Abstract
Chimeric antigen receptor T-cell (CAR-T) therapy targeting CD19 has significantly improved outcomes in the treatment of refractory or relapsed (R/R) B-cell non-Hodgkin lymphoma (NHL). Several risk factors including CAR-T cell-related toxicities and their treatments often lead to infectious complications (ICs); however, the pattern and timeline is not well established. We evaluated ICs in 48 patients with R/R B-cell NHL following CAR-T cell therapy at our institution. Overall, 15 patients experienced 22 infection events. Eight infections (4 bacterial, 3 viral and 1 fungal) occurred within the first 30 days and 14 infections (7 bacterial, 6 viral, 1 fungal) between days 31 to 180 following CAR-T infusion. Most infections were mild-to-moderate and fifteen infections involved the respiratory tract. Two patients developed mild-to-moderate COVID-19 infection and one patient a cytomegalovirus reactivation after CAR-T infusion. Two patients developed IFIs: one case each of fatal disseminated candidiasis and invasive pulmonary aspergillosis at day 16 and 77, respectively. Patients with more than 4 prior antitumor regimens and patient’s ≥ 65 years had a higher infection rate. Infections in patients with relapsed/refractory B-cell NHL are common after CAR-T despite the use of infection prophylaxis. Age ≥ 65 years and having > 4 prior antitumor treatments were identified as risk factors for infection. Fungal infections carried significant impact in morbidity and mortality, suggesting a role for increase fungal surveillance and/or anti-mold prophylaxis following high-dose steroids and tocilizumab. Four of ten patients developed an antibody response following two doses of SARS-CoV-2 mRNA vaccine.
Similar content being viewed by others
Introduction
Chimeric antigen receptor T-cell (CAR-T) therapy is an effective treatment for relapsed and refractory (R/R) b-cell non-Hodgkin lymphoma (NHL) [1-4]. Cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) are well-known complications of CAR-T therapy; however, patients are at risk for significant infections as well. Patients receiving CAR-T cell therapy are typically immunosuppressed due to prior treatments leading to prolonged cytopenias and hypogammaglobinemia followed by exposure to additional lymphodepleting chemotherapy. CRS and ICANS exhibit non-specific clinical manifestations of a hyperinflammatory state, and their differential diagnosis includes, among others, sepsis. The use of high-dose corticosteroids and IL-6 blockers to treat severe CRS/ICANS not only intensifies the risk of infection but can also mask infection-related symptoms such as fever, making the diagnosis of infection more challenging [5]. Severe infections (i.e., grade ≥ 3) have been reported in each of the CAR-T registration studies, with the incidence of infectious complications (ICs) ranging from 8 to 25% [1, 4]. Bacterial complications (e.g., bacteremia, C. difficile gastroenteritis, pneumonia), viral (e.g., respiratory viruses, cytomegalovirus, varicella zoster virus), and fungal infections (e.g., candidemia and invasive molds) have been described, along with a higher burden of ICs occurring within 30 days following CAR-T cell infusion [5]. While data from clinical trials have contributed to the understanding of infection risk, they often lack the granularity provided by single-center studies where the local epidemiology, patients’ characteristics, and treatment practices affect the pattern of ICs related to CAR-T cell therapy.
Herein, we report a single-center retrospective study of IC following CAR-T cell therapy in 48 adult patients with R/R B-cell NHL.
Methods
Patients and data collection
Adult patients (≥ 18 years) with R/R CD19 B-cell malignancies treated with CAR-T cell therapy at the Huntsman Cancer Institute between May 2018 and March 2022 were included. Patients’ electronic medical records were reviewed for patient and disease characteristics, including demographics, laboratory data, ICs early (0–30 days) and late (31–180 days), antimicrobial prophylaxis and treatment courses, prior therapies received, bridging therapy, disease status before CAR-T infusion, CAR-T indications, CAR-T infusion, CAR-T-related toxicities, ICU admission, and death events. Also, pre-infusion (age, sex, type of disease, ECOG, median prior treatments, lymphodepletion, type of CAR-T, Ferritin, lactic acid dehydrogenase, C-reactive protein, and IgG levels) and post-infusion factors (CRS, ICANS, use of steroids, and use of tocilizumab) that could be associated with infections were collected. COVID-19 infections, along with COVID-19 vaccination status and subsequent testing for anti-spike IgG, were captured following the availability of mRNA vaccines in December 2020. Antigen-specific immunoglobulin G (IgG) antibody titers were assessed using fresh plasma samples and direct enzyme-linked immunosorbent assay after 4 weeks receiving at least two COVID-19 vaccines. The Huntsman Cancer Center Institutional Review Board approved this retrospective analysis. Informed consent was obtained from all patients for being included in the study. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2008.
Lymphodepletion chemotherapy and adoptive transfer of CD19-directed CAR-T cells
All patients received lymphodepleting chemotherapy consisting of cyclophosphamide 300–500 mg/m2 and fludarabine 30 mg/m2 on days − 5, − 4, and − 3, followed by single infusion of axicabtagene (n = 20), tisagenlecleucel (n = 13), lisocabtagene (n = 9), and brexucabtagene (n = 6).
Infectious prophylaxis
All patients received standard infectious prophylaxis consisting of levofloxacin and fluconazole from the day of cell infusion until absolute neutrophil count (ANC) recovery above 500 cells/mm3. Acyclovir and anti-Pneumocystis jirovecii (PJP) prophylaxis were given for a minimum of 6 months or until CD4+ lymphocyte count > 200 cells/mm3.
Definition of infection
Bacterial infections were categorized as a bacteremia or a site-specific infection. Repeated positive cultures for the same organism were considered a second event if they occurred ≥ 21 days after the initial event and interval cultures were negative. Site-specific infections were defined by a positive culture of a normally sterile site or by culture and clinical or radiographic evidence of infection in a nonsterile site. Viral infections were defined as upper or lower respiratory tract infections based on the presence of compatible symptoms and a positive viral molecular test, including detection for SARS-CoV-2. Cytomegalovirus (CMV) viremia was defined as any detection of CMV DNA in peripheral blood at any level using our institutional real-time CMV PCR assay independent of the present of compatible CMV viremia symptoms. Invasive fungal infections (IFIs) were classified as proven or probable based on the EORTC/MSG 2019 revised criteria for invasive fungal disease [6]. Infection severity was graded according to CTCAE v5.0 specific to the event of interest. Severe infections (grade ≥ 3) were those that required IV antimicrobial therapy and/or hospitalization or were associated with life-threatening symptoms or invasive interventions, in keeping with previously reported categorizations.
Statistical analysis
Descriptive statistics were used to summarize the clinical data. Categorical data were compared using the chi-square test, whereas, for continuous variables, non-parametric tests were used. Differences among the subgroups of patients were compared by using the chi-square test (two-tailed), Student’s t-test, or non-parametric tests when necessary. Prognostic factors significant (p-value less than 0.05) in the univariate analysis were included in multivariate analyses. Multivariate logistic regression analysis was used to test the association between infection occurrence and putative risk factors.
Results
General characteristics of the series (N = 48)
The cohort included patients with large B-cell lymphoma (LBCL) (n = 38), mantle cell lymphoma (n = 5), transformed LBCL (n = 4), and follicular lymphoma (n = 1). Demographic and clinical characteristics are shown in Table 1. Thirty-eight out of 48 patients (79%) developed any grade of CRS, being 21% of them grade 3 or higher. Twenty-one (44%) developed any grade of ICANs, being 38% grade 3 or higher. The main clinical and biological characteristics are shown in Table 1. Responses after CAR-T infusion at day 30 and relapses are shown in Table 2.
Infectious complications
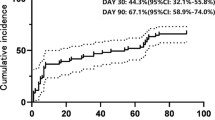
Thirty-seven (77%) patients of all series developed neutropenic fever after CAR-T infusion. Overall, fifteen patients (31%) experienced 22 infection events. Eight infections (36%) (4 bacterial, 3 viral and 1 fungal) occurred within the first 30 days of CAR-T infusion, and 14 infections (64%) (7 bacterial, 6 viral, 1 fungal) between days 31 to 180 following CAR-T infusion (Table 3). Most infections were mild-to-moderate in severity (87%) and did not require intravenous antibiotic therapy or hospital admission. Fifteen infections (68 %) involved the respiratory tract (upper respiratory infection: 10, pneumonia: 5). In general, bacterial and viral infections were detected at a median of 19 and 33 days following CAR-T infusion, respectively. Two patients developed mild-to-moderate COVID-19 infection and one patient had CMV reactivation at days 73, 82, and 49 after CAR-T infusion, respectively. Two patients (3.9%) developed IFIs: one case each of fatal disseminated candidiasis from a fluconazole-resistant Candida glabrata and invasive pulmonary aspergillosis (Aspergillus fumigatus complex) that occurred at day 16 and 77, respectively. Both cases required before the use of high-dose corticosteroids and tocilizumab to treat CRS toxicity grades 2 and 3, respectively. All bacterial, viral, and fungal infections and their pathogens are described in Table 3. Also, we developed a univariate and multivariate analysis with some of the prognostic factors previously reported in the literature and risk of infection as is showed in Table 4. In our series, patients with more than 4 prior antitumor regimens and patient’s ≥ 65 years had a higher infection rate, being age ≥ 65 years the most important factor for infection in the multivariate analysis (see Table 4).
COVID-19 vaccination
We evaluated humoral response to two-dose SARS-CoV-2 mRNA vaccines (BNT162b2 or mRNA-1273) in ten patients who were vaccinated after 90 days of CAR-T cell infusion when COVID-19 vaccine was available in December 2020. In this series, four patients received also tixagevimab plus cilgavimab after CAR-T infusion. At a median of 48 days following the second dose, an anti-Spike IgG was detectable in four (40%) of them.
Conclusions
In this single-center study, we report a high proportion of infectious complications occurring predominantly within the first 30 days following CAR-T cell infusion, with a modest predominance of viral over bacterial infections. Infections of the respiratory tract were the most common; most ICs were mild-to-moderate in severity, not requiring hospitalization or IV antibiotic therapy. Moreover, our uni/multivariate analysis showed age ≥ 65 years and ≥ 4 prior antitumor treatments as the main risk factors for infection.
Our results are in line with previously reported studies. Hill et al. [7] analyzed infectious complications in 133 adult patients in a cohort study including ALL (n = 47), CLL (n = 24), and NHL (n = 62) receiving CAR-T in a phase 1/2 study. In this series, 24% of patients experienced any infection, including 5% fungal and 4% of fatal events. Risk factors identified in this series were ≥ 4 prior treatments, a diagnosis of ALL and receiving a higher dose of CAR-T cells (2 × 107cells/kg). Strati et al. [8] analyzed 31 patients with relapsed/refractory LBCL who underwent CAR-T cell treatment with axicabtagene and were included in the clinical trials ZUMA-1 (NCT02348216) and ZUMA-9 (NCT03153462). Among all 31 patients, 71 infectious events of any grade were reported (42% grade 3–4 infection). Most common infections were viral and 6% of patients developed a fungal infection. Logue et al. [9] conducted a retrospective, single-center study of 85 patients with relapsed/refractory LBCL treated with axicabtagene. In the first 30 days, 36.5% patients presented an infection event, with 12.9% of them requiring IV antibiotics or hospitalization. CRS, ICANS, use of tocilizumab, or steroids and bridging therapy were risk factors for ICs in this series. After day 30, 44.3% of patients had any infection requiring hospitalization or IV antibiotics. Infection was a contributor to death in 3 cases (3.5%) in this series. Cordeiro et al. [10] analyzed a cohort of 86 patients with relapsed/refractory ALL, NHL, and CLL treated with CAR-T infusion included on a phase 1/2 clinical trial. After day 30th, 61% of patients developed any infection, with 71% respiratory tract involvement. Bacterial was the most frequent (60%), 31% viral and 9% fungal etiology. Moreover, 20% of patients in this series required hospitalization.
Baird et al. [11] evaluated hematologic recovery, immune reconstitution, and also infectious complications in 41 patients with NHL treated with axicabtagene ciloleucel. In the first 28 days following infusion, 46.3% patients had an infection, with the majority being mild-to-moderate in severity (68.4%). The most common etiology was viral respiratory tract infections (21.1%). Receipt of corticosteroids was the only factor that predicted risk of infection in a multivariate analysis.
Wudhikarn et al. [12] analyzed 60 patients with LBCL treated with CD19 CAR-T cells and a total of 101 infectious events were observed, being 75% of them mild-to-moderate and bacteria the most common causative pathogens. Thirty-seven percent of them are within the first 30 days. In a multivariate analyses, the use of systemic corticosteroids for the management of CRS or ICANS was associated with an increased risk of infections.
Lastly, a study by Mikkilineni et al. [13] focused on infections occurring within the first 30 days of treatment in 162 CAR-T cell patients who received CAR-T antigen targets (CD19, CD22, D2, and BCMA). The proportion of infectious complications in the first 30 days was 32.7%; greater lines of chemotherapy and a recent infection within 100 days of CAR-T cell infusion were associated with higher risk of infection.
Despite high degree of immunosuppression and prolonged neutropenia, fungal infections have remained infrequent in patients undergoing CAR-T cell therapy. Depending on the study, the incidence of IFI has ranged between 1 and 15%, and most of these infections occur as breakthrough to antifungal prophylaxis [14]. In our series, two patients (3.9%) developed IFIs: one fatal case of disseminated Candidemia due to fluconazole-resistant Candida glabrata (breakthrough fluconazole prophylaxis) and one case of invasive pulmonary aspergillosis. Of note, both patients had received immunosuppression augmentation with tocilizumab and high-dose steroids for high-grade CRS. Several reports have described molds other than Aspergillus, complicating CAR-T cell therapy [15]. Targeted anti-mold prophylaxis has been proposed for individuals with a history of past-fungal infection, severe and prolonged neutropenia (> 3 weeks), previous allogeneic HSCT, and in patients receiving high-dose corticosteroids5. In low-risk patients and/or at treatments centers with low IFI incidence, a preemptive strategy based on biomarkers and imaging screening could be adopted. As the option for CAR-T cell therapy move upstream in the treatment line for several hematological malignancies, the landscape for IFI complications will continue evolving in the upcoming years. Future studies are needed to elucidate specific risk factors for IFI and define the population who benefit the most of anti-mold prophylaxis.
In our case series, the spectrum of clinical syndromes associated with bacterial and viral infections was similar to those previously reported in the literature, with predominance of viral respiratory infections (including COVID-19) and nosocomial infections (see Table 2).
Our study has several limitations. First, it is restricted to a single center and included only patients with relapse/refractory CD19 B-cell NHL. As such, the overall results might not be applicable to centers with different antimicrobial prophylaxis practices or centers that offer CAR-T cell for other than CD19 B-cell NHL. Second, our median time to follow-up was almost 8 months post-CAR-T cell infusion. Hence, infection complications that occurred late in the post-CAR-T cell period might have not been entirely captured in our review. Notably, our study did not link laboratory markers for B-cell aplasia, B-cell dysfunction, or reconstitution of the T-cell compartment with tangible clinical outcomes for infection. Other factors such as CAR-T-cell-related neutropenia, reactivation of latent viral infections (e.g., CMV, HHV-6), and the need for stem-cell reinfusion in refractive cytopenias might play a role in late-onset infection following CAR-T infusion and should be assessed in prospective studies. Lastly, in our series, serological testing to assess immune response to SARS-CoV-2 vaccination was performed inconsistently and at different time points following CAR-T cell infusion. For instance, only 21% of patients had anti-spike IgG titers available to assess immunogenicity following two doses of SARS-CoV-2 mRNA vaccine. Several studies have described suboptimal vaccination responses in patients with hematological malignancies, including CAR-T cell recipients [16-19]. Other markers of vaccine-immune response (e.g., T-cell response) and the effect of vaccine boosters over the augmentation of anti-spike IgG titers were not addressed in this study and may play a substantial role in COVID-19 disease prevention following CAR-T cell therapy. Moreover, the ”real-world” impact of prophylactic strategies using anti-SARS-CoV-2 long-lasting monoclonal antibodies (e.g., tixagevimab plus cilgavimab) remains unknown and deserves further research in this population.
In summary, the reporting of infectious complications from CAR-T cell therapy’s clinical trials has been inconsistent, often lacking details about the nature, timing and course of common infections. In that context, single-center case series like ours contribute to understanding the local epidemiology and to guide antimicrobial prophylaxis strategies. Data from patients’ registries are welcome to delineate national and center-specific CAR-T cell-associated infection rates and define future research targets. In the upcoming years, several factors will continue reshaping the risk for infection following CAR-T cell therapy. The use of CAR-T cells with novel antigen targets (e.g., CAR-T targets NK, anti-BCMA, CD22, disialonganglioside [GD2]) along with the expansion of CAR-T cell indications and its use earlier in the treatment course will inevitably alter the infection risk framework. Research focused on infectious complications CAR-T cells will hopefully provide guidance on adequate standards and extension of antimicrobial prophylaxis in CAR-T cell patients.
References
Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirket JP, Tam CS, Waller EK, Borchmann P, McGuirk JP, Jäger U, Jaglowski S, Andreadis C, Westin JR, Fleury I, Bachanova V, Foley SR, Ho PJ, Mielke S et al (2019) Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med 380(1):45–56. https://doi.org/10.1056/NEJMoa1804980
Neelapu SS, Locke FL, Bartlett LNL, Lekakis J, Miklos DB, Jacobson CA, Braunschweig I, Oluwole OO, Siddiqi T, Lin Y, Timmerman JM, Stiff PJ, Friedberg JW, Flinn IW, Goy A, Hill BT, Smith MR, Deol A, Farooq U et al (2017) Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med 377(26):2531–2554. https://doi.org/10.1056/NEJMoa1707447
Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, Mehta A, Purev E, Maloney DG, Andreadis C, Sehgal A, Solomon SR, Ghosh N, Albertson TM, Garcia J, Kostic A, Mallaney M, Ogasawara K, Newhall K et al (2020) Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet 396(10254):839–852. https://doi.org/10.1016/S0140-6736(20)31366-0
Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, Timmerman JM, Holmes H, Jaglowski S, Flinn IW, McSweeney PA, Miklos DB, Pagel JM, Kersten MJ, Milpied N, Fung H, Topp MS, Houot R, Beitinjaneh A et al (2020) KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med 382(14):1331–1342. https://doi.org/10.1056/NEJMoa1914347
Hill JA, Seo SK (2020) How I prevent infections in patients receiving CD19-targeted chimeric antigen receptor T cells for B-cell malignancies. Blood 136(8):925–935. https://doi.org/10.1182/blood.2019004000
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, Clancy CJ, Wingard JR, Lockhart SR, Groll AH, Sorrell TC, Bassetti M, Akan H, Alexander BD, Andes D, Azoulay E, Bialek R, Bradsher RW, Bretagne S et al (2020) Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 71(6):1367–1376. https://doi.org/10.1093/cid/ciz1008
Hill JA, Li D, Hay KA, Green ML, Cherian S, Chen X, Riddell SR, Maloney DG, Boeckh M, Turtle CJ (2018) Infectious complications of CD19-targeted chimeric antigen receptor–modified T-cell immunotherapy. Blood. 131(1):121–130. https://doi.org/10.1182/blood-2017-07-793760
Strati P, Varma A, Adkins S, Nastoupil LJ, Westin J, Hagemeisteret FB, Fowler NH, Lee HJ, Fayad LE, Samaniego F, Ahmed S, Chen Y, Horowitz S, Arafat S, Johncy S, Kebriaei P, Mulanovich VE, Heredia EA, Neelapu SS (2021) Hematopoietic recovery and immune reconstitution after axicabtagene ciloleucel in patients with large B-cell lymphoma. Haematologica 106(10):2667–2672. https://doi.org/10.3324/haematol.2020.254045
Logue JM, Zucchetti E, Bachmeier CA, Krivenko GS, Larson V, Ninh D, Grillo G, Cao B, Kim J, Chavez JC, Baluch A, Khimani F, Lazaryan A, Nishihori T, Liu HD, Pinilla-Ibarz J, Shah BD, Faramand R, Coghill AE et al (2021) Immune reconstitution and associated infections following axicabtagene ciloleucel in relapsed or refractory large B-cell lymphoma. Haematologica 106(4):978–986. https://doi.org/10.3324/haematol.2019.238634
Cordeiro A, Bezerra ED, Hirayama AV, Hill JA, Wu QV, Voutsinas J, Sorror ML, Turtle CJ, Maloney DG, Bar M (2020) Late events after treatment with CD19-targeted chimeric antigen receptor modified T cells. Biol Blood Marrow Transplant 26:26–33. https://doi.org/10.1016/j.bbmt.2019.08.003
Baird JH, Epstein DJ, Tamaresis JS, Ehlinger Z, Spiegel JY, Craig J, Claire GK, Frank MJ, Muffly L, Shiraz P, Meyer E, Arai S, Brown JW, Johnston L, Lowsky R, Negrin RS, Rezvani AR, Weng WK, Latchford T et al (2021) Immune reconstitution and infectious complications following axicabtagene ciloleucel therapy for large B-cell lymphoma. Blood Adv. 5(1):143–155. https://doi.org/10.1182/bloodadvances.2020002732
Wudhikarn K, Palomba ML, Pennisi M, Garcia-Recio M, Flynn JR, Devlin SM, Afuye A, Silverberg ML, Maloy MA, Shah GL, Scordo M, Dahi PB, Sauter CS, Batlevi CL, Santomasso BD, Mead E, Seo SK, Perales MA (2020) Infection during the first year in patients treated with CD19 CAR T cells for diffuse large B cell lymphoma. Blood Cancer J 10(8):79. https://doi.org/10.1038/s41408-020-00346-7
Mikkilineni L, Yates B, Steinberg SM, Shahani SA, Molina JC, Palmore T, Lee DW, Kaplan RN, Mackall CL, Fry TJ, Gea-Banacloche J, Jerussi T, Nussenblatt V, Kochenderfer JN, Shah NN (2021) Infectious complications of CAR T-cell therapy across novel antigen targets in the first 30 days. Review Blood Adv 5(23):5312–5322. https://doi.org/10.1182/bloodadvances.2021004896
Stewart AG, Henden AS (2021) Infectious complications of CAR T-cell therapy: a clinical update. Review Ther Adv Infect Dis 24(8):20. https://doi.org/10.1177/20499361211036773
Haidar G, Dorritie K, Farah R, Bogdanovich T, Nguyen MH, Palash SP (2020) Invasive mold infections after chimeric antigen receptor-modified T-cell therapy: a case series, review of the literature, and implications for prophylaxis. Clin Infect Dis 71(3):672–676. https://doi.org/10.1093/cid/ciz1127
Monin L, Laing AG, Muñoz-Ruiz M, Del Molino I, Alaguthurai T, Hayday D-VC, TS GC, Seow J, Abdul-Jawad S, Kamdar S, Harvey-Jones E, Graham R, Cooper J, Khan M, Vidler J, Kakkassery H, Sinha S, Davis R, Dupont L et al (2021) Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol 22(6):765–778. https://doi.org/10.1016/S1470-2045(21)00213-8
Ram R, Freund T, Halperin T, Ben-Ami R, Amit O, Bar-On Y, Beyar-Katz O, Eilaty N, Gold R, Kay S, Glait-Santar C, Hagin D (2022) Immunogenicity of a third dose of the BNT162b2 mRNA COVID-19 vaccine in patients with impaired B cell reconstitution after cellular therapy-a single center prospective cohort study. Transplant Cell Ther 28(5):278.e1–278.e4. https://doi.org/10.1016/j.jtct.2022.02.012
Hill JA, Krantz EM, Hay KA, Dasgupta S, Stevens-Ayers T, Bender RA, Bar M, Maalouf J, Cherian S, Chen X, Pepper G, Riddell SR, Maloney DG, Boeckh MJ, Turtle CJ (2019) Durable preservation of antiviral antibodies after CD19-directed chimeric antigen receptor T-cell immunotherapy. Blood Adv 3(22):3590–3601. https://doi.org/10.1182/bloodadvances.2019000717
Bhoj VG, Arhontoulis D, Wertheim G, Capobianchi J, Callahan CA, Ellebrecht CT, Obstfeld AE, Lacey SF, Melenhorst JJ, Nazimuddin F, Hwang WT, Maude SL, Wasik MA, Bagg A, Schuster S, Feldman MD, Porter DL, Grupp SA, June CH, Milone MC (2016) Persistence of long-lived plasma cells and humoral immunity in individuals responding to CD19-directed CAR T-cell therapy. Blood 128(3):360–370. https://doi.org/10.1182/bloodadvances.2019000717
Acknowledgements
The authors thank the staff and faculty of the Marrow Transplantation Program at Huntsman Cancer Institute and University of Utah for tireless work caring for the patients involved in this study.
Author information
Authors and Affiliations
Contributions
S. M. and C. A. G. designed and performed research, analyzed data and wrote the manuscript. D. C. and C. L. reviewed that data and edited the manuscript; all authors approved the final manuscript prior to submission.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
C. J. L. has received honoraria for educational activities and/or consultancy and/or participation in advisory boards from Jazz, Incyte, Fresensius Kabi, BMS, Kite, Kadmon, CareDx; has received research funding from Incyte; and serves on a trial steering committee for Incyte. S. M., C. A. G., and D. R. C. declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mercadal, S., Gomez, C.A., Lee, C.J. et al. Infectious complications following CAR-t cell therapy for B cell non-Hodgkin lymphoma: a single-center experience and review of the literature. Ann Hematol 102, 1837–1843 (2023). https://doi.org/10.1007/s00277-023-05131-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05131-7