Patient-, disease- and transplant characteristics are summarized in Table 1. Between 2006 and 2010, 144 adult patients with AML were treated with FLAMSA-RIC using TBI/Cy or FLAMSA-RIC using Bu/Cy followed by allogeneic HSCT at our center. Median age at allo-HSCT was 49 years (range: 18–71 years), 49% were female and 85% showed an ECOG of 0 or 1 at transplant (Table 1). 70% of patients had de novo AML, 19% secondary AML (sAML) and 10% therapy-related AML (tAML). The majority of patients had diagnosis of AML with an intermediate and adverse cytogenetic risk (68% and 24%, respectively). 52% were cytogenetically normal AML with mutations of NPM1, FLT3-ITD and FLT3-TKD in 35%, 27%, and 9% of cases. Most patients were transplanted in relapse or with refractory disease (51%).
At time of initial AML diagnosis 10 patients (7%) presented with EM manifestation while 16 patients (11%) developed EMD in the course of relapsed or refractory disease, summing up to patients presenting with or with a history of EMD at time of allo-HSCT.
The 26 patients with prior EMD at time of allo-HSCT (EM AML patients) showed a significantly higher WBC at first diagnosis (p = 0.03), were mostly female (p = 0.025) and were more frequently transplanted with a donor/recipient gender mismatch compared to patients without EM manifestation (p = 0.028) compared to 118 patients without EMD before allo-HSCT (Non-EM AML patients) (Table 1). In addition, we observed a trend towards more frequent occurrence of NPM1 (p = 0.068) and FLT3-TKD (p = 0.058) mutations in patients with EM AML.
Patients had received a median of 2 intensive chemotherapy cycles prior to allo-HSCT regardless of whether EMD manifestation was present or not (p = 0.889). Upfront HSCT was only performed in patients without EMD manifestation. Median time from diagnosis to allo-HSCT was 5.7 months in the overall cohort, 4.9 months in the non-EM AML and 7.4 months in EM AML patients (p = 0.060). We observed no significant differences in terms of donor type, stem cell source, conditioning regimen and post-grafting immunosuppression (Table 1).
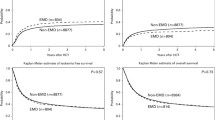
Outcome: survival and relapse comparing EM AML vs non-EM AML patients
Median follow-up for 64 survivors was 11.6 years (95% CI: 10.9–12.3 years). Median post-transplant OS for all 144 patients was 4.8 years (95% CI: 0.3–9.3) with a probability of OS at 3 years post-transplant of 57% (Figure S1A). EMD prior to allo-HSCT had no impact on post-transplant OS when compared with the non-EMD group (median post-transplant OS 3.8 years [95% CI: NA] versus 4.8 years [95% CI: 0.0–9.9 years], respectively and OS at 3 years 58% versus 57%, respectively) (Fig. 1A).
Median RFS was not reached (Figure S1B) and no statistical difference could be detected between patients with EMD at time of allo-HSCT and those without EMD (Fig. 1B). RFS at 3 years were 76% and 75%, respectively.
Cumulative relapse rates for the entire cohort at 3, 5, and 10 years after allogeneic HSCT were 20%, 23%, and 25%, respectively (data not shown). Relapse rate after allo-HSCT did not differ between patients with non-EM AML (n = 30/118, 25%) and patients that were diagnosed with prior EM AML (n = 6/26, 23%) (p = n.s.).
Relapse types and patterns
Thirty-six patients (25%) relapsed after allo-HSCT; fifteen of these showed EM relapse, either as isolated EM manifestation (n = 4) or concurrent to a BM relapse (n = 11), hereafter referred to as EM ± BM relapse.
One of 36 patients that relapsed was alive at last follow-up, 89% had died from leukemia (n = 32/36) and 8% (n = 3/36) of patients had died from infections. Median time from transplantation to relapse was 9.0 months (range: 0.4–118 months). Median post-relapse OS in 36 relapsed patients was 6.4 months (95% CI: 3.5–9.1 months) (Figure S1C). Six out of the 36 patients that relapsed showed late relapse (3 years post allo-HSCT), including 3 patients with very late relapse that occurred after 8, 9, and 10 years, all of which were located in the BM only.
While relapse rates were not different between the EMD and non-EMD group, regarding the relapse manifestation site, only three patients (patient numbers #10, #12, #18) with prior EM AML showed EM ± BM relapse, affecting new organ sites in all but one case (Fig. 2A and B). The other 12 patients presenting with EM ± BM relapse had no history of EMD (Fig. 2B).
Organ involvement in EM AML. (A) Extramedullary manifestations in 26 patients with EMD prior to allo HSCT. (B) Extramedullary manifestations in 15 patients with EM ± BM relapse after allo HSCT. Green boxes indicate manifestations prior to allo HSCT. Purple squares represent relapse manifestations. Underlined patients presented with EM AML at first diagnosis (n = 10)
EMD manifestations after allo-HSCT occurred more often at multiple sites compared to EMD manifestations before allo-HSCT or at initial diagnosis (53% vs 15%, respectively), and showed a different organ site distribution (Fig. 2A and B).
EM manifestation at first diagnosis corresponded to dispersed tissue infiltration by blast cells without formation of a tumor mass. Predominantly, the skin (50%) and gingiva (40%) were involved while hardly ever the CNS (10%) was included. However, prior to allo-HSCT meningeosis leucemica (31%) and CNS involvement (12%) were among the most frequent sites affected (Fig. 2A). Patients with EM involvement at relapse post allo-HSCT most commonly (93%) presented with a tumor mass corresponding to a myelosaroma. Mostly lymph nodes were affected (53%), and chloromatous tumor mass infiltration of multiple organs and tissues were observed, histologically proven in 80% of the cases (Fig. 2B).
Isolated BM and EM ± BM relapse: characteristics and risk factors
Patients with EM ± BM relapse vs isolated BM relapse showed a higher rate of de novo AML (80% vs 52%, p = 0.089) and the presence of NPM1 mutations in CN-AML (100% vs 13%, p = 0.058) (Table S1). All patients with isolated BM relapse had received a fully HLA-matched transplant compared to 80% in the combined EM ± BM group, where three patients were transplanted from an HLA-mismatched donor (HLA-match 9/10) (p 0.032) (Table S2). Most of the patients underwent transplantation with active disease. Herein the distribution within the relapse groups was similar (p = 0.631) (Table S2).
Post-transplant characteristics are depicted in Tables S3. Grade 1 aGVHD occurred in 75% of patients with isolated BM relapse vs 40% of patients with EM ± BM relapse (p = 0.096, Table S3), as also aGVHD occurred pre-dominantly in the skin-only in patients with isolated BM (92%) compared to 70% of patients with combined relapse (Table S3). Time until engraftment was similar in both groups of relapses (isolated BM: median 19 days EM ± BM: median 19 days), as well as time to onset of aGvHD (isolated BM: median 17 days EM ± BM:13 days). Time to relapse and time to death were not different between the different relapse types (Table S3).
Risk factors (p < 0.100) for the development of an isolated BM relapse included adverse cytogenetic risk according to MRC, an inadequate blast clearance (≥ 10%) at d16 during induction chemotherapy, and relapsed/refractory disease before allogeneic HSCT (Table 2, Tables S4 and S5). Protective factors that reduced the likelihood of isolated BM relapse included de novo AML vs non-de novo AML, the presence of CN-AML, presence of an NPM1 mutation, development of a grade 2–4 aGVHD as well as presence of cGVHD (Table 2, Tables S4 and S6).
In contrast, the only risk factors for the development of EM ± BM relapse included younger age at HSCT and a higher number of prior intensive chemotherapy cycles (Table 2, Tables S4 and S5). cGVHD was a protective factor (Table S6).
Outcome: survival and relapse comparing patients with isolated BM vs EM ± BM relapse
Median post-transplant OS in patients with isolated BM relapse and EM ± BM relapse was 15.5 (95% CI: 10.7–20.2) and 15.5 (95% CI: 0.5–30.9) months, respectively, and as such did not reveal significant differences (Fig. 3A). Median post-transplant OS in patients with isolated BM relapse, isolated EM AML relapse and EM + BM relapse was 15.5 (95% CI: 10.7–20.2), 12.1 (95% CI: 0.0–31.1), and 15.5 (95% CI: 1.9–29.1) months, respectively, and did also not reveal significant differences (Figure S2A).
Median RFS was not significantly different in patients with isolated BM relapse compared to patients with EM ± BM relapse (9.6 months; 95% CI: 8.1–11.2 vs. 7.3 months; 95% CI: 5.9–8.7), (Fig. 3B). Median RFS was similar between patients with isolated BM vs. EM ± BM relapse and tended to be longest in patients with isolated EM relapse (Figure S2B).
Median post-relapse OS was similar comparing patients with isolated BM relapse to patients with EM AML relapse with or without concomitant BM relapse (6.7 months; 95% CI: 2.0–11.4 vs. 6.3 months; 95% CI: 3.5–9.2) (Fig. 3C). Median post-relapse OS in patients with isolated BM relapse, isolated EM relapse and EM + BM relapse was 6.7 (95% CI: 2.0–11.4), 3.1 (95% CI: 0.1–6.1) and 7.6 (95% CI: 4.5–10.6) months, respectively (Figure S2C). Patients with isolated EM relapse showed a significant shorter post-relapse OS compared to patients with isolated BM relapse (p = 0.049) as well as compared to patients with combined EM + BM relapse (Median post-relapse OS: 3.1 months vs. 7.6 months p = 0.014) (Figure S2C). Forty-three percent of patients with isolated BM relapse and 47% of patients with EM ± BM relapse received a second allo-HSCT (data not shown). Only one of the four patients with isolated EM relapse was referred to a potentially curative second allo-HSCT.
When analyses were restricted to patients that had received a treatment with a curative intent (e.g., a second allogeneic HSCT), there were no significant differences with regard to OS and RFS comparing patients with different relapse subtypes (Figures S3 and S4).
Patients with isolated BM relapse and EM with or without concomitant BM relapse showed similar post-relapse OS of 8.9 and 8.6 months, respectively (Figure S5A). One patient with isolated EM relapse showed a shorter post-relapse OS compared to 9 patients with isolated BM relapse (median post-transplant OS: 4.0 months vs. 8.9 months, p = 0.069) as well as compared to 6 patients with combined EM + BM relapse (4.0 months vs 8.6 months, p = 0.014) (Figure S5B).
Discussion
The goal of this study was to investigate the occurrence, the prognostic impact, and risk factors for EM AML relapse as well as the association of prior EM AML with outcomes after allogeneic transplantation in a uniformly treated patient cohort receiving sequential FLAMSA-RIC. In the light of limited published data regarding relapse behavior and impact on survival once disease recurred after transplantation, we particularly sought to assess relapse patterns and to identify risk factors for the development of extramedullary relapse after transplantation.
Our study is based on high-risk AML patients receiving a homogeneous conditioning regimen in preparation for HLA-matched transplantation. In our cohort 18% of the patients presented with EMD before transplant. In line with previous publications, regarding clinical presentation at first diagnosis, AML with EM was associated with significantly higher WBC at diagnosis and more frequently tended to harbor NPM1 and FLT3-TKD mutation [30]. Intriguingly, at first diagnosis CNS involvement was rare, however prior to allo-HSCT it made up 43% of EM sites in our cohort. This might be explained by the fact, that we perform CNS staging routinely prior to advancing to allo-HSCT, whereas we do not assess CNS involvement a first diagnosis if the patient presents without related symptoms.
Once transplanted overall relapse rate was 25%, which is similar to data published by Schmid et al [5] (20% relapse rate) in patients with high-risk AML who received FLAMSA-RIC allo-HSCT, but lower compared to other studies in AML patients with various other RIC regimen (30–60% relapse rate) [31, 33]. Rate of EM relapse in our study with 10.4% was moderate in the setting of HLA-matched transplantation. This is similar to 12.9% of EM relapse after RIC for allo-HSCT in high risk AML patients undergoing HLA-matched transplantation reported by Schmid et al. [24], but higher compared to 6–7% in other RIC studies, including all or the majority of patients transplanted in CR [14, 34].
Among the twenty-six patients within our cohort with EMD at diagnosis and prior to transplantation, only three relapsed with EM involvement, underlining the effectiveness of allo-HSCT as a curative treatment also in EM AML. Interestingly, sites affected in patients with EM relapse were multiple showing mostly a solid tumor mass manifestation and mostly did not overlap with the ones at first diagnosis, strongly suggesting that immune escape mechanisms might lead to a different relapse pattern after allo-HSCT [35].
Our study has a long median follow-up time for survivors of 11.6 years, which allows for the detection of late relapses. In fact, 6/36 patients relapsed 3 years after allogeneic HSCT, and another 3 patients developed very late relapses after 8, 9, and 10 years. In contrast to data from Watts et al. who suggested that very late relapses occur predominantly in an EM localization [36] all 3 very late relapses in our study occurred in the BM. However, as at the beginning of the millennium only few mutations were tested in AML patients, it remains unclear whether these late relapses in our cohort were relapses indeed, or on the contrary new therapy-derived AMLs (t-AML) or donor cell derived AMLs as they might nowadays be diagnosed.
Interestingly, risk factors for BM relapses versus EM relapses differed suggesting a difference in their etiology. In addition to known risk factors for the development of relapse such as AML with an adverse cytogenetic risk according to MRC or relapsed/refractory disease before allo-HSCT [3, 17] our study suggests that an inadequate blast clearance (≥ 10%) at d16 during induction therapy is not only a prognostic factor for long-term outcome in AML during conventional chemotherapy [29] but also an indicator of a higher likelihood of BM relapse in the context of allogeneic transplantation. Similarly, the presence of an NPM1 mutation at diagnosis was found to be a protective factor reducing the likelihood for BM relapse. Rollig et al. showed a longer RFS in patients with NPM1 + mutated AML after allo-HSCT [37] compared to standard chemotherapy. In this context, a limitation of our study is the lack of MRD data since, e.g., NPM1-MRD status post-HSCT has been shown to improve risk assessment for relapse [38]. The only 2 risk factors for the development of EM relapse included younger age and a higher number of induction cycles before allogeneic transplant. Age < 18 years was a risk factor for EM relapse identified by Harris et al. [17]. A higher number of chemotherapy cycles has not been reported before as a risk factor for EM disease but the requirement for more therapy cycles might be a surrogate for a more aggressive disease. Risk factors as disease phase (more relapse/refractory disease) at transplant [17, 21] and poor cytogenetics [17, 19] have been described in other studies that focused on isolated EM disease, in contrast to our analyses that was limited by small numbers of isolated EM relapse and therefore had to combine EM ± BM relapse. While some authors have suggested cGVHD [13, 17] to be associated with EM relapse, this was not observed in a large study performed by Shem-Tov who found that presence of aGVHD or cGVHD was a protective factor for risk of BM relapse, but had no effect on isolated EM relapse risk [19]. In line with these data, we found that aGVHD grade 2–4 lowers the risk for a BM relapse, while it did not affect the risk of EM ± BM relapse. The presence of cGVHD was a protective factor for both types of relapses, reducing the risk of BM as well as of EM ± BM relapse.
Several studies suggest that isolated EM relapse occur later compared to BM relapses [14,15,16, 19]. We similarly observed a trend to a longer RFS in patients with isolated EM relapse compared to isolated BM relapse. Due to the small number of patients and different treatment strategies post relapse this did not reach statistical significance.
Existing data for prognosis of patients with EM AML relapse compared to BM relapse after allogeneic HSCT is limited and conflicting due to small patient numbers and heterogeneity of patient cohorts and the discrepancy between histologically confirmed and clinically diagnosed EMD. In 80% of our cohort EM AML relapse was histologically confirmed. Shem-Tov et al. demonstrated a better survival of 31 patients with AML or ALL with isolated EM relapses compared to BM relapse. [19]. Similarly, Sohl et al. whose analyses were based on AML patients only found a significantly better post-relapse survival in patients with isolated EM relapses (n = 13) compared to those with concurrent BM (n = 12) [14]. Chong et al. whose analyses were based on a variety of different hematological malignancies that underwent allo-HSCT including AML, 15 patients with EM ± BM relapse had a favorable post-relapse survival compared to BM relapses [13]. In contrast, one of largest studies including 38 isolated EM relapses and 149 BM relapses in patients with AML or ALL and with a long term follow-up, did not demonstrate differences in outcome depending on the type of relapse [21]. Similarly, Curley et al. did not observe difference in outcome between EM ± BM vs BM relapses [16]. In line with these studies, we did not find a survival benefit for patients with EM ± BM relapse compared to BM relapse. Despite other studies, subgroup analyses differentiating effects of isolated EM from other forms of relapses were challenging due to the small number of patients with isolated EM AML relapse affecting only 4 patients in our cohort. Post-relapse survival tended to be shorted in our four patients with isolated EM relapse, but this was likely due to the fact that 3 of 4 patients had not received another therapy in curative intent and thus did not undergo a potentially curative second allo-HSCT.
Taken together, we observed a moderate occurrence of EM relapses in high-risk AML patients with a feature change to more solid presentation of EMD after FLAMSA-RIC HLA-matched allo-HSCT. We have assessed a wide range of clinical, disease specific, therapeutic and post-transplant characteristics with regard to their impact on BM or EM ± BM relapse risk. Although risk factors for BM vs. EM relapse differed, suggesting a different etiology of these relapse types, overall survival and post-relapse survival was comparable between the two groups. Our long-term follow up enabled us to detect three very late relapses that occurred after 8, 9, and 10 years which emphasizes the need for a long-term close follow-up of AML patients after transplantation. The presence of EMD prior to allo-HSCT did not influence outcomes following sequential-RIC transplantation underlining the effectiveness of this strategy as a curative treatment option also in the treatment of patients with EM AML.
References
Gyurkocza B, Lazarus HM, Giralt S (2017) Allogeneic hematopoietic cell transplantation in patients with AML not achieving remission: Potentially curative therapy. Bone Marrow Transplant 52(8):1083–1090
Hamadani M, Mohty M, Kharfan-Dabaja MA (2011) Reduced-intensity conditioning allogeneic hematopoietic cell transplantation in adults with acute myeloid leukemia. Cancer Control 18(4):237–245
Tsirigotis P, Byrne M, Schmid C et al (2016) Relapse of AML after hematopoietic stem cell transplantation: Methods of monitoring and preventive strategies. A review from the ALWP of the EBMT. Bone Marrow Transplant 51(11):1431–1438
Scott BL (2020) Allogeneic stem cell transplantation for high-risk acute leukemia and maintenance therapy: No time to waste. Blood Adv 4(13):3200–3204
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ (2005) Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol 23(24):5675–5687
Schmid C, Schleuning M, Schwerdtfeger R et al (2006) Long-term survival in refractory acute myeloid leukemia after sequential treatment with chemotherapy and reduced-intensity conditioning for allogeneic stem cell transplantation. Blood 108(3):1092–1099
Blaise DP, Boiron JM, Faucher C et al (2005) Reduced intensity conditioning prior to allogeneic stem cell transplantation for patients with acute myeloblastic leukemia as a first-line treatment. Cancer 104(9):1931–1938
Tischer J, Stemmler HJ, Engel N et al (2013) Feasibility of clofarabine cytoreduction followed by haploidentical hematopoietic stem cell transplantation in patients with relapsed or refractory advanced acute leukemia. Ann Hematol 92(10):1379–1388
Ringdén O, Labopin M, Schmid C et al (2017) Sequential chemotherapy followed by reduced-intensity conditioning and allogeneic haematopoietic stem cell transplantation in adult patients with relapse or refractory acute myeloid leukaemia: a survey from the Acute Leukaemia Working Party of EBMT. Br J Haematol 176(3):431–439
Fraccaroli A, Prevalsek D, Fritsch S et al (2018) Sequential HLA-haploidentical transplantation utilizing post-transplantation cyclophosphamide for GvHD prophylaxis in high-risk and relapsed/refractory AML/MDS. Am J Hematol 93(12):1524–1531
Zoellner A-K, Fritsch S, Prevalsek D et al (2015) Sequential therapy combining clofarabine and T-cell-replete HLA-haploidentical haematopoietic SCT is feasible and shows efficacy in the treatment of refractory or relapsed aggressive lymphoma. Bone Marrow Transplant 50(5):679–684
Duléry R, Ménard AL, Chantepie S et al (2018) Sequential Conditioning with Thiotepa in T Cell- Replete Hematopoietic Stem Cell Transplantation for the Treatment of Refractory Hematologic Malignancies: Comparison with Matched Related, Haplo-Mismatched, and Unrelated Donors. Biol Blood Marrow Transplant 24(5):1013–1021
Chong G, Byrnes G, Szer J, Grigg A (2000) Extramedullary relapse after allogeneic bone marrow transplantation for haematological malignancy. Bone Marrow Transplant 26(9):1011–1015
Solh M, DeFor TE, Weisdorf DJ, Kaufman DS (2012) Extramedullary Relapse of Acute Myelogenous Leukemia after Allogeneic Hematopoietic Stem Cell Transplantation: Better Prognosis Than Systemic Relapse. Biol Blood Marrow Transplant 18(1):106–112
Shi JM, Meng XJ, Luo Y et al (2013) Clinical characteristics and outcome of isolated extramedullary relapse in acute leukemia after allogeneic stem cell transplantation: A single-center analysis. Leuk Res 37(4):372–377
Curley C, Durrant S, Kennedy GA (2013) Is extramedullary relapse of acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation associated with improved survival? Asia Pac J Clin Oncol 9(3):285–289
Harris AC, Kitko CL, Couriel DR et al (2013) Extramedullary relapse of acute myeloid leukemia following allogeneic hematopoietic stem cell transplantation: Incidence, risk factors and outcomes. Haematologica 98(2):179–184
Ge L, Ye F, Mao X et al (2014) Extramedullary relapse of acute leukemia after allogeneic hematopoietic stem cell transplantation: Different characteristics between acute myelogenous leukemia and acute lymphoblastic leukemia. Biol Blood Marrow Transplant 20(7):1040–1047
Shem-Tov N, Saraceni F, Danylesko I et al (2017) Isolated Extramedullary Relapse of Acute Leukemia after Allogeneic Stem Cell Transplantation: Different Kinetics and Better Prognosis than Systemic Relapse. Biol Blood Marrow Transplant 23(7):1087–1094
Alhashim N, Aljurf M, Hassanein M et al (2018) Extramedullary relapses after allogeneic stem cell transplantation for acute myeloid leukemia: clinical characteristics, incidence, risk factors and outcomes. Bone Marrow Transplant 53:838–843
Sakellari I, Gavriilaki E, Batsis I et al (2019) Isolated Extramedullary Relapse as a Poor Predictor of Survival after Allogeneic Hematopoietic Cell Transplantation for Acute Leukemia. Biol Blood Marrow Transplant 25(9):1756–1760
Yuda S, Fuji S, Onishi A et al (2019) Extramedullary Relapse of Acute Myelogenous Leukemia after Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant 25(6):1152–1157
Yoshihara S, Ikegame K, Kaida K et al (2012) Incidence of extramedullary relapse after haploidentical SCT for advanced AML/myelodysplastic syndrome. Bone Marrow Transplant 47(5):669–676
Schmid C, Labopin M, Nagler A et al (2012) Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensity conditioning for allogeneic stem cell transplantation. Blood 119(6):1599–1606
Grimwade D, Hills RK, Moorman AV et al (2010) Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 116(3):354–365
Benthaus T, Schneider F, Mellert G et al (2008) Rapid and sensitive screening for CEBPA mutations in acute myeloid leukaemia. Br J Haematol 143(2):230–239
Schneider F, Hoster E, Unterhalt M et al (2009) NPM1 but not FLT3-ITD mutations predict early blast cell clearance and CR rate in patients with normal karyotype AML (NK-AML) or high-risk myelodysplastic syndrome (MDS). Blood 113(21):5250–5253
Sorror ML, Maris MB, Storb R et al (2005) Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106(8):2912–2919
Kern W, Haferlach T, Schoch C et al (2003) Early blast clearance by remission induction therapy is a major independent prognostic factor for both achievement of complete remission and long-term outcome in acute myeloid leukemia: data from the German AML Cooperative Group (AMLCG) 1992 Trial. Blood 101(1):64–70
Eckardt JN, Stölzel F, Kunadt D et al (2022) Molecular profiling and clinical implications of patients with acute myeloid leukemia and extramedullary manifestations. J Hematol Oncol 15(1):1–13
Blaise D, Tabrizi R, Boher JM et al (2013) Randomized study of 2 reduced-intensity conditioning strategies for human leukocyte antigen-matched, related allogeneic peripheral blood stem cell transplantation: Prospective clinical and socioeconomic evaluation. Cancer 119(3):602–611
Beelen DW, Trenschel R, Stelljes M, Groth C, Masszi T, Reményi P, Wagner-Drouet EM, Hauptrock B, Dreger P, Luft T, Bethge W, Vogel W, Ciceri F, Peccatori J, Stölzel F, Schetelig J, Junghanß C, Grosse-Thie C, Michallet M, Labussiere-Wallet H, Schaefer-Eckart K, Dressler S, Grigoleit GU, Mielke S, Scheid C, Holtick U, Patriarca F, Medeot M, Rambaldi A, Micò MC, Niederwieser D, Franke GN, Hilgendorf I, Winkelmann NR, Russo D, Socié G, Peffault de Latour R, Holler E, Wolff D, Glass B, Casper J, Wulf G, Menzel H, Basara N, Bieniaszewska M, Stuhler G, Verbeek M, Grass S, Iori AP, Finke J, Benedetti F, Pichlmeier U, Hemmelmann C, Tribanek M, Klein A, Mylius HA, Baumgart J, Dzierzak-Mietla M, Markiewicz M (2020) Treosulfan or busulfan plus fludarabine as conditioning treatment before allogeneic haemopoietic stem cell transplantation for older patients with acute myeloid leukaemia or myelodysplastic syndrome (MC-FludT.14/L): a randomised, non-inferiority, phase 3 trial. Lancet Haematol 7(1):e28–e39. https://doi.org/10.1016/S2352-3026(19)30157-7
Craddock C, Jackson A, Loke J et al (2021) Augmented reduced-intensity regimen does not improve postallogeneic transplant outcomes in acute myeloid leukemia. J Clin Oncol 39(7):768–778
Kogut N, Tsai NC, Thomas SH et al (2013) Extramedullary relapse following reduced intensity allogeneic hematopoietic cell transplant for adult acute myelogenous leukemia. Leuk Lymphoma 54(3):665–668
Zeiser R, Vago L (2019) Mechanisms of immune escape after allogeneic hematopoietic cell transplantation. Blood 133(12):1290–1297
Watts JM, Wang XV, Swords RT et al (2016) Very late relapse of AML after allogeneic hematopoietic cell transplantation is often extramedullary. Bone Marrow Transplant 51(7):1013–1015
Röllig C, Bornhäuser M, Kramer M et al (2015) Allogeneic stem-cell transplantation in patients with NPM1-mutated acute myeloid leukemia: Results from a prospective donor versus no-donor analysis of patients after upfront HLA typing within the SAL-AML 2003 trial. J Clin Oncol 33(5):403–410
Zhou Y, Othus M, Walter RB et al (2018) Deep NPM1 Sequencing Following Allogeneic Hematopoietic Cell Transplantation Improves Risk Assessment in Adults with NPM1-Mutated AML. Biol Blood Marrow Transplant 24(8):1615–1620
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures involving human participants were in accordance with the institutional ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fraccaroli, A., Vogt, D., Rothmayer, M. et al. Impact of extramedullary disease in AML patients undergoing sequential RIC for HLA-matched transplantation: occurrence, risk factors, relapse patterns, and outcome. Ann Hematol 102, 2213–2223 (2023). https://doi.org/10.1007/s00277-023-05281-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05281-8