Abstract
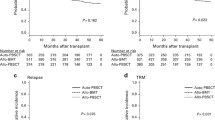
Bone marrow (BM) and granulocyte colony-stimulating factor-mobilized peripheral blood stem cells (PBSC) are used as grafts from HLA-identical-related donors for adults with myelodysplastic syndrome (MDS). To assess the impact of graft sources on post-transplant outcomes in MDS patients, we conducted a retrospective analysis of a nationwide database. A total of 247 and 280 patients underwent transplantation with BM and PBSC, respectively. The inverse probability of treatment weighting (IPTW) methods revealed that overall survival (OS) was comparable between BM and PBSC (P = .129), but PBSC transplantation was associated with worse graft-versus-host disease (GVHD)-free/relapse-free survival (GRFS) (hazard rate [HR], 1.24; 95% confidence intervals [CIs], 1.00–1.53; P = 0.049) and chronic GVHD-free and relapse-free survival (CRFS) (HR, 1.29; 95% CIs, 1.13–1.73; P = 0.002) than BM transplantation. In the propensity score matched cohort (BM, n = 216; PBSC, n = 216), no significant differences were observed in OS and relapse; 3-year OS rates were 64.7% and 60.0% (P = 0.107), while 3-year relapse rates were 27.1% and 23.5% (P = 0.255) in BM and PBSC, respectively. Three-year GRFS rates (36.6% vs. 29.2%; P = 0.006), CRFS rate (37.7% vs. 32.5%; P = 0.003), and non-relapse mortality rates (13.9% vs. 21.1%; P = 0.020) were better in BM than in PBSC. The present study showed that BM transplantation provides a comparable survival benefit with PBSC transplantation and did not identify an enhanced graft-versus-MDS effect to reduce the incidence of relapse in PBSC transplantation.



Similar content being viewed by others
References
Bensinger W, Martin P, Storer B, Clift R, Forman S, Negrin R et al (2001) Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers. N Engl J Med 344(3):175–181
Powles R, Mehta J, Kulkarni S, Treleaven J, Millar B, Marsden J et al (2000) Allogeneic blood and bone-marrow stem-cell transplantation in haematological malignant diseases: a randomised trial. Lancet 355(9211):1231–1237
Heldal D, Tjønnfjord G, Brinch L, Albrechtsen D, Egeland T, Steen R et al (2000) A randomised study of allogeneic transplantation with stem cells from blood or bone marrow. Bone Marrow Transplant 25(11):1129–1136
Blaise D, Kuentz M, Fortanier C, Bourhis J, Milpied N, Sutton L et al (2000) Randomized trial of bone marrow versus lenograstim-primed blood cell allogeneic transplantation in patients with early-stage leukemia: a report from the Société Française de Greffe de Moelle. J Clin Oncol 18(3):537–546
Couban S, Simpson D, Barnett M, Bredeson C, Hubesch L, Howson-Jan K et al (2002) A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 100(5):1525–1531
Morton J, Hutchins C, Durrant S (2001) Granulocyte-colony-stimulating factor (G-CSF)-primed allogeneic bone marrow: significantly less graft-versus-host disease and comparable engraftment to G-CSF-mobilized peripheral blood stem cells. Blood 98(12):3186–3191
Vigorito A, Azevedo W, Marques J, Azevedo A, Eid K, Aranha F et al (1998) A randomised, prospective comparison of allogeneic bone marrow and peripheral blood progenitor cell transplantation in the treatment of haematological malignancies. Bone Marrow Transplant 22(12):1145–1151
Stem Cell Trialists' Collaborative Group (2005) Allogeneic peripheral blood stem-cell compared with bone marrow transplantation in the management of hematologic malignancies: an individual patient data meta-analysis of nine randomized trials. J Clin Oncol 23(22):5074–5087
Tefferi A, Vardiman JW (2009) Myelodysplastic syndromes. N Engl J Med 361(19):1872–1885
Khoury J, Solary E, Abla O et al (2022) The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia 36(7):1703–1719
Arber D, Orazi A, Hasserjian R et al (2022) International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood 140(11):1200–1228
Robin M, Porcher R, Zinke-Cerwenka W, van Biezen A, Volin L, Mufti G et al (2017) Allogeneic haematopoietic stem cell transplant in patients with lower risk myelodysplastic syndrome: a retrospective analysis on behalf of the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transplant 52(2):209–215
Lim Z, Brand R, Martino R, Biezen A, Finke J, Bacigalupo A et al (2009) Allogeneic hematopoietic stem-cell transplantation for patients 50 years or older with myelodysplastic syndromes or secondary acute myeloid leukemia. J Clin Oncol 28(3):405–411
Koreth J, Pidala J, Perez W, Deeg H, Garcia-Manero G, Malcovati L et al (2013) Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: an international collaborative decision analysis. J Clin Oncol 31(21):2662–2670
DeFilipp Z, Ciurea SO, Cutler C et al (2022) Hematopoietic cell transplantation in the management of myelodysplastic syndrome: an evidence-based review from the American Society for Transplantation and Cellular Therapy Committee on practice guidelines. Transplant Cell Ther. https://doi.org/10.1016/j.jtct.2022.11.014
Ishiyama K, Aoki J, Itonaga H et al (2019) Graft-versus-MDS effect after unrelated cord blood transplantation: a retrospective analysis of 752 patients registered at the Japanese Data Center for hematopoietic cell transplantation. Blood Cancer J 9(3):31
Itonaga H, Ishiyama K, Aoki K et al (2019) Increased opportunity for prolonged survival after allogeneic hematopoietic stem cell transplantation in patients aged 60-69 years with myelodysplastic syndrome. Ann Hematol 98(6):1367–1381
Konuma T, Itonaga H, Ishiyama K et al (2023) Progress in survival following three decades of allogeneic hematopoietic cell transplantation for myelodysplastic syndrome: a real-world registry study in Japan. Am J Hematol. https://doi.org/10.1002/ajh.26839
Phelan R, Arora M, Chen M. Current use and outcome of hematopoietic stem cell transplantation: CIBMTR US summary slides, 2020. https://www.cibmtr.org/ReferenceCenter/SlidesReports/SummarySlides/pages/index.aspx.
Rowley S, Donaldson G, Lilleby K, Bensinger W, Appelbaum F (2001) Experiences of donors enrolled in a randomized study of allogeneic bone marrow or peripheral blood stem cell transplantation. Blood 97(9):2541–2548
Cornelissen J, Holt B, Petersen E, Vindelov L, Russel C, Höglund M et al (2003) A randomized multicenter comparison of CD34(+)-selected progenitor cells from blood vs from bone marrow in recipients of HLA-identical allogeneic transplants for hematological malignancies. Exp Hematol 31(10):855–864
Anasetti C, Logan B, Lee S, Waller E, Weisdorf D, Wingard J et al (2012) Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med 367(16):1487–1496
Porta D, Alessandrino E, Bacigalupo A et al (2014) Predictive factors for the outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood 123(15):2333–2342
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K et al (2017) Genetic abnormalities in myelodysplasia and secondary acute myeloid leukemia: impact on outcome of stem cell transplantation. Blood 129(17):2347–2358
Nazha A, Hu ZH, Wang T et al (2020) A personalized prediction model for outcomes after allogeneic hematopoietic cell transplant in patients with myelodysplastic syndromes. Biol Blood Marrow Transplant 26(11):2139–2146
Montalban-Bravo G, Kanagal-Shamanna R, Sasaki K et al (2019) NPM1 mutations define a specific subgroup of MDS and MDS/MPN patients with favorable outcomes with intensive chemotherapy. Blood Adv 26(3):922–933
Itonaga H, Ishiyama K, Aoki K, Aoki J, Ishikawa T, Ohashi K et al (2019) Clinical impact of the loss of chromosome 7q on outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 54(9):1471–1481
Duncavage EJ, Jacoby MA, Chang GS et al (2018) Mutation clearance after transplantation for myelodysplastic syndrome. N Engl J Med 379(11):1028–1041
Atsuta Y (2016) Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol 103(1):3–10
Kanda J (2016) Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol 103(1):11–19
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A et al (2007) Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol 86(3):269–274
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al (1982) Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 51(2):189–199
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89(6):2079–2088
Itonaga H, Aoki K, Aoki J et al (2018) Prognostic impact of donor source on allogeneic hematopoietic stem cell transplantation outcomes in adults with chronic myelomonocytic leukemia: a nationwide retrospective analysis in Japan. Biol Blood Marrow Transplant 24(4):840–848
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al (2009) Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 15(3):367–369
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V et al (2009) Defining the intensity of conditioning regimens: working definitions. Biol Bone Marrow Transplant 15(12):1628–1633
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al (1995) 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 15(6):825–828
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S et al (1991) Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol 28(3):250–259
Aoki K, Ishikawa T, Ishiyama K, Aoki J, Itonaga H, Fukuda T et al (2015) Allogeneic haematopoietic cell transplantation with reduced-intensity conditioning for elderly patients with advanced myelodysplastic syndromes: a nationwide study. Br J Haematol 168(3):463–466
Saber W, Cutler CS, Nakamura R, Zhang MJ, Atallah E, Rizzo JD et al (2013) Impact of donor source on hematopoietic cell transplantation outcomes for patients with myelodysplastic syndromes (MDS). Blood 122(11):1974–1982
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG et al (2015) Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood 125(8):1333–1338
Solh M, Zhang X, Connor K, Brown S, Solomon SR, Morris LE et al (2016) Factors predicting graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation: multivariable analysis from a single center. Biol Blood Marrow Transplant 22(8):1403–1409
Mehta R, Holtan S, Wang T et al (2020) Composite GRFS and CRFS outcomes after adult alternative donor HCT. J Clin Oncol 38(18):2062–2076
Mehta RS, Holtan SG, Wang T et al (2019) GRFS and CRFS in alternative donor hematopoietic cell transplantation for pediatric patients with acute leukemia. Blood Adv 3(9):1441–1449
D’Agostino RB (1998) Propensity score methods for bias reduction in the comparison of a treatment to a nonrandomized control group. Statist Med 17(19):2265–2281
Sorror M, Maris M, Storb R, Baron F, Sandmaier B, Maloney D et al (2005) Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106(8):2912–2919
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48(3):452–458
Gooley TA, Leisenring W, Crowley J, Storer BE (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18(6):695–706
Fine JP, Gray RJ (1999) A proportional hazards model for subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Brunstein C, DeFor T, Lazaryan A, Bejanyan N, Arora M, Brunstein C et al (2015) Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood 125(8):1333–1338
Nakasone H, Kawamura K, Yakushijin K et al (2019) BM is preferred over PBSCs in transplantation from an HLA-matched related female donor to a male recipient. Blood Adv 3(11):1750–1760
Bacigalupo A, Socié G, Schrezenmeier H, Tichelli A, Locasciulli A, Fuehrer M et al (2012) Bone marrow versus peripheral blood as the stem cell source for sibling transplants in acquired aplastic anemia: survival advantage for bone marrow in all age groups. Haematologica 97(8):1142–1148
Ratanatharathorn V, Nash R, Przepiorka D, Devine S, Klein J, Weisdorf D et al (1998) Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood 92(7):2303–2314
Shingaki S, Tsukada N, Ikeda M, Suzuki K (2018) Graft-versus-host disease-free, relapse-free survival after HLA-identical sibling peripheral blood stem cell transplantation with tacrolimus-based graft-versus-host disease prophylaxis in Japanese patients. Transplant Proc 50(1):241–245
Chen G, Paplham P, McCarthy P (2014) Remestemcel-L for acute graft-versus-host disease therapy. Expert Opin Biol Ther 14(2):261–269
Muroi K, Miyamura K, Okada M, Yamashita T, Murata M, Ishikawa T et al (2016) Bone marrow-derived mesenchymal stem cells (JR-031) for steroid-refractory grade III or IV acute graft-versus-host disease: a phase II/III study. Int J Hematol 103(2):243–250
Fuji S, Hirakawa T, Takano K et al (2022) Disease-specific impact of anti-thymocyte globulin in allogeneic hematopoietic cell transplantation: a nationwide retrospective study on behalf of the JSTCT, transplant complications working group. Bone Marrow Transplant 57(3):479–486
Hiramoto N, Kurosawa S, Tajima K, Okinaka K, Tada K, Kobayashi Y et al (2014) Positive impact of chronic graft-versus-host disease on the outcome of patients with de novo myelodysplastic syndrome after allogeneic hematopoietic cell transplantation: a single-center analysis of 115 patients. Eur J Haematol 92(2):137–146
Baron F, Maris M, Sandmaier B, Storer B, Sorror M, Diaconescu R et al (2005) Graft-versus-tumor effects after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. J Clin Oncol 23(9):1993–2003
Horowitz M, Gale R, Sondel P, Goldman J, Kersey J, Kolb H et al (1990) Graft-versus-leukemia reactions after bone marrow transplantation. Blood. 75(3):555–562
Sullivan K, Weiden P, Storb R, Witherspoon R, Fefer A, Fisher L et al (1989) Influence of acute and chronic graft-versus-host disease on relapse and survival after bone marrow transplantation from HLA-identical siblings as treatment of acute and chronic leukemia. Blood 73(6):1720–1728
Valcárcel D, Martino R, Caballero D, Martin J, Ferra C, Nieto J et al (2008) Sustained remissions of high-risk acute myeloid leukemia and myelodysplastic syndrome after reduced-intensity conditioning allogeneic hematopoietic transplantation: chronic graft-versus-host disease is the strongest factor improving survival. J Clin Oncol 26(4):577–584
Kanda Y, Izutsu K, Hirai H, Sakamaki H, Iseki T, Kodera Y et al (2004) Effect of graft-versus-host disease on the outcome of bone marrow transplantation from an HLA-identical sibling donor using GVHD prophylaxis with cyclosporin A and methotrexate. Leukemia 18(5):1013–1019
Itonaga-H KM, Hamamura A et al (2022) Outcome of therapy-related myelodysplastic syndrome and oligoblastic acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation: a propensity score matched analysis. Hematol Oncol 40(4):752–762
Witte T, Bowen D, Robin M et al (2017) Allogeneic hematopoietic stem cell transplantation for MDS and CMML: recommendations from an international expert panel. Blood 129(13):1753–1762
Della Porta MG, Gallì A, Bacigalupo A, Zibellini S, Bernardi M, Rizzo E et al (2016) Clinical effects of driver somatic mutations on the outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem-cell transplantation. J Clin Oncol 34(30):3627–3637
Bejar R, Stevenson KE, Caughey B, Lindsley RC, Mar BG, Stojanov P et al (2014) Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem cell transplantation. J Clin Oncol 32(25):2691–2698
Bredeson C, Leger C, Couban S, Simpson D, Huebsch L, Walker I et al (2004) An evaluation of the donor experience in the Canadian multicenter randomized trial of bone marrow versus peripheral blood allografting. Biol Blood Marrow Transplant 10(6):405–414
Favre G, Beksaç M, Bacigalupo A, Ruutu T, Nagler A, Gluckman E et al (2003) Differences between graft product and donor side effects following bone marrow or stem cell donation. Bone Marrow Transplant 32(9):873–880
Miller J, Perry E, Price T, Bolan C, Karanes C, Boyd T et al (2008) Recovery and safety profiles of marrow and PBSC donors: experience of the National Marrow Donor Program. Biol Blood Marrow Transplant 14(9):29–36
Clausen J, Kircher B, Auberger J et al (2012) Bone marrow may be the preferable graft source in recipients homozygous for HLA-C group 2 ligands for inhibitory killer Ig-like receptors. Bone Marrow Transplant 47(6):791–798
Acknowledgements
This work was supported in part by the Takeda Science Foundation.
The authors would like to thank all the physicians and data managers at the various institutes who contributed valuable data on transplantation to the Japanese Society for Transplantation and Cellular Therapy (JSTCT), all the members of the data management committees of JSTCT, and all the members of the “Adult Myelodysplastic Syndromes Working Group of the JSTCT.”
Author information
Authors and Affiliations
Contributions
H.I. and Y.M. designed the research, organized the project, analyzed the data, and wrote the manuscript. H.I., Y.M., and K.I. collected data from TRUMP. H.I., Y.M., K.A., N.S., Y.O., T.F., K.K., T.K., Y.U., T.A., M.T., Y.K., M.S., T.E., J.K., Y.A., and K.I. interpreted data and reviewed and approved the final manuscript.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplemental information
ESM 1:
Figure S1. Transplant outcomes in the entire subset. (A) The 3-year probabilities of overall survival (OS) were 66.1% (95% CI, 59.6-71.8%) and 57.6% (95% CI, 51.4-63.2%) in the bone marrow (BM) and peripheral blood stem cell (PBSC) groups, respectively. (B) The 3-year probabilities of graft-versus-host disease (GVHD)-free and relapse-free survival (GRFS) were 38.3% (95% CI, 32.1-44.5%) and 28.4% (95% CI, 23.1-33.9%) in the BM and PBSC groups, respectively. (C) The 3-year probabilities of chronic GVHD-free and relapse-free survival (CRFS) were 40.5% (95% CI, 34.2-46.7%) and 31.2% (95% CI, 25.8-36.8%) in the BM and PBSC groups, respectively. (D) The 3-year cumulative incidences of relapse (CIR) were 23.7% (95% CI, 18.5-29.2%) and 24.7% (95% CI, 19.8-30.0%) in the BM and PBSC groups, respectively. (E) The 3-year non-relapse mortalities (NRM) were 15.2% (95% CI, 10.9-20.1%) and 22.2% (95% CI, 17.5-27.2%) in the BM and PBSC groups, respectively. Figure S2. Histogram of the propensity score distribution in the entire subset. Propensity score distributions represented a better overlap in the post-inverse probability of treatment weighting (IPTW) adjustment (left) than the pre-IPTW adjustment (right). Figure S3. Box-plot of the propensity score distribution in the PSM population. Propensity score distributions represented a better overlap in the post-propensity score matching (PSM) subset (left) than the pre-PSM subset (right). Figure S4. Transplant outcomes in the PSM population. The estimated cumulative incidence curves of neutrophil engraftment (A), platelet recovery (B), acute GVHD development (C), and chronic GVHD development (D). (A) The median times of neutrophil engraftment were days 17 and 14 in the BM and PBSC groups, respectively. The rate of neutrophil engraftment was 90.7% (95% CI, 86.0-93.9%) and 96.3% (95% CI, 92.7-98.1%) at day 28 after HSCT in BM and PBSC groups, respectively; and 95.4% (95% CI, 91.6-97.5%) and 96.3% (95% CI, 92.7-98.1%) at day 100 after HSCT in BM and PBSC groups, respectively. (B) The median times of platelet recovery were days 30 and 24 in the BM and PBSC groups, respectively. The rate of platelet recovery was 71.7% (95% CI, 65.2-77.3%) and 78.6% (95% CI, 72.5-83.5%) at day 45 after HSCT in BM and PBSC groups, respectively; and 78.2% (95% CI, 72.1-83.2%) and 82.7% (95% CI, 77.0-87.2%) at day 100 after HSCT in BM and PBSC groups, respectively. (C) The cumulative incidence of acute GVHD on day 100 were 49.3% (95% CI, 42.5-55.8%) and 58.9% (95% CI, 51.9-65.3%) in the BM and PBSC groups, respectively. (D) The cumulative incidence of chronic GVHD at 3 years were 41.5% (95% CI, 34.4-48.3%) and 55.8% (95% CI, 48.2-62.8%) in the BM and PBSC groups, respectively. Figure S5. A forest plot of transplant outcomes. Hazard ratios (HRs) from the subgroup analysis of NRM (A) and CIR (B) between BM and PBSC transplantation. HRs <1.00 indicate a better outcome after BM transplantation than after PBSC transplantation. (1.07 MB)
ESM 2
49.7 KB
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Itonaga, H., Miyazaki, Y., Aoki, K. et al. Allogeneic transplantation of bone marrow versus peripheral blood stem cells from HLA-identical relatives in patients with myelodysplastic syndromes and oligoblastic acute myeloid leukemia: a propensity score analysis of a nationwide database. Ann Hematol 102, 1215–1227 (2023). https://doi.org/10.1007/s00277-023-05167-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05167-9