Abstract
Acquired aplastic anemia (AA) is a bone marrow failure disorder characterized by pancytopenia, and immunosuppressive therapy (IST) is the optional first-line management. Several studies identified the influencing factors on IST response; however, there are still a considerable number of patients suffering from poor prognoses. In this study, we enrolled 61 AA patients aged ≤ 40 years old, and whole-exome sequencing (WES) found unexpected high FANC heterozygous germline mutations (28/61, 45.9%). Patients with FANC mutations have a significantly lower absolute reticulocyte count and CD34+ % in the bone marrow and also lower 3-, 6-, and 9-month IST response than that without mutation, which were 0% vs. 25% (P = 0.017), 26.3% vs. 42.1% (P = 0.495), and 29.4% vs. 72.2% (P = 0.011), especially in anti-thymocyte globulin combined with the cyclosporin A (ATG + CsA) group, which were 0% vs.33.4% (P = 0.143), 25% vs.83.3% (P = 0.103), and 25% vs. 100% (P = 0.003), respectively. The event-free survival in the FANCwt group was also better than that in the FANCmut group (P = 0.016) and also showed in patients who received ATG + CsA treatment (P = 0.045). In addition, all the adverse effects of FANC germline mutation were not significant in stem cell–transplanted group. Our result indicated that the WES-based detection of FANC heterozygous germline mutations may have a great meaning in predicting IST response of acquired AA. This study was registered at chictr.org.cn (# ChiCTR2100054992).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acquired aplastic anemia (AA) is a bone marrow disorder pathologically characterized by empty bone marrow and thus pancytopenia [1]. Immunosuppressive therapy (IST) and hematopoietic stem cell transplantation (HSCT) are the first-line treatments for AA. Despite a good response rate of 70–90% in AA [2], a great number of younger patients (≤ 40 years of age) is still hesitant for HSCT therapy due to the risk of treatment-related mortality and chronic and refractory complications, as well as unavailable donors. In China, over 70% of AA patients received IST as the first-line treatment, and the response rates in severe AA, non-severe AA, and transfusion-dependent AA patients were reported 60.6%, 64.3%, and 69.4%, respectively [3], denoting that approximately 40% of patients were unresponsive to IST. Several studies identified the influencing factors for varying IST response and survival, and the factors included patient age, disease severity, absolute reticulocyte (Ret) count (ARC), and the interval between diagnosis and treatment [4,5,6]. However, the overall response was never over 90%, which prompted us to further explore the underlying reasons.
With the advent of next-generation sequencing (NGS), new molecular insights into the pathogenesis of AA have been achieved. Some genetic mutations detected by NGS such as DNMT3A, ASXL1, TP53, RUNX1, and CSMD1 were related to lower response to IST and poor overall and progression-free survival (PFS), while mutations on PIGA and BCOR/BCORL1 were correlated with a better outcome. These elucidations in gene mutations may guide treatment of AA patients [7]. Whole-exome sequencing (WES), a new approach designed to sequence protein-coding regions of the genome that account for 1% of the genome [8], opened the door for identifying potential pathogenic genetic variants without spending the considerable resources required for the entire genome analysis. Up to date, a limited report is available on the use of WES in exploring the etiology and pathogenesis of AA. The WES is an accurate molecular technique to rule out congenital hematopoietic failures in young patients with pancytopenia. In our clinical center, we use the WES technique in younger patients suspected of AA if they can afford the expense. We found unexpected high FANC mutations in patients with AA (~ 50%), compared with 0.3–0.5% reported in the general healthy population [9]. Previous studies found that loss of function of any of the FANC genes may affect the expression of FANC protein and further influence the stability of hematopoietic stem cell chromosomes resulting in progressive bone marrow dysfunction and sensitivity to DNA cross-linking agents [10]. In addition, the intrinsic defects of hematopoietic stem cells in FA patients may cause B cells to be in long-term exposure to the harmful pro-apoptotic marrow environment, which was associated with decreased systemic immune function. But the effect of FANC heterozygous germline mutation on AA remained to be elaborated. In this study, we aimed to explore the significance of FANC heterozygous germline mutation in response to IST or HSCT and prognosis in AA patients.
Methods
Study design
The data of newly diagnosed AA patients in the First Affiliated Hospital of Zhejiang Chinese Medical University from January 2019 to July 2021 were retrospectively reviewed. The diagnosis and assessment of the disease were confirmed based on the Camitta criteria [11] and 2015 BJH guidelines [12], and the cases included severe aplastic anemia (SAA), very severe aplastic anemia (VSAA), non-severe aplastic anemia (NSAA), and transfusion-dependent none-severe aplastic anemia (TD-NSAA). Informed consent was obtained according to the Helsinki Declaration. This study was also registered at chictr.org.cn (# ChiCTR2100054992).
Patient selection
Inclusion criteria were (1) patients younger than 40 years old; (2) patients diagnosed with AA; (3) patients who had a WES analysis result; and (4) patients who were negative for chromosomal breakage test.
Exclusion criteria were as follows: patients who had other or secondary pancytopenia, including paroxysmal nocturnal hemoglobinuria (PNH), myelodysplastic syndrome (MDS), hypocellular MDS, hypo-proliferative acute myeloid leukemia, and myelofibrosis, were excluded based on comprehensive differentiation diagnosis, including bone marrow biopsy/smear, bone marrow CD34+ ratio, and flow cytometry (FCM) analysis as well as NGS results.
Baseline characteristics of patients
The baseline clinical characteristic of patients included age, gender, severity of disease, disease course defined as the interval time from diagnosis to treatment, treatment history, blood transfusion, routine blood test, and CD34+ % in bone marrow cells. Information on outcome variables was also retrieved for analysis.
WES and data analysis
Bone marrow or peripheral blood was collected from AA patients, and WES was performed to check the FANC family (FANCA, FANCB/FAAP95, FANCC, FANCD1/BRCA2, FANCD2, FANCE, FANCF, FANCG/XRCC9, FANCI, FANCJ/BRIP1, FANCL, FANCM, FANCN/PALB2, FANCO/RAD51C, FANCP/SLX4, FANCQ/ERCC4, FANCR/RAD51, FANCS/BRCA1, FANCT/UBE2T, FANCU/XRCC2, FANCV/REV7, and FANCW/RFWD3) mutation status. All the mutation was further confirmed as germline mutation (heterozygous) with rechecking of the oral mucosa sample by means of PCR sequencing–based typing (PCR-SBT). The procedure for WES sequencing and data analysis was as follows.
DNA extraction and detection
Genomic DNA extracted from the bone marrow or peripheral blood for each sample was fragmented to an average size of 180~280 bp and subjected to DNA library creation using established Illumina paired-end protocols. The Agilent SureSelect Human All ExonV6 Kit (Agilent Technologies, Santa Clara, CA, USA) was used for exome capture according to the manufacturer’s instructions. The Illumina NovaSeq 6000 platform (Illumina Inc., San Diego, CA, USA) was utilized for genomic DNA sequencing to generate 150-bp paired-end reads with a minimum coverage of 10× for ~ 99% of the genome (mean coverage of 100×).
Data analysis
After sequencing, basecall file conversion and demultiplexing were performed with bcl2fastq software (Illumina). The resulting fastq data were submitted to in-house quality control software for removing low-quality reads and then were aligned to the reference human genome (hg19) using the Burrows-Wheeler Aligner (bwa) [13], and duplicate reads were marked using sambamba tools [14]. SNP/INDEL calling: single nucleotide variants (SNVs) and indels were called with SAMtools to generate gVCF [15]. The raw calls of SNVs and INDELs were further filtered with the following inclusion thresholds: (1) read depth > 4; (2) root-mean-square mapping quality of covering reads > 30; and (3) the variant quality score > 20.
Annotation
Annotation was performed using ANNOVAR [16]. Annotations included minor allele frequencies from public control data sets as well as deleteriousness and conservation scores enabling further filtering and assessment of the likely pathogenicity of variants.
Rare variant filtering
Filtering of rare variants was performed as follows: (1) variants with a MAF less than 0.05 in 1000 genomic data (1000g_all) [17], esp6500siv2_all [18], and gnomAD data (gnomAD_ALL and gnomAD_EAS) [19]. (2) Only SNVs occurring in exons or splice sites (splicing junction 10 bp) are further analyzed since we are interested in amino acid changes. (3) Then, synonymous SNVs which are not relevant to the amino acid alternation predicted by dbscSNV are discarded. The small fragment non-frameshift (< 10 bp) indel in the repeat region defined by RepeatMasker is discarded. (4) Variations are screened according to scores of SIFT [20], Polyphen [21], MutationTaster [22], and CADD [23] softwares. The potentially deleterious variations are reserved if the score of more than half of these four softwares supports harmfulness of variations [24]. Sites (> 2 bp) that did not affect alternative splicing were removed.
ACMG classification
In order to better predict the harmfulness of variation, the classification system of the American College of Medical Genetics and Genomics (ACMG) was used. The variations are classified into pathogenic, likely pathogenic, uncertain significance, likely benign, and benign [25].
Immunological index evaluation
On WES analysis, we found that besides FANC mutations, some patients also had other mutations that may affect the immune system. The serum immunoglobulins and lymphocyte subsets in peripheral blood including immunoglobulin A (IgA), IgG, IgM, CD4+CD25+CD127−Tregs, CD3+CD4+ T helper cells (Th), CD3+CD8+ cytotoxic T cells (Tc), the ratio of CD4+/CD8+, and CD19+B lymphocytes were collected and analyzed.
Treatment strategies
The selection of treatment was based on the severity of the disease, age, and availability of donors as well as economic status, and all the decision was made with fully informed consent. For patients diagnosed with TD-NSAA, the standard management had no consensus yet. For patients who showed high value in obtaining a higher response, the HSCT and intensive IST were recommended. For patients who cannot afford the expense, cyclosporin (CsA) single treatment or supportive management was performed.
CsA single treatment
The oral dose of CsA was 3–5 mg/kg/day, with a general target blood concentration (valley concentration) of 150–250 μg/L for adults, or 100–150 μg/L for children. The clinical dosage of CsA could be adjusted based on the drug concentration and curative effect.
ATG combined with CsA
The dose of rabbit ATG (Thymoglobulin, Sanofi, France) was 3–4 mg/kg/day, and the ATG was used continuously for 5 days. Adrenal glucocorticoid was administered simultaneously when ATG was used and gradually withdrawn 14 days later to prevent allergic reaction as well as serologic reaction. The CsA was initiated on the first day when ATG was started, and the dose was adjusted according to the target drug concentration.
HSCT
In our cohort, patients received allogeneic-HSCT (allo-HSCT) from HLA-identical sibling donor (ISD), matched unrelated donor (MUD), or haploidentical donor (HID). The conditioning regimen included cyclophosphamide of 30–50 mg/kg/day for 4 days, fludarabine of 30 mg/m2 for 5 days, and rabbit ATG (Thymoglobulin, Sanofi, France) of 2.5 mg/kg/day for 4 days. CsA, mycophenolate mofetil (MMF), and methotrexate (MTX) were administered as GVHD prophylaxis regimens.
Efficacy assessment
Treatment efficacy was assessed at 3rd, 6th, and 9th months after treatment initiation. All the clinical data were collected, and the baseline comparison was carried out. The patients who were lost to follow-up or treated for less than 3 months were not included in the efficacy evaluation. The treatment response in SAA was defined as follows [12]: (1) complete response (CR), hemoglobin concentration normal for age and gender, ANC count > 1.5 × 109/L, and PLT count > 150 × 109/L; (2) partial response (PR), transfusion independent, and no longer meeting criteria for severe disease; (3) no response (NR) and still severe. The treatment response in NSAA was defined as follows: (1) CR, the same criteria as for severe disease; (2) PR, transfusion-independent (if previously required) or doubling or normalization of at least one lineage (in line with any one of the CR criteria) or increase above baseline: hemoglobin of 30 g/L (if initially < 60), ANC of 0.5 × 109/L (if initially < 0.5), PLT of 20 × 109/L (if initially < 20); and (3) NR, worse or not meeting the criteria.
Statistical analysis
The IBM SPSS 23.0 software was used for data analysis. The Shapiro-Wilk test was utilized to evaluate the normality of quantitative data. Quantitative data with normal distribution were assessed by a parametric test and those with non-normal distribution by a non-parametric test. Categorical data were assessed by Fisher’s exact test. Quantitative data conforming to normal distribution were represented as mean ± standard deviation (SD), and those with skewed distribution as median and 1st–3rd quartiles. The enumeration data described the number of cases and percentages (%). Survival curves were constructed using the Kaplan-Meier method, and the log-rank test was used to determine differences between survival proportions. The P < 0.05 was considered statistically significant.
Results
Patients’ characteristics
Characteristic analysis of entire population
A total of 61 patients diagnosed with AA and who underwent WES analysis were enrolled in this study. There were 27 females and 34 males with a median age of 23 (9–40) years. According to the severity of the disease, there were 9 cases of very severe AA (VSAA), 16 patients with severe AA (SAA), 28 patients with transfusion-dependent non-severe AA (TD-NSAA), and 8 cases of non-severe AA (NSAA). The rate of FANC germline mutations in our center accounts for 45.9% (28/61), and all the mutations were heterozygous. Detailed clinical data of patients with gene mutation are shown in Supplemental Table 1. The frequencies of FANC mutant genes were 7/38 for FANCA, 4/38 for PALB2 (FANCN), 4/38 for FANCD1, 4/38 for FANCD2, 4/38 for SLX4 (FANCP), 3/38 for FANCE, 2/38 for FANCL and FANCI, and 1/38 for FANCF, FANCG, FANCM, FANCB, FANCC, ERCC4 (FANCP), BRIP1 (FANCJ), and UBE2T (FANCT) (Fig. 1).
Characteristic analysis based on FANC status
To better understand the influence of FANC status on the baseline characteristics of the AA, the patients were divided into two groups based on FANC mutation status, AA with wide-type FANC (FANCwt) and AA with mutated FANC (FANCmut). The baseline clinical characteristics, such as age, gender, the severity of disease, disease course, treatment history, blood transfusion, peripheral hemogram, and absolute reticulocyte count, as well as CD34+ % of bone marrow cells, were compared, and all the indexes were similar across the subgroups (Table 1). However, the absolute reticulocyte count (ARC) and CD34+ % of bone marrow were found remarkably lower in the FANC mutation group (P = 0.021, 0.015, respectively). In addition, there were also more VSAA and SAA cases in the FANCmut group (14/28) when compared to the FANCwt group (11/33), but not statistically significant (P = 0.205).
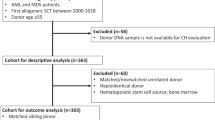
Treatment distribution
For all 61 patients enrolled in the analysis, the treatment regimens were selected based on the severity of the disease and patients’ preferences (Fig. 2). Forty-four patients initially received IST (29 patients with CsA single treatment and 15 patients with ATG + CsA), 12 patients firstly underwent HSCT (including 3 from 10/10 MUD, and 9 from HID), and the remaining 5 patients only received supportive treatment. During the observation, in the CsA single treatment group (n = 19), 4 patients were lost to follow-up within 3 months (Fig. 3).
Response comparison in the entire population
There were 25, 15, and 12 patients who were eligible for efficacy analysis in the CsA single treatment, ATG + CsA, and HSCT groups, respectively. The overall hematological response in patients who received HSCT at 3rd, 6th, and 9th months was all 100%, compared to 12.0%, 25.0%, and 50.0% in the CsA single treatment group and 13.4%, 50%, and 53.8% in the ATG + CsA group, respectively. The combined IST efficiency at the 3rd, 6th, and 9th month was 12.5%, 34.2%, and 51.4%, respectively. The were no significant differences between the CsA single treatment and ATG + CsA groups at each time point, and the efficiency of HSCT was superior to IST, regardless of the CsA group or ATG + CsA group at any time points (3rd, 6th, and 9th months, all P < 0.01) (Fig. 4).
Subgroup efficacy analysis
Response rate of entire population based on FANC germline mutations
To assess the effect of FANC germline mutation on therapy response, patients were divided into subgroups based on FANC status, and the distribution of therapeutic methods was similar between groups (Supplemental Table 2). The overall hematological response rates in patients with FANC mutation at 3rd, 6th, and 9th months were 23.1%, 44.0%, and 42.8%, respectively, compared to 40.0%, 54.2%, and 78.3% in the FANC non-mutation subgroup, and significant differences were found at the 9th month (P = 0.029), while no differences were found at the 3rd and 6th (P = 0.237 and 0.572, respectively) (Fig. 5).
Response rate of entire population based on FANC germline mutations. The response rate (CR+PR) of aplastic anemia patients with or without FANC mutation were compared based on 3, 6, 9 months observation. ns means no significant difference, *<0.05. The number of patients included in each subgroup were shown
Comparison of IST vs. HSCT on response rate based on FANC status
Based on FANC status, the response was further compared between different therapeutic methods, IST vs. HSCT. In the FANCwt group, results showed that the efficiencies of IST were 25%, 42.1%, and 72.2% at the 3rd, 6th, and 9th months, compared to all 100% in the HSCT group. And the difference was significant at the 3rd and 6th months (P = 0.005, P = 0.041), but not at the 9th month (P = 0.280) (Fig. 6A). In the FANCmut group, the results were 0%, 26.3%, and 29.4% in the IST group, compared to all 100% in the HSCT group at 3rd-, 6th-, and 9th-month evaluation, respectively. All had a significant difference (P < 0.001, P = 0.002, and P = 0.001, respectively) (Fig. 6B). When considering the effect of FANC status on IST or HSCT efficiency, we found that the FANC status did not influence the HSCT efficiency (all 100%), but in the IST, the 3rd-, 6th-, and 9th-month efficiencies were 25.0% vs. 0% (P =0 .017), 42.1% vs. 26.3% (P = 0.498), and 72.2% vs. 29.4% (P = 0.011), respectively, between FANCwt and FANCmut (Fig. 6C).
Comparison of IST vs. HSCT on response rate based on FANC status. All the patients were divided into two groups based on FANC mutation. The comparison of response rate (CR+PR) of patients (with or without FANC mutation, Figure 6A and 6B) to HSCT or IST, as well as IST response based on FANC mutation (Figure 6C) were compared based on 3, 6, 9 months observation. ns means no significant difference, *<0.05, **<0.01, ***<0.001. The number of patients included in each subgroup were shown
Comparison of different IST regimens on response rate based on FANC status
Twenty-four patients with FANCwt status and 20 patients with FANCmut status received IST, and the basic characteristics are summarized in Table 2. No significant differences were observed among age, gender, blood transfusion, and the severity of AA. The specific distribution according to the severity of AA is shown in Table 2. The WBC count, neutrophil count, HB, and absolute Ret count were much lower in the IST-FANCmut group (P = 0.018, 0.018, 0.031, and 0.007, respectively). In the FANCwt group, results showed that the efficiencies of CsA were 21.4%, 23.1%, and 61.6% at 3rd, 6th, and 9th months, compared to 33.4%, 83.4%, and 100% in the ATG + CsA group. And the difference was only significant at the 6th-month evaluation (P = 0.041) (Fig. 7A). In the FANCmut group, the results were 0%, 27.3%, and 33.3% in the CsA group, compared to 0%, 25.0%, and 25.0% in the ATG + CsA group at the 3rd-, 6th-, and 9th-month evaluation, respectively. And no statistical differences were observed (all P > 0.05) (Fig. 7B). When considering the effect of FANC status on CsA or ATG + CsA efficiency, we found that in the CsA single treatment group, the 3rd-, 6th-, and 9th-month efficiencies were 21.4% vs. 0% (P = 0.230), 23.1% vs. 27.3% (P = 1.0), and 61.6% vs. 33.3% (P =0.387), respectively; no statistical differences were observed between FANCwt and FANCmut (Fig. 7C). In the ATG + CsA group, the 3rd-, 6th-, and 9th-month efficiencies were 33.4% vs. 0% (P = 0.143), 83.3% vs. 25% (P = 0.103), and 100% vs. 25% (P = 0.003), respectively, and the difference was only significant at the 9th-month evaluation (Fig. 7D).
Comparison of different IST regimens on response rate based on FANC status. All the aplastic anemia patients received IST were divided into two groups based on FANC mutation. The comparison of response rate (CR+PR) of patients (with or without FANC mutation, Figure 7A and 7B) to CsA or ATG+CsA, as well as IST (CsA or ATG+CsA, Figure 7C and 7D) response based on FANC mutation were compared based on 3, 6, 9 months observation. ns means no significant difference, *<0.05. The number of patients included in each subgroup were shown
Comparison of immunological indexes based on FANC status
The WES analyses showed that besides the FANC mutation, the most coexisting mutations that may affect the immune system were LIG4 (3/26), and the others include TNFRS13B, AIRE, SMARCAL1, C8A, RFT1, and SERPING1 (1/26 in all). Considering the effect of immunological status on the treatment response in AA, we analyzed the lymphocytes and serum levels of immunoglobulins in peripheral blood before treatment. There were no statistical differences in IgA, IgG, IgM, Treg (CD4+CD25+CD127-), Th cells (CD3+CD4+), Ts cells (CD3+CD8+), and the ratio of CD4/CD8, and B cells (CD19+) among the FANC germline mutation subgroups (all P > 0.05) (Supplemental Table 3).
Overall survival (OS) comparison based on therapy and FANC status
We excluded 4 patients who were lost to follow-up and 5 patients who only received supportive treatment. Finally, 40 patients who received IST and 12 patients who received HSCT were eligible for OS analysis. There were respectively 20 and 6 patients who received IST or HSCT in the FANCwt group and 20 and 6 patients who received IST or HSCT in the FANCmut group. The median follow-up period was 18.25 (1.5–72) months. There was only one patient in the FANCmut group whose condition transformed into acute myeloid leukemia (AML) 49 months after the failure of CsA single treatment and died due to severe infection. All others survived at the time of the last follow-up. The differences in overall survival in patients with or without FANC mutation were not present (P > 0.05) (Fig. 8A). And there were also no differences among different therapeutic methods (HSCT, ATG + CsA, or CsA, with or without FANC mutations) (Fig. 8B).
Overall survival (OS) and event free survival (EFS) comparison based on therapy and FANC status. The OS of entire population (Figure 8A) and different treatment regime (Figure 8B) based on FANC mutation were compared, and no statistic differences were observed. The EFS of entire population (Figure 8C) and different treatment regime (Figure 8D) based on FANC mutation were compared. The patients without FANC mutation (FANCwt) had a significantly better EFS than that with mutation (FANCmut) (P<0.05), and the ATG+CsA treatment group without FANC mutation showed a better EFS compared to that with FANC mutation (P<0.05)
Event-free survival (EFS) comparison based on therapy and FANC status
At a median follow-up period of 18.25 (1.5–72) months, 40 patients who received IST and 12 patients who received HSCT were eligible for the EFS analysis. In the FANCwt group, two patients further received HSCT because of the failure from CsA single treatment (20.5 months and 45.5 months). Another one relapsed at 71 months after partial remission from ATG + CsA treatment and suffered from transfusion-dependent anemia and thrombocytopenia. For patients in the FANCmut group, six patients switched treatments after preliminary treatment failure, including one that transformed into acute myeloid leukemia. All these results showed that the patients without FANC mutation had a better EFS (P = 0.016) (Fig. 8C), and the subgroup analysis showed that the differences were significant in patients received ATG + CsA treatment (P = 0.045) (Fig. 8D).
EFS risk evaluation based on patients’ baseline characteristics
We used cox regression to identify the possible factors affecting the EFS. Firstly, all possible factors such as age, degree of disease, treatment regimens, FANC status, the interval time from diagnosis to treatment, and 3-, 6-, and 9-month response were included in cox regression separately, and then variables with a P value < 0.05 were added to the further cox regression (Table 3). The results showed that FANC mutation was the only predictor associated with poor EFS (odds ratio (OR) = 5.576, 95% confidence interval (CI) 1.169–26.590, P = 0.031) (Fig. 9).
Event free survival (EFS) risk evaluation based on patients’ baseline characteristics. Age, degree of disease, treatment regimens, FANC mutation and 3, 6, 9-month response were entered into cox regression separately, results showed FANC mutation was the only predictor associated with poor EFS (P=0.031)
Discussion
Acquired aplastic anemia has its unique clinical behavior, and recent advances have also shown more complicated phenotypes and imperfect genotype-phenotype correlations [26]. In China, quite a lot of patients with AA choose IST, because of age limitation, financial difficulties, unsuitable donors, and other reasons. In patients who are treated with IST, especially ATG + CsA, the response rate was not good as those reported in Western countries. This variation in response may be because of the unavailability of horse-ATG [27] and thus the species differences in ATG, which was not comprehensively elucidated. In addition, with the analysis of IST predictive response factors [4,5,6], there are still a considerable number of patients suffering from poor prognoses even if they have workable treatment.
With the widespread use of WES diagnostic techniques in the clinic, the number of patients benefiting from these tools has been rapidly increasing. The biallelic compromise of one of 22 FANC genes involving the FA/BRCA repair pathway caused Fanconi anemia (FA) with an incidence rate of 1 in 300,000 live births and a prevalence rate of 1–9 per million [28, 29], which was reported to be the most frequent inherited cause of bone marrow disorder (BMF) clinically characterized by congenital malformations [29, 30]. The FANC mutation carrier frequency varies in different regions. Generally, the mutation frequency of the FANC gene in a normal population is 1/189 and is increased to 1/64 in some populations with a high incidence of FA [31]. At present, there is no clinical report on acquired aplastic anemia complicated with FANC germline mutations and also no data report on the frequency of FANC mutations in Chinese. In this study, the WES analyses showed that there was an unexpectedly high rate of FANC germline mutations in the cohort (28/61, 45.9%), which was probably 96–160 times than the healthy population, denoting the significance of this exploration. Overall, genetic variants were found in most of the patients, with an average of 5 mutations per patient, but the proportion of FANC gene mutation was higher than that of other gene mutations in the whole-exome sequencing 11.73% (38/324) vs. 0.31–1.54% (1/324–5/324) (detailed gene mutation information is shown in supplemental Table 4).
Biallelic inactivation of the FANC gene results in the rare and autosomal recessive disease, Fanconi anemia, a disorder characterized by developmental anomalies, bone marrow failure, and susceptible to malignancies. In this study, all FANC mutated patients were confirmed negative for mitomycin-C-induced chromosome breakage tests and did not have any congenital malformations as well as family history. Besides, all of the FANC mutations identified in patients were heterozygous germline mutations, which may explain the lack of FA phenotype despite FANC mutations. Based on the baseline clinical analysis, we found that the patients with FANC mutation had a significantly lower level of ARC (P < 0.05), probably leading to more VSAA + SAA cases in the mutation group (50% vs. 33.3%, P = 0.205). More patients received IST than HSCT, and regarding the response rate of IST, CsA was comparable to ATG + CsA, but the response rate was much lower than HSCT (3-, 6-, and 9-month results). Further, subgroup analysis based on the FANC mutation showed that there was an earlier (3-month result) and a better (9-month result) IST response than that in the FANCmut group. The patients with wide-type FANC had a much better response to ATG + CsA than CsA (but P > 0.05), while the FANC mutation eliminated the advantage of ATG + CsA (regardless of CsA or ATG + CsA, the response of < 40% at any time points of evaluation). The long-term outcome showed that OS was not influenced by therapeutic methods as well as FANC status; however, the EFS was significantly better in IST without FANC mutation than in cases with mutations. All the results indicated that FANC mutation is associated with the response and EFS of AA patients receiving ATG + CsA treatment, and HSCT treatment performed better in this population.
FANC mutation was involved in the regulation of hematopoietic function. The mechanism of bone marrow failure caused by FANC gene mutation remains to be elucidated. FA pathway coordinates DNA damage signaling and enzymatic DNA repair processes during DNA replication. Germline homozygous mutations in the FA genes led to deficiencies of FA DNA repair pathway, which was thought to be the main mechanism responsible for bone marrow failure in FA [32]: (a) HSC defect starts before birth, and mutant HSCs are unambiguously reduced during development resulting in stem cell apoptosis [32, 33]; (b) attrition of HSC pools caused by unresolved DNA damage-dependent cell cycle arrest and apoptosis [32]. Studies also found that non-canonical pathways mediated stem cell exhaustion. Many Fanconi anemia proteins [34] participated in control of signaling pathways that stress HSCs; they had additional functions in protecting cells from oxidative stress, inflammation, and endogenous aldehyde–induced death, as well as facilitating autophagy. When faced with inflammatory stress, FANC mutated HSCs will be hypersensitive, resulting in the overproduction of inflammatory cytokines [29]. Overexpressed TNF-α and IFN-γ inhibited erythropoiesis [35], increased TGF-β1 that arrested the pro-apoptotic state, increased regulatory T cells, reduced B/NK cells, and inhibited the growth and differentiation of early hematopoietic stem cells (HSCs) as well as IgG and IgM [36]. All these may be reasonable for poor IST efficacy in AA patients with FA mutation. However, these mechanisms were from the research on bone marrow failure caused by FA homozygous mutation. Recently, studies revealed a certain incidence of heterozygous FANC mutation in AA patients [37, 38], but the underlying mechanisms in bone marrow failure were not well explained. They speculated that the eventual onset of the disease originated from heterozygous FANC mutation was more complex and delayed and might relate to the accumulating chromosomal structural abnormalities, which implied the normal alleles are not entirely protective. In this study, we also explored the immunophenotype of peripheral blood lymphocytes and serum levels of immunoglobulins (Ig) that may be involved in the immune response, but there were no statistical differences. However, the patients with the FANC mutation had lower bone marrow CD34+ cells and more severe cases. We were not able to verify the mechanisms in this study, and more exploratory studies are needed to explain the contribution of heterozygous FANC mutation in the development of AA and its effect in lower IST response.
In conclusion, for patients younger than 40 years old without FANC germline mutation, ATG + CsA can exert a curative effect that was comparable to HSCT, but for cases with FANC mutation, HSCT can be a better choice. FANC germline mutation can negatively influence the treatment response with IST in Chinese aplastic anemia patients. The relatively small sample size is the limitation of our study; we will further initiate multi-center and larger sample size study.
Data availability
The data used and/or analyzed during the current study are available from the corresponding author upon a reasonable request.
References
Young NS, Calado RT, Scheinberg P (2006) Current concepts in the pathophysiology and treatment of aplastic anemia. Blood 108(8):2509–2519. https://doi.org/10.1182/blood-2006-03-010777
Georges GE, Doney K, Storb R (2018) Severe aplastic anemia: allogeneic bone marrow transplantation as first-line treatment. Blood Adv 2(15):2020–2028. https://doi.org/10.1182/bloodadvances.2018021162
Zhu XF, He HL, Wang SQ, Tang JY, Han B, Zhang DH, Wu LQ, Wu DP, Li W, Xia LH, Zhu HL, Liu F, Shi HX, Zhang X, Zhou F, Hu JD, Fang JP, Chen XQ, Ye TZ et al (2019) Current treatment patterns of aplastic anemia in China: a prospective cohort registry study. Acta Haematol 142(3):162–170. https://doi.org/10.1159/000499065
Bacigalupo A, Oneto R, Schrezenmeier H, Hochsmann B, Dufour C, Kojima S, Zhu X, Chen X, Issaragrisil S, Chuncharunee S, Jeong DC, Giammarco S, Van Lint MT, Zheng Y, Vallejo C (2018) First line treatment of aplastic anemia with thymoglobuline in Europe and Asia: outcome of 955 patients treated 2001-2012. Am J Hematol 93(5):643–648. https://doi.org/10.1002/ajh.25081
Jin JY, Kim DW, Lee JW, Han CW, Min WS, Park CW, Kim CC, Kim DJ, Kim HK, Song HH (1995) Immune suppression therapy in aplastic anemia: influencing factors on response and survival. Korean J Intern Med 10(1):25–31. https://doi.org/10.3904/kjim.1995.10.1.25
Vaht K, Goransson M, Carlson K, Isaksson C, Lenhoff S, Sandstedt A, Uggla B, Winiarski J, Ljungman P, Brune M, Andersson PO (2018) Low response rate to ATG-based immunosuppressive therapy in very severe aplastic anaemia - a Swedish nationwide cohort study. Eur J Haematol 100(6):613–620. https://doi.org/10.1111/ejh.13057
Yoshizato T, Dumitriu B, Hosokawa K, Makishima H, Yoshida K, Townsley D, Sato-Otsubo A, Sato Y, Liu D, Suzuki H, Wu CO, Shiraishi Y, Clemente MJ, Kataoka K, Shiozawa Y, Okuno Y, Chiba K, Tanaka H, Nagata Y et al (2015) Somatic mutations and clonal hematopoiesis in aplastic anemia. N Engl J Med 373(1):35–47. https://doi.org/10.1056/NEJMoa1414799
Prokop JW, May T, Strong K, Bilinovich SM, Bupp C, Rajasekaran S, Worthey EA, Lazar J (2018) Genome sequencing in the clinic: the past, present, and future of genomic medicine. Physiol Genomics 50(8):563–579. https://doi.org/10.1152/physiolgenomics.00046.2018
Kutler DI, Singh B, Satagopan J, Batish SD, Berwick M, Giampietro PF, Hanenberg H, Auerbach AD (2003) A 20-year perspective on the International Fanconi Anemia Registry (IFAR). Blood 101(4):1249–1256. https://doi.org/10.1182/blood-2002-07-2170
Dong H, Nebert DW, Bruford EA, Thompson DC, Joenje H, Vasiliou V (2015) Update of the human and mouse Fanconi anemia genes. Hum Genomics 9:32. https://doi.org/10.1186/s40246-015-0054-y
Camitta BM (1988) Criteria for severe aplastic anaemia. Lancet 1(8580):303–304. https://doi.org/10.1016/s0140-6736(88)90388-1
Killick SB, Bown N, Cavenagh J, Dokal I, Foukaneli T, Hill A, Hillmen P, Ireland R, Kulasekararaj A, Mufti G, Snowden JA, Samarasinghe S, Wood A, Marsh JC, British Society for Standards in H (2016) Guidelines for the diagnosis and management of adult aplastic anaemia. Br J Haematol 172(2):187–207. https://doi.org/10.1111/bjh.13853
Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25(14):1754–1760. https://doi.org/10.1093/bioinformatics/btp324
Tarasov A, Vilella AJ, Cuppen E, Nijman IJ, Prins P (2015) Sambamba: fast processing of NGS alignment formats. Bioinformatics 31(12):2032–2034. https://doi.org/10.1093/bioinformatics/btv098
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R, Genome Project Data Processing S (2009) The sequence alignment/map format and SAMtools. Bioinformatics 25(16):2078–2079. https://doi.org/10.1093/bioinformatics/btp352
Wang K, Li M, Hakonarson H (2010) ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res 38(16):e164. https://doi.org/10.1093/nar/gkq603
Genomes Project C, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR (2015) A global reference for human genetic variation. Nature 526(7571):68–74. https://doi.org/10.1038/nature15393
Yang RQ, Jabbari J, Cheng XS, Jabbari R, Nielsen JB, Risgaard B, Chen X, Sajadieh A, Haunso S, Svendsen JH, Olesen MS, Tfelt-Hansen J (2014) New population-based exome data question the pathogenicity of some genetic variants previously associated with Marfan syndrome. BMC Genet 15:74. https://doi.org/10.1186/1471-2156-15-74
Holgersen EM, Gandhi S, Zhou Y, Kim J, Vaz B, Bogojeski J, Bugno M, Shalev Z, Cheung-Ong K, Goncalves J, O’Hara M, Kron K, Verby M, Sun M, Kakaradov B, Delong A, Merico D, Deshwar AG (2021) Transcriptome-wide off-target effects of steric-blocking oligonucleotides. Nucleic Acid Ther 31(6):392–403. https://doi.org/10.1089/nat.2020.0921
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4(7):1073–1081. https://doi.org/10.1038/nprot.2009.86
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR (2010) A method and server for predicting damaging missense mutations. Nat Methods 7(4):248–249. https://doi.org/10.1038/nmeth0410-248
Schwarz JM, Rodelsperger C, Schuelke M, Seelow D (2010) MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods 7(8):575–576. https://doi.org/10.1038/nmeth0810-575
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J (2014) A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 46(3):310–315. https://doi.org/10.1038/ng.2892
Muona M, Berkovic SF, Dibbens LM, Oliver KL, Maljevic S, Bayly MA, Joensuu T, Canafoglia L, Franceschetti S, Michelucci R, Markkinen S, Heron SE, Hildebrand MS, Andermann E, Andermann F, Gambardella A, Tinuper P, Licchetta L, Scheffer IE et al (2015) A recurrent de novo mutation in KCNC1 causes progressive myoclonus epilepsy. Nat Genet 47(1):39–46. https://doi.org/10.1038/ng.3144
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, Committee ALQA (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Kallen ME, Dulau-Florea A, Wang W, Calvo KR (2019) Acquired and germline predisposition to bone marrow failure: diagnostic features and clinical implications. Semin Hematol 56(1):69–82. https://doi.org/10.1053/j.seminhematol.2018.05.016
Scheinberg P, Nunez O, Weinstein B, Scheinberg P, Biancotto A, Wu CO, Young NS (2011) Horse versus rabbit antithymocyte globulin in acquired aplastic anemia. N Engl J Med 365(5):430–438. https://doi.org/10.1056/NEJMoa1103975
Moreno OM, Paredes AC, Suarez-Obando F, Rojas A (2021) An update on Fanconi anemia: clinical, cytogenetic and molecular approaches (Review). Biomed Rep 15(3):74. https://doi.org/10.3892/br.2021.1450
Bagby GC (2016) Multifunctional Fanconi proteins, inflammation and the Fanconi phenotype. EBioMedicine 8:10–11. https://doi.org/10.1016/j.ebiom.2016.06.005
Peffault de Latour R, Soulier J (2016) How I treat MDS and AML in Fanconi anemia. Blood 127(24):2971–2979. https://doi.org/10.1182/blood-2016-01-583625
Rosenberg PS, Tamary H, Alter BP (2011) How high are carrier frequencies of rare recessive syndromes? Contemporary estimates for Fanconi anemia in the United States and Israel. Am J Med Genet A 155A(8):1877–1883. https://doi.org/10.1002/ajmg.a.34087
Rageul J, Kim H (2020) Fanconi anemia and the underlying causes of genomic instability. Environ Mol Mutagen 61(7):693–708. https://doi.org/10.1002/em.22358
Solanki A, Rajendran A, Mohan S, Raj R, Vundinti BR (2020) Mitochondrial DNA variations and mitochondrial dysfunction in Fanconi anemia. PLoS One 15(1):e0227603. https://doi.org/10.1371/journal.pone.0227603
Bagby G (2018) Recent advances in understanding hematopoiesis in Fanconi anemia. F1000Res 7:105. https://doi.org/10.12688/f1000research.13213.1
Dufour C, Corcione A, Svahn J, Haupt R, Poggi V, Beka’ssy AN, Scime R, Pistorio A, Pistoia V (2003) TNF-alpha and IFN-gamma are overexpressed in the bone marrow of Fanconi anemia patients and TNF-alpha suppresses erythropoiesis in vitro. Blood 102(6):2053–2059. https://doi.org/10.1182/blood-2003-01-0114
Korthof ET, Svahn J, Peffault de Latour R, Terranova P, Moins-Teisserenc H, Socie G, Soulier J, Kok M, Bredius RG, van Tol M, Jol-van der Zijde EC, Pistorio A, Corsolini F, Parodi A, Battaglia F, Pistoia V, Dufour C, Cappelli E (2013) Immunological profile of Fanconi anemia: a multicentric retrospective analysis of 61 patients. Am J Hematol 88(6):472–476. https://doi.org/10.1002/ajh.23435
Przychodzen B, Makishima H, Sekeres MA, Balasubramanian SK, Thota S, Patel BJ, Clemente M, Hirsch C, Dienes B, Maciejewski JP (2018) Fanconi anemia germline variants as susceptibility factors in aplastic anemia. MDS and AML Oncotarget 9(2):2050–2057. https://doi.org/10.18632/oncotarget.23328
Nie D, Zhang J, Wang F, Li X, Liu L, Zhang W, Cao P, Chen X, Zhang Y, Chen J, Ma X, Zhou X, Wu Q, Liu M, Liu M, Tian W, Liu H (2022) Fanconi anemia gene-associated germline predisposition in aplastic anemia and hematologic malignancies. Front Med 16(3):459–466. https://doi.org/10.1007/s11684-021-0841-x
Acknowledgements
We thank all the patients who gave consent to disclose their medical records and answered our review calls.
Funding
The present study was supported by the National Natural Science Foundation of China (No. 82174138), Zhejiang Scientific Research Fund of Traditional Chinese Medicine (No. 2020ZB085, No. 2022ZA059), and Health technology Plan of Zhejiang Province (No. 2022RC216), Project of Academic Inheritance Studio of Famous and Aged Chinese Medicine Experts in Zhejiang Province (No. GZS2021022).
Author information
Authors and Affiliations
Contributions
Dijiong Wu, Yingying Shen, and Baodong Ye conceived and designed the study. Yingying Shen, Hangchao Li, Qi Liu, and Yuzhu Li assisted in the acquisition of data. Yingying Shen, Qi Liu, Ying Chen, Shan Liu, and Dijiong Wu analyzed and interpreted the data. Yingying Shen, Qi Liu, Dijiong Wu, and Baodong Ye wrote, reviewed, and revised the manuscript. Wenbin Liu, Huijin Hu, Yuechao Zhao, Qinghong Yu, Haifeng Zhuang, Liqiang Wu, Zhiping Hu, Zhiyin Zheng, Jianping Shen, Shenyun Lin, Yiping Shen, and Yuhong Zhou treated and followed up the patients. All authors contributed toward data analysis, drafting, and critically revising the paper and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of the First Affiliated Hospital of Zhejiang Chinese Medical University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yingying Shen, Qi Liu, and Hangchao Li contribute equally
Supplementary information
ESM 1:
Supplement Table 1. Clinical features of AA with germline FANC mutation (DOC 67 kb)
ESM 2:
Supplement Table 2. Distribution of therapeutic methods of AA patients with/without FANC mutation (DOC 30 kb)
ESM 3:
Supplement Table3. Comparison of immunological status between AA patients with/without FANC mutation who received IST (DOC 34 kb)
ESM 4:
Supplemental Table 4. Detailed Gene Mutation distributions of all the AA patients (DOC 60 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, Y., Liu, Q., Li, H. et al. Whole-exome sequencing identifies FANC heterozygous germline mutation as an adverse factor for immunosuppressive therapy in Chinese aplastic anemia patients aged 40 or younger: a single-center retrospective study. Ann Hematol 102, 503–517 (2023). https://doi.org/10.1007/s00277-023-05086-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05086-9