Abstract
We sought to evaluate the efficacy of the purine analogue cladribine in 79 patients with advanced systemic mastocytosis (AdvSM) using data from the ‘German Registry on Disorders of Eosinophils and Mast Cells (GREM)’. The overall response rate according to modified Valent criteria (46 evaluable patients) for first- (1L) and second-line (2L) cladribine treatment was 41% (12/29) and 35% (6/17, P = 0.690), respectively, and the median overall survival (OS, all patients evaluable) was 1.9 years (n = 48) and 1.2 years (n = 31; P = 0.311). Univariate and multivariable analyses of baseline and on-treatment parameters identified diagnosis of mast cell leukemia (hazard ratio [HR] 3.5, 95% confidence interval [CI, 1.3–9.1], P = 0.012), eosinophilia ≥ 1.5 × 109/L (HR 2.9 [CI 1.4–6.2], P = 0.006) and < 3 cycles of cladribine (HR 0.4 [CI 0.2–0.8], P = 0.008) as independent adverse prognostic parameters for OS. There was no impact of other laboratory (anemia, thrombocytopenia, serum tryptase) or genetic markers (mutations in SRSF2, ASXL1 or RUNX1) on OS. In consequence, none of the recently established prognostic scoring systems (MARS, IPSM, MAPS or GPSM) was predictive for OS. Modified Valent criteria were superior to a single factor-based response assessment (HR 2.9 [CI 1.3–6.6], P = 0.026). In conclusion, cladribine is effective in 1L and 2L treatment of AdvSM. Mast cell leukemia, eosinophilia, application of < 3 cycles and a lack of response are adverse prognostic markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic mastocytosis (SM) is a rare myeloid neoplasm characterized by multifocal accumulation of neoplastic mast cells (MC) in the bone marrow (BM), visceral organs and skin [1,2,3,4]. Advanced systemic mastocytosis (AdvSM) comprises aggressive SM (ASM), SM with an associated hematologic neoplasm (AHN), and MC leukemia (MCL). SM phenotype driver is an acquired somatic point mutation in KIT at codon D816V (KIT D816V) found in > 90% of AdvSM patients [5, 6]. In addition, 60–80% of patients harbor additional somatic mutations, e.g. in SRSF2, ASXL1, RUNX1 (S/A/R gene panel), NRAS, or DNMT3A, which are important parameters for combined clinico-genetic prognostic risk scoring systems (e.g., Mutation-Adjusted Risk Score, MARS; Mayo Alliance Prognostic System, MAPS; Global Prognostic Score for SM, GPSM) [7,8,9,10,11,12].
The development of novel targeted drugs, e.g., the multikinase inhibitor midostaurin [13,14,15] and the KIT D816V inhibitor avapritinib [16, 17], has extended the therapeutic options for patients with AdvSM, which were previously based on the off-label use of the purine analogue cladribine [18,19,20,21,22]. However, recent data on response rates and variably on leukemia-free (LFS), event-free- (EFS) and overall survival (OS) meanwhile favor the use of midostaurin and avapritinib [23,24,25,26]. Notwithstanding, cladribine will remain a relevant treatment option beyond first-line treatment due to intolerance, resistance and progression on KIT inhibitors [23, 27, 28]. No predictive markers have yet been established for response, resistance and survival in cladribine-treated AdvSM patients [18,19,20,21,22], a gap which we aimed to fill by analysis of a comprehensive cohort of 79 cladribine-treated patients enrolled within the ‘German Registry on Disorders of Eosinophils and Mast Cells’ (GREM).
Patients and methods
Study population
All cladribine-treated patients (n = 79) from the GREM which were diagnosed between 2003 and 2021 were selected for this project, which is an updated and more detailed analysis of a comparative study between midostaurin and cladribine [23]. The diagnosis of SM was established according to the World Health Organization classification [1, 29,30,31]. All BM biopsies were evaluated by reference pathologists (H.-P.H., K.S.) of the European Competence Network on Mastocytosis (ECNM) [32]. The study design adhered to the tenets of the Declaration of Helsinki and was approved by the institutional review board of the Medical Faculty of Mannheim, Heidelberg University, Germany. Written informed consent was provided by all patients.
Treatment
The number of patients allowed separation of first- (1L) and second-line (2L) treatment. Prior treatment included midostaurin while subsequent treatment approaches included (individually or sequentially) midostaurin, avapritinib, acute myeloid leukemia-like intensive chemotherapy and, rarely, allogeneic stem cell transplantation. Treatment options with a potentially low disease-modifying impact (e.g. interferon-alpha) or solely directed towards AHN (e.g. hydroxyurea, azacytidine) were not considered as 1L- or 2L-treatment.
Gene mutation analyses
Quantitative assessment of the KIT D816V expressed allele burden (EAB) was performed by allele-specific quantitative real-time reverse-transcriptase polymerase chain reaction (RT-qPCR) analysis on RNA/complementary DNA as previously described [33]. NGS analyses on DNA were performed through library preparation by the Access Array Technology (Fluidigm, San Francisco, CA) and sequencing on the MiSeq Instrument (Illumina, San Diego, CA). Gene mutations were annotated using the reference sequence of the Ensembl Transcript ID (Ensembl release 85: July 2016).
Prognostic scoring systems
The predictive value and clinical utility of several recently established prognostic scoring systems (MARS, International Prognostic Scoring System for AdvSM [IPSM-AdvSM], MAPS, and GPSM) was conducted according to published criteria [7, 11, 12, 34]. Similarities and differences between the scores are given elsewhere. [11, 30]
Response assessment
Response assessment according to modified Valent criteria [21] included regular monitoring of C-findings, serum tryptase and a BM biopsy within 2 months after the last applied course of cladribine. The reasons for not using the more recently established International Working Group-Myeloproliferative Neoplasms Research Treatment-ECNM (IWG-MRT-ECNM) criteria included: (i) the retrospective nature of our analysis did not allow to adequately address the complex IWG-MRT-ECNM criteria, (ii) the modified Valent response criteria were commonly used for response assessment of cladribine in prior studies. Molecular response was defined as KIT D816V expressed allele burden reduction ≥ 25% within 2 months after the last course. [7, 23, 33, 35]
Statistical analyses
All statistical analyses considering clinical, laboratory and molecular parameters were obtained at the time of diagnosis/first referral to our center (initial parameters), treatment initiation with cladribine (baseline parameters) and at multiple time points during treatment (including time point for response assessment). The Mann–Whitney U-test was used to compare continuous variables and medians of distributions. Fisher’s exact test was used for categorical variables. We retrospectively analyzed the OS (time of diagnosis/treatment initiation to the date of death/last visit) by using the Kaplan–Meier method with log-rank test for group comparisons/visualizations. Disease progression was defined as a shift to a more aggressive AdvSM subtype (secondary MCL or secondary acute myeloid leukemia [AML]). Duration of treatment was defined as the duration from initiation of cladribine to discontinuation for any reason. For the estimation of hazard ratios (HRs) and multivariable analysis, the Cox proportional hazard regression model was used. All variables that showed prognostic significance in univariate analyses were included in multivariable analyses. The first multivariable analysis was performed in an unmodified cohort of patients irrespective of prior or following treatment approaches (midostaurin, avapritinib, intensive chemotherapy and allogeneic stem cell transplantation); the second multivariable analysis was performed in a modified cohort in which patients with prior or following treatment approaches were either excluded or censored at the time of initiation of the next treatment line. P values of < 0.05 (two-sided) were considered as significant. Data management and statistical analyses were performed with SPSS (SPSS version 20.0; IBM Corporation, Armonk, NY) and GraphPad Prism software (version 8, GraphPad, La Jolla, CA, USA).
Results
Therapeutic modalities
Cladribine was used at a dose of 0.14 mg/kg/day subcutaneously or intravenously on days 1–5 of a 28-day course. For both 1L- (n = 48, 61%) and 2L-treatment (n = 31, 39%), a median number of 3 cycles (range 1–6 and 1–8, respectively) was applied over a median of 3.3 (range 0.1–16.0) and 3.0 months (range 0.1–28.5), respectively (P = 0.612; Table 1). Three or more cycles were applied in 32/79 (41%) patients (1L, n = 21, 44%; 2L, n = 11, 35%). The main reasons for dose reduction, e.g. application only on days 1–3 or extension of intervals, was prolonged myelosuppression (15/79, 19%).
Comparison of baseline characteristics
Compared to 1L-treatment, patients on 2L-treatment presented with a higher frequency of anemia (61% vs. 35%, P = 0.039), a higher percentage of BM MC infiltration (58% vs. 40%, P = 0.023) and a higher median serum tryptase level (448 vs. 199 µg/L, P = 0.018). No significant differences were observed regarding median time from diagnosis (2.2 vs. 2.6 years, P = 0.821) and median time from start of treatment (0.8 vs. 1.5 years, P = 0.186; Table 1, Appendix Table 2).
Evaluation of on-treatment and outcome parameters
According to modified Valent criteria, the overall response rate (ORR) on cladribine in 46/79 (58%) evaluable patients was 18/46 (39%) with a complete remission (CR) in 0/46, a major remission (MR) in 10/46 (22%), and a partial remission (PR) in 8/46 (17%) patients. Comparisons between the patient cohorts with and without available response assessment revealed balanced subgroups (Appendix Table 1). There was no difference between 1L- (12/29, 41%) and 2L-treatment (6/17, 35%; P = 0.690). Any response (MR + PR) vs. no response was associated with improved median OS (3.4 vs. 1.5 years, P = 0.021; Fig. 1A) and was independent of 1L- (3.5 vs. 1.5 years, P = 0.060) or 2L- (3.2 vs. 1.2 years, P = 0.023) treatment (Figs. 1B-C). The use of ≥ 3 cycles was associated with an improved ORR (14/25, 56% vs. 4/21, 19% responder; P = 0.011) and median OS (2.8 vs. 1.2 years, P = 0.038). The median OS (1.9 vs. 1.2 years, P = 0.311) was not different between 1L- and 2L-treatment (Fig. 2A, Table 1).
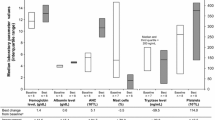
The median percentage change from baseline to response assessment of serum tryptase, BM MC infiltration and KIT D816V EAB was -29% (range -97% to 75%), 11% (range -94% to 233%) and -1% (range -100% to 1669%; Fig. 3), respectively. The median percentage change was significantly higher in responders vs. non-responders according to modified Valent criteria (serum tryptase -46% vs. -28%, BM MC infiltration -50% vs. 0% and KIT D816V EAB -41% vs. 0%; P < 0.05).
Risk stratification according to recently established prognostic scoring systems
MARS [7] and the IPSM-AdvSM [34] were recently validated for up-front midostaurin risk-stratification [23]. Both risk scores were assessed for stratification at time of diagnosis (all patients) and at time of initiation of 1L- or 2L-treatment. At diagnosis, median OS according to MARS (n = 69 evaluable) was 1.5, 2.1, and 1.9 years in low- (n = 16, 23%), intermediate- (n = 11, 16%) and high-risk patients (n = 42, 61%, P = 0.270), respectively. Median OS according to IPSM-AdvSM (n = 71 evaluable) was 1.3, 2.5, and 1.2 years in AdvSM-1/2 (n = 16, 23%), AdvSM-3 (n = 36, 50%), and AdvSM-4 patients (n = 19, 27%, P = 0.053; Fig. 2B-C), respectively. Data were not different when applied at start of 1L- (P = 0.592, P = 0.769) or 2L-treatment (P = 0.125, P = 0.054). Of note, neither MAPS (P = 0.358) nor GPSM (P = 0.127) were able to predict OS on cladribine (Appendix Figure 1).
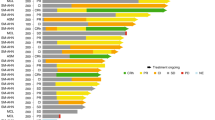
Univariate and multivariable analyses
Univariate and multivariable analyses of baseline parameters from all 79 patients identified diagnosis of MCL (hazard ratio [HR] 3.5, 95% confidence interval [CI, 1.3–9.1], P = 0.012), eosinophilia ≥ 1.5 × 109/L (HR 2.9 [CI 1.4–6.2], P = 0.006) and application of < 3 cycles cladribine (HR 0.4 [CI 0.2–0.8], P = 0.008) as independent adverse prognostic parameters for OS (Figs. 4 and 5, Appendix Figure 2, Appendix Table 3). Outcome on cladribine was independent of the presence of one or more additional somatic mutations in the S/A/R gene panel (HR 0.6 [CI 0.2–2.0], P = 0.412). In univariate analysis, modified Valent criteria were superior (HR 2.9 [CI 1.3–6.6], P = 0.026; Fig. 6; Appendix Table 4) to a single factor-based on-treatment response assessment, e.g. BM MC infiltration, serum tryptase or KIT D816V EAB.
Univariate and multivariable analysis of baseline parameters (entire cohort). Abbreviations: Eos, eosinophils; CMML chronic myelomonocytic leukemia; Hb, hemoglobin; HES/CEL, hypereosinophilic syndrome/chronic eosinophilic leukemia; MC, mast cell; MCL, mast cell leukemia; MDS/MPNu, myelodysplastic/myeloproliferative neoplasms unclassifiable; Plt, platelets; S/A/R, SRSF2/ASXL1/RUNX1; Wbc, white blood cells
Univariate analysis of on-treatment parameters. *Cheson criteria for transfusion were considered if necessary. #or normalization. Abbreviations: AP, alkaline phosphatase; BM, Bone marrow; CI, confidence interval; Eos, eosinophilia; Hb, hemoglobin; MC, mast cell; Mono, monocytosis; N, normalization; HR, Hazard ratio; MC, mast cell; Plt, platelets; R, response
Discussion
In historical cohorts of up to a maximum of 32 AdvSM patients [18, 19, 21], the ORR on cladribine according to (modified) Valent criteria [21, 36] ranged between 50 and 100%. [20] Further interpretation on the impact of treatment with cladribine on progression-free (PFS), relapse-free (RFS), event-free (EFS), leukemia-free (LFS) and overall survival is limited because (i) most reports did not clearly differentiate between ISM and AdvSM, (ii) no report separated between 1L- and 2L-treatment and (iii) the definitions of PFS/RFS/EFS/LFS were not consistent between studies. In a registry-based cross-assessment, we recently reported an ORR (modified Valent criteria) of 35% in midostaurin-treated and 40% in cladribine-treated patients [23]. Notwithstanding, the OS on cladribine was significantly inferior to midostaurin in both 1L- and 2L-treatment cohorts. In the current report, we sought to provide a more detailed analysis on response rates on cladribine in 1L- and 2L-treatment, biomarkers indicating response and resistance and the association between ORR and OS.
Multivariable analysis identified hypereosinophilia (> 1.5 × 109/l), as marker of an AHN, diagnosis of MCL, and application < 3 cycles as adverse prognostic markers. This confirms a recent report from the Mayo Clinic registry on 22 cladribine-treated AdvSM patients indicating a diagnosis of an AHN (in addition to older age and absence of KIT D816V) as adverse prognostic markers for survival and is also in line with a previous publication on the poor prognostic impact of eosinophilia in SM [18, 37]. Recent data also revealed that midostaurin was superior to cladribine in controlling AHN-associated myeloproliferation [23]. The application of ≥ 3 cycles was further associated with a higher ORR.
In a minority of patients (< 10%), cladribine was used for bridging the interval to the start of the midostaurin trial in 2009 and at later time points, it was used in a few patients for more rapid MC debulking with subsequent pre-planned switch to midostaurin. Although myelosuppression became apparent in approximately 20% of patients, infectious complications were not noted as reasons for treatment discontinuation. In contrast to midostaurin, OS on cladribine was not influenced by cytopenias prior to treatment or additional somatic mutations in the S/A/R gene panel. Consequently, none of the prognostic scoring systems (MARS, IPSM, MAPS, GPSM) was predictive for OS. The reasons for this observation are unknown but may be explained at least in part by the fact that the scores more effectively identify low-risk patients on targeted treatment with midostaurin [23, 27] or avapritinb [26] than on conventional chemotherapy with cladribine.
In contrast to the recent report from the Mayo Clinic, possibly due to the higher number of patients in our study, any response according to modified Valent criteria in 1L- but also 2L-treatment was associated with improved OS, thus confirming the usefulness of response assessment for guiding further treatment strategies. The data were underscored by the predictive superiority of modified Valent criteria versus a single factor-based response assessment. Although 2L patients presented with a higher disease burden, response and survival were not statistically different from 1L patients.
Recently reported propensity score weighted analyses on LFS/EFS and OS revealed superiority of midostaurin over cladribine and of avapritinib over best available treatment including midostaurin and cladribine [23,24,25]. However, we conclude that (i) cladribine remains a relevant option within the AdvSM treatment algorithm; its application in 1L-, 2L- or 3L-line locally depends on the approval status and availability of midostaurin and avapritinib; (ii) mast cell leukemia, eosinophilia, application of < 3 cycles and lack of response according to modified Valent criteria are adverse prognostic markers, and (iii) commonly used prognostic models for AdvSM are of limited value because of high mortality in low- and intermediate-risk patients.
The genetic and clinical complexity of AdvSM requires further prospective clinical trials to study the effects of KIT inhibitors in combination with simultaneous or intermittent use of other anti-neoplastic drugs, e.g. cladribine or hypomethylating agents. Such an approach may counteract the potential outgrowth of KIT D816V negative or multimutated subclones [38]. For patients with progression into secondary MCL or secondary AML, AML-like chemotherapy with or without subsequent allogeneic stem cell transplantation remains the most reasonable and potentially curative treatment options.
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author (A.R.) on reasonable request.
References
Valent P, Akin C, Metcalfe DD (2017) Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood 129(11):1420–1427
Valent P, Akin C, Escribano L et al (2007) Standards and standardization in mastocytosis: consensus statements on diagnostics, treatment recommendations and response criteria. Eur J Clin Invest 37(6):435–453
Valent P, Akin C, Sperr WR et al (2003) Diagnosis and treatment of systemic mastocytosis: state of the art. Br J Haematol 122(5):695–717
Pardanani A (2021) Systemic mastocytosis in adults: 2021 Update on diagnosis, risk stratification and management. Am J Hematol 96(4):508–525
Chatterjee A, Ghosh J, Kapur R (2015) Mastocytosis: a mutated KIT receptor induced myeloproliferative disorder. Oncotarget 6(21):18250–18264
Jawhar M, Schwaab J, Schnittger S et al (2015) Molecular profiling of myeloid progenitor cells in multi-mutated advanced systemic mastocytosis identifies KIT D816V as a distinct and late event. Leukemia 29(5):1115–1122
Jawhar M, Schwaab J, Alvarez-Twose I et al (2019) MARS: mutation-adjusted risk score for advanced systemic mastocytosis. J Clin Oncol 37(31):2846–2856
Jawhar M, Schwaab J, Schnittger S et al (2016) Additional mutations in SRSF2, ASXL1 and/or RUNX1 identify a high-risk group of patients with KIT D816V(+) advanced systemic mastocytosis. Leukemia 30(1):136–143
Jawhar M, Schwaab J, Hausmann D et al (2016) Splenomegaly, elevated alkaline phosphatase and mutations in the SRSF2/ASXL1/RUNX1 gene panel are strong adverse prognostic markers in patients with systemic mastocytosis. Leukemia 30(12):2342–2350
Schwaab J, Schnittger S, Sotlar K et al (2013) Comprehensive mutational profiling in advanced systemic mastocytosis. Blood 122(14):2460–2466
Muñoz-González JI, Álvarez-Twose I, Jara-Acevedo M et al (2021) Proposed global prognostic score for systemic mastocytosis: a retrospective prognostic modelling study. Lancet Haematol 8(3):e194–e204
Pardanani A, Shah S, Mannelli F et al (2018) Mayo alliance prognostic system for mastocytosis: clinical and hybrid clinical-molecular models. Blood Adv 2(21):2964–2972
DeAngelo DJ, George TI, Linder A et al (2018) Efficacy and safety of midostaurin in patients with advanced systemic mastocytosis: 10-year median follow-up of a phase II trial. Leukemia 32(2):470–478
Gotlib J, Kluin-Nelemans HC, George TI et al (2016) Efficacy and safety of midostaurin in advanced systemic mastocytosis. N Engl J Med 374(26):2530–2541
Chandesris MO, Damaj G, Canioni D et al (2016) Midostaurin in advanced systemic mastocytosis. N Engl J Med 374(26):2605–2607
DeAngelo DJ, Radia DH, George TI et al (2021) Safety and efficacy of avapritinib in advanced systemic mastocytosis: the phase 1 EXPLORER trial. Nat Med 27(12):2183–2191
Gotlib J, Reiter A, Radia DH et al (2021) Efficacy and safety of avapritinib in advanced systemic mastocytosis: interim analysis of the phase 2 PATHFINDER trial. Nat Med 27(12):2192–2199
Tefferi A, Kittur J, Farrukh F et al (2021) Cladribine therapy for advanced and indolent systemic mastocytosis: Mayo Clinic experience in 42 consecutive cases. Br J Haematol 196(4):975–983
Barete S, Lortholary O, Damaj G et al (2015) Long-term efficacy and safety of cladribine (2-CdA) in adult patients with mastocytosis. Blood 126(8):1009–1016
Kluin-Nelemans HC, Oldhoff JM, Van Doormaal JJ et al (2003) Cladribine therapy for systemic mastocytosis. Blood 102(13):4270–4276
Lim KH, Pardanani A, Butterfield JH, Li CY, Tefferi A (2009) Cytoreductive therapy in 108 adults with systemic mastocytosis: Outcome analysis and response prediction during treatment with interferon-alpha, hydroxyurea, imatinib mesylate or 2-chlorodeoxyadenosine. Am J Hematol 84(12):790–794
Jawhar M, Schwaab J, Meggendorfer M et al (2017) The clinical and molecular diversity of mast cell leukemia with or without associated hematologic neoplasm. Haematologica 102(6):1035–1043
Lübke J, Schwaab J, Naumann N et al (2022) Superior efficacy of midostaurin over cladribine in advanced systemic mastocytosis: a registry-based analysis. J Clin Oncol 40(16):1783–1794
Pilkington H, Smith S, Roskell N, Iannazzo S (2022) Indirect treatment comparisons of avapritinib versus midostaurin for patients with advanced systemic mastocytosis. Future Oncol 18(13):1583–1594
Reiter A, Gotlib J, Álvarez-Twose I et al (2022) Efficacy of avapritinib versus best available therapy in the treatment of advanced systemic mastocytosis. Leukemia 36(8):2108–2120
Reiter A, Schwaab J, DeAngelo DJ et al (2022) Efficacy and safety of avapritinib in previously treated patients with advanced systemic mastocytosis. Blood Adv 6(21):5750–5762
Jawhar M, Schwaab J, Naumann N et al (2017) Response and progression on midostaurin in advanced systemic mastocytosis: KIT D816V and other molecular markers. Blood 130(2):137–145
Lübke J, Naumann N, Kluger S et al (2019) Inhibitory effects of midostaurin and avapritinib on myeloid progenitors derived from patients with KIT D816V positive advanced systemic mastocytosis. Leukemia 33(5):1195–1205
Valent P, Horny HP, Escribano L et al (2001) Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res 25(7):603–625
Reiter A, George TI, Gotlib J (2020) New developments in diagnosis, prognostication, and treatment of advanced systemic mastocytosis. Blood 135(16):1365–1376
Khoury JD, Solary E, Abla O et al (2022) he 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia 36(7):1703–1719
Jawhar M, Schwaab J, Horny HP et al (2016) Impact of centralized evaluation of bone marrow histology in systemic mastocytosis. Eur J Clin Invest 46(5):392–397
Erben P, Schwaab J, Metzgeroth G et al (2014) The KIT D816V expressed allele burden for diagnosis and disease monitoring of systemic mastocytosis. Ann Hematol 93(1):81–88
Sperr WR, Kundi M, Alvarez-Twose I et al (2019) International prognostic scoring system for mastocytosis (IPSM): a retrospective cohort study. Lancet Haematol 6(12):e638–e649
Naumann N, Lübke J, Baumann S et al (2021) Adverse prognostic impact of the KIT D816V transcriptional activity in advanced systemic mastocytosis. Int J Mol Sci 22(5):2562
Valent P, Akin C, Sperr WR et al (2003) Aggressive systemic mastocytosis and related mast cell disorders: current treatment options and proposed response criteria. Leuk Res 27(7):635–641
Kluin-Nelemans HC, Reiter A, Illerhaus A et al (2019) Prognostic impact of eosinophils in mastocytosis: analysis of 2350 patients collected in the ECNM Registry. Leukemia 34(4):1090–1101
Jawhar M, Dohner K, Kreil S et al (2019) KIT D816 mutated/CBF-negative acute myeloid leukemia: a poor-risk subtype associated with systemic mastocytosis. Leukemia 33(5):1124–1134
Acknowledgements
This work was supported by the ´Deutsche José Carreras Leukämie-Stiftung` (grant no. DJCLS 08R/2020). P.V. was supported by the Austrian Science Fund (FWF) grant SFB F4704-B20.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conception and design: JL, AR, JS
Financial support: JS, AR
Administrative support: WKH, AR, JS
Provision of study materials or patients: JL, NN, GM, SK, AF, WKH, AR, JS
Collection and assembly of data: JL
Data analysis and interpretation: JL
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
Corresponding author
Ethics declarations
Research involving human participants
The study design adhered to the tenets of the Declaration of Helsinki and was approved by the institutional review board of the Medical Faculty of Mannheim, Heidelberg University, Germany.
Informed consent
Written informed consent was provided by all patients.
Disclosure of potential conflicts of interest
Disclosures of conflict of interest: H.-P.H. served as a consultant for Novartis and Blueprint. P.V. received a research grant from Blueprint and Celgene, served as a consultant in a midostaurin trial with Novartis, and received consultancy honoraria from Blueprint, Deciphera, Novartis, Celgene and Pfizer. A.R. was a member of the Study Steering Committee (SSC) for the global trial of midostaurin in advanced systemic mastocytosis (AdvSM) (Novartis), the Response Adjudication Committee (RAC) for studies of avapritinib in AdvSM (Blueprint Medicines), and the SSC for the phase II trial of ripretinib in AdvSM (Deciphera Pharmaceuticals); has received funding for the conduct of these trials; and has received honoraria and reimbursement of travel expenses from Novartis, Blueprint Medicines and Deciphera Pharmaceuticals. J.S. has served as a member in the advisory board of Blueprint for studies of avapritinib in indolent SM and received honoraria from Novartis.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lübke, J., Naumann, N., Metzgeroth, G. et al. Response and resistance to cladribine in patients with advanced systemic mastocytosis: a registry-based analysis. Ann Hematol 102, 2077–2085 (2023). https://doi.org/10.1007/s00277-023-05180-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05180-y