Abstract
The comparative efficacy and safety of restrictive with liberal transfusion thresholds remain controversial in anemic preterm infants. This meta-analysis aimed to compare the efficacy and safety of these two transfusion thresholds for anemic preterm infants. We searched PubMed, Embase, Cochrane Library, and China National Knowledge Infrastructure (CNKI) for relevant randomized controlled trials (RCTs) comparing restrictive with liberal transfusion thresholds in anemic preterm infants through April 30, 2022. Two independent investigators screened literature, extracted data, and appraised the methodological quality of eligible studies. Meta-analysis was conducted using RevMan version 5.3.5. Twelve RCTs with 4380 preterm infants were included. Liberal transfusion threshold significantly increased the level of hemoglobin after transfusion (mean difference (MD): −10.03; 95% confidence interval (CI): −15.98 to −4.08; p=0.001; I2=94%) and hematocrit (MD: −3.62; 95%CI: −6.78 to −0.46; p=0.02; I2=80%) compared with restrictive transfusion. Infants’ age at first transfusion in restrictive transfusion group was higher than that of infants in liberal transfusion group (MD: 5.08; 95%CI: 2.27 to7.89; p=0.004; I2=54%); however, restrictive transfusion was associated with more time on supplemental oxygen (MD: 3.56; 95%CI: 1.93 to 5.18; p<0.001; I2=62%) and ventilator or CPAP (MD: 3.31; 95%CI: 1.42 to 5.20; p=0.006; I2=75%). For the remaining outcomes, two transfusion strategies were comparable. Furthermore, a series of sensitivity analyses confirmed the robustness of the level of hemoglobin after transfusion, age at first transfusion, time on ventilator or CPAP, and safety outcomes. Evidence with substantial heterogeneity indicates that liberal and restrictive transfusion thresholds are effective and safe blood cell transfusion strategies in anemic preterm infants, but the liberal strategy may be more effective in shortening the length of necessary respiratory support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm infants are at high risk for anemia due to immaturity, impaired erythropoiesis, and frequent blood sampling [1, 2]. Therefore, preterm infants have one of the highest transfusion requirements within the hospital setting [3], especially very (VLBW) or extremely low birth weight (ELBW) infants [4]. More than 90% of ELBW infants received at least one red blood cell transfusion during their initial hospitalization [5, 6]. Red blood cell transfusion has been demonstrated to have several benefits, such as maintaining high hemoglobin [7, 8] and reducing the risks of hypoxemia and apnea of prematurity [9, 10]. Although a low level of hemoglobin was considered to have an adverse impact on growth [11], some studies suggested that red blood cell transfusion can have several complications, such as intraventricular hemorrhage [12, 13], retinopathy of prematurity [14, 15], bronchopulmonary dysplasia [16, 17], necrotizing enterocolitis [18, 19], and death [20]. Therefore, several attentions have been paid to investigating the thresholds for red blood cell transfusion.
Various thresholds for red blood cell transfusion have been applied in clinical practice [21]; however, it could be mainly categorized into two strategies, including restrictive and liberal thresholds [3]. A series of previous randomized controlled trials (RCTs) have investigated the impact of different transfusion thresholds on clinical outcomes of anemic preterm infants but reported conflicting results [22,23,24]. Subsequently, several meta-analyses [25,26,27,28] have further evaluated the comparative efficacy and safety of restrictive versus liberal transfusion thresholds for treating anemic preterm infants and suggested that restrictive transfusion threshold was comparable to liberal transfusion threshold in death and neurodevelopment. However, the value of these findings dedicated to making the clinical decision was limited because several clinically important outcomes were not evaluated in previous meta-analyses, such as age at first transfusion, total transfusion volume, and time on supplemental oxygen. Moreover, some potentially eligible studies [29,30,31,32] published in the Chinese language were also not included in the meta-analysis.
Therefore, we conducted this meta-analysis to further evaluate the relative efficacy and safety of restrictive versus liberal transfusion thresholds in anemic preterm infants by including more eligible studies and more comprehensive outcomes.
Methods
We designed the current meta-analysis following the Cochrane Handbook for Systematic Reviews of Interventions version 6.2 [33]. We reported all results in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [34]. It is not necessary to include ethical approval and patients’ informed consent because this is a meta-analysis of published studies. It is necessary to say that the formal protocol of the current meta-analysis was not registered on any platform.
Search strategy
A systematic search was performed in PubMed, Embase, the Cochrane Library, and China National Knowledge Infrastructure (CNKI) to identify relevant RCTs which compared restrictive with liberal transfusion thresholds in anemic preterm infants. Two independent investigators performed the search. The search was limited from the establishment date of each database until April 30, 2022. We constructed a search strategy using medical subject heading (MeSH) and text words, and the following terms and their analogs were used: “anemia,” “premature infant,” “extremely premature infant,” “blood transfusion,” and “random.” The details of the search strategy are summarized in Table S1. We also manually screened the eligible studies included in the previous meta-analyses and the reference lists of all eligible studies to identify studies missing from database search. Any disagreement regarding study retrieval was resolved by discussion.
Selection criteria
According to the following selection criteria, two independent investigators selected eligible studies through screening title, abstract, and full text. Specifically speaking, studies were included if (1) participants were determined as anemic preterm infants with low birth weight (LBW, birth weight <2500 g), very low birth weight (VLBW, birth weight <1500 g), or extremely low birth weight (ELBW, birth weight <1000 g); (2) anemic preterm infants were assigned to receive restrictive or liberal transfusion threshold throughout their initial hospitalization; (3) at least one of physiological measurements (the level of hemoglobin after transfusion (g/l) and hematocrit (%)), transfusion-related indicators (age at the first transfusion, transfusion per infant, donor exposure per infant, and total transfusion volume), clinical outcomes (time on supplemental oxygen, time on ventilator or continuous positive airway pressure (CPAP), and the length of hospital stay), and safety outcomes (death or neurodevelopmental impairment, bronchopulmonary dysplasia, necrotizing enterocolitis, any retinopathy of prematurity, retinopathy of prematurity with stage >3, intraventricular hemorrhage, intraventricular hemorrhage with grade >3, apnea, periventricular leukomalacia, and patent ductus arteriosus) had to be reported; and (4) RCTs were published in English with full text.
We excluded ineligible studies according to the exclusion criteria as follows: (1) ineligible study designs such as case series, narrative review, animal study, meta-analysis; (2) essential data were not available for data analysis, and no response was received after sending an e-mail to the corresponding author; and (3) duplicate reports from the same participants that were published by the same group had relatively poor methodological quality and insufficient data.
Data extraction
Two independent investigators extracted the following essential data from original studies using a pre-designed standard information extraction sheet: characteristics of the included studies (the first author’s name, publication year, country, and sample size), participants’ baseline information (mean gestational age, the percentage of male infants, birth weight, and dose of per transfusion), clinical outcomes, and information of methodological quality. If an eligible study only reported the mean values of each group and p-value for the significance test between two groups, we estimated the same standard deviation (SD) for both groups using the formula recommended by the Cochrane Handbook. Moreover, if an eligible study reported results using median with interquartile range (IQR), we transformed it to be mean with SD using the recognized formula [35]. For the level of hemoglobin and hematocrit, we extracted the data after transfusion rather than the changing value between before transfusion and after transfusion for meta-analysis because most studies only reported values at randomization rather than before transfusion. Furthermore, these two values were evenly distributed between the two groups at randomization (level of hemoglobin (g/l): t=−0.437, p=0.672; hematocrit (%): t=0.189, p=0.855).
Risk of bias assessment
We appraised the risk of bias of eligible studies using the Cochrane Collaboration Risk of Bias tool from seven items as follows: random sequence generation (selection bias); allocation concealment (selection bias); blinding of personnel and participants (performance bias): blinding of outcome assessment (detection bias): incomplete outcome data (attrition bias); selective reporting (reporting bias); and other bias sources. Each item was rated as “low,” “unclear,” or “high” risk. Any disagreements regarding the risk of bias assessment were resolved through discussion. The results of the risk of bias assessment were graphically presented using RevMan version 5.4.
Statistical analysis
Meta-analysis was conducted using the RevMan version 5.4 software (The Cochrane Collaboration, Copenhagen, Denmark). Pooled results were expressed as the mean difference (MD) or relative risk (RR), with a 95% confidence interval (CI) [36]. We evaluated statistical heterogeneity across studies using the chi-square test (Cochrane Q) [37] and I2 statistic [38]. Statistical heterogeneity was significant if the p-value <0.1 and I2 ≥50% [39], and then, sensitivity analysis was introduced to test the robustness of the pooled results. Sensitivity analysis was conducted by using the leave-one-out strategy. Considering the fact that full elimination of variations between studies is impossible, we therefore used the random-effects model to conduct meta-analysis [40, 41]. Nevertheless, we simultaneously calculated all results based on the fixed-effects model to assess the robustness of all results by comparing them with those calculated from the random-effects model. A p-value <0.05 was considered statistically significant. In addition, we further evaluated the impact of transfusion thresholds on infants with VLBW and ELBW by excluding infants with LBW. Finally, we used a funnel plot to test the risk of publication bias although the accumulated number of eligible studies did not exceed 10 [42].
Results
Study search
A total of 624 records were captured from three electronic databases, and 1 study was identified from the previously published meta-analysis. Initially, 205 duplicate records and 27 registered records of clinical trials were automatically removed by EndNote software. Then, 377 unrelated records were excluded through screening their titles and abstracts. After screening full texts of the remaining 16 studies, we continued to exclude 4 ineligible studies due to unrelated to the topic (n=1), ineligible study design (n=1), letter to the editor (n=1), and narrative review (n=1). Finally, a total of 12 eligible studies [22,23,24, 29,30,31,32, 43,44,45,46,47] were included in the final analysis. The detailed process of the study retrieval and selection is shown in Fig. 1.
Characteristics of studies
Among 12 studies included in this meta-analysis, five studies [22, 29,30,31,32] were conducted in China, three studies [43, 44, 47] in the USA, three studies [23, 24, 46] in Canada, and one study [45] in Germany. Except for one study [44], other studies were published between 2005 and 2021. The sample size of the individual study ranged from 36 to 1824, with an accumulated number of 4380. Two studies [29, 30] enrolled anemic preterm infants with LBW, five studies [22, 31, 32, 43, 44] enrolled anemic preterm infants with VLBW, and the remaining five studies [23, 24, 45,46,47] enrolled anemic preterm infants with ELBW. The dose per transfusion of all eligible studies ranged from 10 to 20 ml/kg. Detailed baseline characteristics of 12 eligible studies are presented in Table 1. The transfusion thresholds for two transfusion strategies among all eligible studies are summarized in Table S2.
Risk of bias
All eligible studies were regarded as RCTs because the word “random” was mentioned; however, five studies [22, 29,30,31, 45] did not report the method of generating random sequences. In addition, only four studies [23, 43, 46, 47] reported the methods of concealing allocation. All studies were rated as “low” or “unclear” risk in performance bias, attrition bias, reporting bias, and other bias sources, but two studies were rated as “high” risk in detection bias. Generally, the overall methodological quality of 12 eligible studies is moderate.
Meta-analysis of physiological measurements
A total of 8 studies [22,23,24, 29, 43, 44, 46, 47] reported the level of hemoglobin after transfusion, and meta-analysis based on the random-effects model suggested that liberal transfusion threshold significantly increased the level of hemoglobin compared to restrictive transfusion threshold (MD: −10.03; 95%CI: −15.98 to −4.08; p=0.001). In addition, four studies [22, 29, 30, 43] reported hematocrit after transfusion, and meta-analysis suggested that liberal transfusion threshold was associated with increased hematocrit (MD: −3.62; 95%CI: −6.78 to −0.46; p=0.02). The results of physiological measurements are displayed in Fig. 2. The pooled result of hemoglobin (MD: −10.24; 95%CI: −11.34 to −9.14; p<0.001) and hematocrit (MD: −3.96; 95%CI: −5.32 to −2.59; p<0.001) was not significantly changed by the meta-analyses based on the fixed-effects model (Fig. S2). However, the difference between the two transfusion thresholds in hematocrit changed to be insignificant after excluding LBW infants (MD: −3.00; 95%CI: −8.97 to 2.98; p=0.33; Table 2).
Meta-analysis of transfusion-related indicators
Among 12 eligible studies, four [22, 29, 31, 43] and two [43, 46] studies reported age at first transfusion and donor exposure per infant between two groups, respectively. Meta-analysis based on the random-effects model suggested older age at first transfusion (MD: 5.08; 95%CI: 2.27 to 7.89; p=0.004) and lower donor exposure (MD: −0.52; 95%CI: −0.91 to −0.13; p=0.009) in anemic preterm infants treated by restrictive transfusion threshold (Fig. 3), which was consistent with the pooled results of meta-analyses based on the fixed-effects model (Fig. S3). Transfusion per infant and total transfusion volume were reported by seven [22, 23, 29,30,31, 43, 46] and three [22, 29, 31] studies, respectively. Meta-analysis based on the random-effects model suggested no statistical difference between restrictive and liberal transfusion thresholds for these two outcomes (Fig. 3); however, meta-analyses based on the fixed-effects model showed that restrictive transfusion threshold was better than liberal transfusion threshold in terms of these two outcomes (Fig. S3). It is noted that the exclusion of LBW preterm infants from the meta-analysis did not change the pooled results (Table 2).
Meta-analysis of clinical outcomes
Five [29, 31, 32, 43, 45], seven [22, 29,30,31,32, 43, 45], and ten [22, 23, 29,30,31,32, 43,44,45,46] studies reported time on supplemental oxygen, time on ventilator or CPAP, and length of hospital stay, respectively. Meta-analysis based on the random-effects model suggested that the restrictive transfusion threshold significantly prolonged the time on supplemental oxygen (MD: 3.56; 95%CI: 1.93 to 5.18; p<0.001) and ventilator or CPAP (MD: 3.31; 95%CI: 1.42 to 5.20; p=0.006), but had a comparable length of hospital stay between two thresholds (MD: −0.86; 95%CI: −2.84 to 1.12; p=0.39), which were not significantly changed after excluding LBW preterm infants (Table 2). Results of clinical outcomes are graphically reported in Fig. 4. However, meta-analyses based on the fixed-effects model showed that restrictive transfusion threshold was associated with significantly shortened length of hospital stay compared to liberal transfusion threshold (Fig. S2).
Meta-analysis of safety outcomes
A total of 13 safety outcomes were evaluated in this meta-analysis, and meta-analysis based on the random-effects model revealed no statistical difference between restrictive and liberal transfusion groups for any safety outcomes (Table 3), including the composite incidence of death and neurodevelopment impairment (p=0.87), overall mortality (p=0.91), the incidence of neurodevelopment impairment (p=0.34), bronchopulmonary dysplasia (p=0.40), necrotizing enterocolitis (p=0.36), any retinopathy of prematurity (p=0.26), retinopathy of prematurity with stage 3 or above (p=0.07), intraventricular hemorrhage (p=0.80), intraventricular hemorrhage with grade 3 or above (p=0.23), apnea (p=0.43), sepsis (p=0.81), periventricular leukomalacia (p=0.25), and patent ductus arteriosus (p=0.05). Furthermore, meta-analysis based on the fixed-effects model yielded consistent results, and results were not significantly reversed after the exclusion of LBW preterm infants (Table 3).
Sensitivity analysis
For physiological measurements, transfusion-related indicators, and clinical outcomes, we used the leave-one-out strategy to examine the robustness of pooled results because substantial statistical heterogeneity was detected for all analyses. As presented in Table 2, sensitivity analysis suggested that the pooled result of hematocrit, age at first transfusion, donor exposure per infant, total transfusion volume, and time on supplemental oxygen were significantly changed when leaving one study from meta-analysis each time.
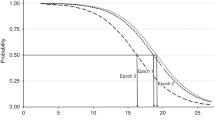
Publication bias
We created a funnel plot to evaluate the risk of publication bias for all outcomes qualitatively. As shown in Fig. 5, an asymmetric funnel plot was available for physiological measurements, indicating the risk of publication bias. However, symmetric funnel plots were available for transfusion-related indicators, clinical outcomes, and safety outcomes, suggesting the absence of publication bias for these outcomes.
Discussion
Summary of main findings
Red blood cell transfusions are commonly administered to anemic preterm infants, especially to those with VLBW and ELBW. Currently, two transfusion thresholds are available for red blood cell transfusion, including restrictive and liberal transfusion thresholds. Unfortunately, the comparative efficacy and safety of these two transfusion thresholds in anemic preterm infants remain controversial. In the current meta-analysis, a total of 4380 anemic preterm infants with LBW, VLBW, or ELBW were accumulated from 12 eligible studies. Although the comparability of the eligible studies included in this meta-analysis is limited by the high heterogeneity; pooled results remain revealing some promising findings. First, meta-analysis suggested both restrictive and liberal transfusion thresholds may be safe transfusion strategies because they are comparable in terms of safety. Second, liberal transfusion threshold may be more effective in improving the level of hemoglobin after transfusion and decreasing the need for supplemental oxygen, and shortening the time on ventilator or CPAP. Third, the differences in hematocrit, transfusion per infant, total transfusion volume, donor exposure per infant, and the length of hospital stay between the two transfusion thresholds required further validation by larger randomized multicenter studies because the pooled results are significantly changed after excluding LBW anemic preterm infants or changing analysis model from random-effects model to fixed-effects model.
Comparison with previous meta-analyses
Several meta-analyses [25,26,27,28] have compared the efficacy and safety of restrictive versus liberal transfusion thresholds. In 2014, Ibrahim et al. [25] firstly investigated the comparative effects of restrictive with liberal transfusion thresholds on clinical outcomes in VLBW infants, in which three studies involving 625 preterm infants were included. Finally, the authors found that restrictive transfusion was associated with less transfusion and donor exposure per infant, which were inconsistent with our findings. It is noted that limited eligible studies greatly impaired the robustness and reliability of the findings of this meta-analysis. Since then, in 2021, Wang and colleagues performed a systematic review and meta-analysis to further assess the efficacy and safety of restrictive versus liberal transfusion thresholds in VLBW infants [27]. It is noted that this meta-analysis included six studies with 3483 infants to evaluate more comprehensive outcomes, such as the level of hemoglobin after treatment and the composite incidence of death and neurodevelopment impairment, and reported no difference between restrictive and liberal transfusion thresholds for all target outcomes except for the level of hemoglobin, which were consistent with our findings. Unfortunately, other clinically important outcomes were not considered in this meta-analysis, such as transfusion-related indicators and time on ventilator or CPAP. In 2022, two meta-analyses [26, 28] published in the Chinese language also investigated the safety of restrictive versus liberal transfusion thresholds in VLBW infants. These two meta-analyses reported consistent results with our meta-analysis; however, the inclusion of limited eligible studies significantly decreased its reliability.
Compared with previous meta-analyses, the current study has three strengths. The methodology and data of this study are different from those of previous meta-analysis. First, we searched Chinese database to include more eligible studies in the final analysis, which benefits to increase the statistical power and then generate more robust and reliable findings. Second, we used random-effects model to conservatively estimate all results and used leave-one-out strategy to further exam the robustness of pooled results. Third, more comprehensive outcomes were considered in the current meta-analysis such as total transfusion volume, time on supplemental oxygen, and time on ventilator or CPAP. Therefore, results from this meta-analysis benefit to evaluate the efficacy and safety of restrictive and liberal transfusion thresholds more systematically.
Explanation of main findings
Red blood cell transfusions are commonly used to treat low hemoglobin levels in anemic preterm infants; however, a previous meta-analysis has described a correlation between red blood cell transfusion and the occurrence of retinopathy of prematurity in premature infants [48]. In the present meta-analysis, we did not find significant difference in the incidence of retinopathy of prematurity between two transfusion thresholds because transfusion per infant and total transfusion volume were comparable in both groups.
The proper use of oxygen may be lifesaving; however, excessive supplemental oxygen in preterm infants is a risk factor of retinopathy of prematurity, bronchopulmonary dysplasia, and longer hospital stay [49]. The current meta-analysis revealed that restrictive transfusion threshold was associated with prolonged time on supplemental oxygen in preterm infants; however, no difference was detected in the occurrence of retinopathy of prematurity and bronchopulmonary dysplasia and hospital stay. Studies indicated that if higher-grade retinopathy of prematurity is already present, the administration of oxygen to prevent relative retinal hypoxia while maintaining stage-dependent narrow oxygen saturation limits may minimize retinopathy of prematurity proliferation [50]. It is noted that eligible studies included in the present meta-analysis reported a wide range of tolerated Hb/Hct levels after transfusion, which might answer why the difference between the two strategies in the occurrence of retinopathy of prematurity and bronchopulmonary dysplasia does not achieve statistical significance. Moreover, sensitivity analysis significantly changed the result of time on supplemental oxygen; therefore, future studies are warranted to further evaluate this outcome.
In addition, iron deficiency [51, 52] has been demonstrated as an important risk factor for neurodevelopment; however, the incidence of neurodevelopment between restrictive and liberal transfusion thresholds was not significantly different although liberal transfusion kept significantly higher level of hemoglobin. Interestingly, evidence suggested that erythropoietin failed to improve neurodevelopmental outcomes despite the increase in red blood cells and hemoglobin concentration [53].
Limitations
Compared to previous meta-analyses, the current study has several strengths mentioned above, but several limitations should also be further explained. First, significant statistical heterogeneity was detected for physiological measurements, transfusion-related indicators, and clinical outcomes, and the level was not greatly decreased although sensitivity analysis with the leave-one-out strategy was conducted. Therefore, we could not eliminate the negative impact of variations in patient variables on our findings. Therefore, future study should especially ensure the homogeneity of the participants as much as possible. Second, there were differences across studies in birth weight; however, we designed two strategies to examine the robustness of pooled results, including the exclusion of LBW infants and the leave-one-out method (see Tables 2 and 3). Third, we detected the risk of publication bias for physiological measurements, which might have a negative impact on the pooled results. Certainly, we did not use the quantitative method (Egger and Begg tests) to test the symmetry of the funnel plot. Therefore, we could not eliminate the error of visual inspection. Fourth, there were differences across studies in the definition of thresholds (see Table S2); however, we did not conduct subgroup analysis to investigate the impact of different transfusion thresholds on outcomes because this strategy will further decrease the number of eligible studies included in the individual analysis, thereby greatly reducing the statistical power. Future studies may use the network meta-analysis to determine the comparative efficacy and safety of different transfusion thresholds in preterm infants when sufficient studies are published. Fifth, there are a limited number of eligible studies for certain outcomes, such as donor exposures per infant and total transfusion volume, so pooled results should be interpreted with caution due to insufficient statistical power. Sixth, we were unable to calculate concrete increases in hemoglobin and hematocrit values in individual studies because only two studies reported values before transfusion.
Conclusion
Liberal transfusion threshold significantly increases the level of hemoglobin and is associated with a shorter time on ventilator or CPAP in preterm infants. Moreover, liberal transfusion threshold most likely increases hematocrit and shortened the time on supplemental oxygen. Two transfusion thresholds were comparable for all safety outcomes. Overall, both liberal and restrictive transfusion thresholds are effective and safer strategies to red blood cell transfusion in anemic preterm infants, but liberal strategy is more effective in shortening the length of necessary respiratory support. Given the limitations of this meta-analysis, we suggest that more studies to validate our findings, especially the differences between the two transfusion thresholds in terms of hematocrit, transfusion per infant, total transfusion volume, donor exposure per infant, and the length of hospital stay.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Saito-Benz M, Bennington K, Gray CL, Murphy WG, Flanagan P, Steiner F, Atkinson G, Berry MJ (2022) Effects of Freshly Irradiated vs Irradiated and Stored Red Blood Cell Transfusion on Cerebral Oxygenation in Preterm Infants: A Randomized Clinical Trial. JAMA Pediatr 176:e220152–e220152. https://doi.org/10.1001/jamapediatrics.2022.0152
Kalteren WS, Verhagen EA, Mintzer JP, Bos AF, Kooi EMW (2021) Anemia and Red Blood Cell Transfusions, Cerebral Oxygenation, Brain Injury and Development, and Neurodevelopmental Outcome in Preterm Infants: A Systematic Review. Front Pediatr 9:644462. https://doi.org/10.3389/fped.2021.644462
Saito-Benz M, Flanagan P, Berry MJ (2020) Management of anaemia in pre-term infants. Br J Haematol 188:354–366. https://doi.org/10.1111/bjh.16233
Patel RM, Meyer EK, Widness JA (2016) Research Opportunities to Improve Neonatal Red Blood Cell Transfusion. Transfus Med Rev 30:165–173. https://doi.org/10.1016/j.tmrv.2016.06.005
Maier RF, Sonntag J, Walka MM, Liu G, Metze BC, Obladen M (2000) Changing practices of red blood cell transfusions in infants with birth weights less than 1000 g. J Pediatr 136:220–224. https://doi.org/10.1016/s0022-3476(00)70105-3
Fabres J, Wehrli G, Marques MB, Phillips V, Dimmitt RA, Westfall AO, Schelonka RL (2006) Estimating blood needs for very-low-birth-weight infants. Transfusion 46:1915–1920. https://doi.org/10.1111/j.1537-2995.2006.00997.x
Busch MP, Kleinman SH, Nemo GJ (2003) Current and emerging infectious risks of blood transfusions. Jama 289:959–962. https://doi.org/10.1001/jama.289.8.959
Luban NL (2005) Transfusion safety: Where are we today? Ann N Y Acad Sci 1054:325–341. https://doi.org/10.1196/annals.1345.040
Zagol K, Lake DE, Vergales B, Moorman ME, Paget-Brown A, Lee H, Rusin CG, Delos JB, Clark MT, Moorman JR, Kattwinkel J (2012) Anemia, apnea of prematurity, and blood transfusions. J Pediatr 161:417–421.e411. https://doi.org/10.1016/j.jpeds.2012.02.044
Abu Jawdeh EG, Martin RJ, Dick TE, Walsh MC, Di Fiore JM (2014) The effect of red blood cell transfusion on intermittent hypoxemia in ELBW infants. J Perinatol 34:921–925. https://doi.org/10.1038/jp.2014.115
Stockman JA 3rd, Clark DA (1984) Weight gain: a response to transfusion in selected preterm infants. Am J Dis Child 138:828–830. https://doi.org/10.1001/archpedi.1984.02140470028009
Christensen RD, Baer VL, Del Vecchio A, Henry E (2013) Unique risks of red blood cell transfusions in very-low-birth-weight neonates: associations between early transfusion and intraventricular hemorrhage and between late transfusion and necrotizing enterocolitis. J Matern Fetal Neonatal Med 26(Suppl 2):60–63. https://doi.org/10.3109/14767058.2013.830495
Baer VL, Lambert DK, Henry E, Snow GL, Butler A, Christensen RD (2011) Among very-low-birth-weight neonates is red blood cell transfusion an independent risk factor for subsequently developing a severe intraventricular hemorrhage? Transfusion 51:1170–1178. https://doi.org/10.1111/j.1537-2995.2010.02980.x
Hesse L, Eberl W, Schlaud M, Poets CF (1997) Blood transfusion. Iron load and retinopathy of prematurity. Eur J Pediatr 156:465–470. https://doi.org/10.1007/s004310050641
Dani C, Reali MF, Bertini G, Martelli E, Pezzati M, Rubaltelli FF (2001) The role of blood transfusions and iron intake on retinopathy of prematurity. Early Hum Dev 62:57–63. https://doi.org/10.1016/s0378-3782(01)00115-3
Hirano K, Morinobu T, Kim H, Hiroi M, Ban R, Ogawa S, Ogihara H, Tamai H, Ogihara T (2001) Blood transfusion increases radical promoting non-transferrin bound iron in preterm infants. Arch Dis Child Fetal Neonatal Ed 84:F188–F193. https://doi.org/10.1136/fn.84.3.f188
Collard KJ (2006) Is there a causal relationship between the receipt of blood transfusions and the development of chronic lung disease of prematurity? Med Hypotheses 66:355–364. https://doi.org/10.1016/j.mehy.2005.04.046
Mally P, Golombek SG, Mishra R, Nigam S, Mohandas K, Depalhma H, LaGamma EF (2006) Association of necrotizing enterocolitis with elective packed red blood cell transfusions in stable, growing, premature neonates. Am J Perinatol 23:451–458. https://doi.org/10.1055/s-2006-951300
Christensen RD, Lambert DK, Henry E, Wiedmeier SE, Snow GL, Baer VL, Gerday E, Ilstrup S, Pysher TJ (2010) Is “transfusion-associated necrotizing enterocolitis” an authentic pathogenic entity? Transfusion 50:1106–1112. https://doi.org/10.1111/j.1537-2995.2009.02542.x
dos Santos AM, Guinsburg R, de Almeida MF, Procianoy RS, Leone CR, Marba ST, Rugolo LM, Fiori HH, Lopes JM, Martinez FE (2011) Red blood cell transfusions are independently associated with intra-hospital mortality in very low birth weight preterm infants. J Pediatr 159:371-376.e371-373. https://doi.org/10.1016/j.jpeds.2011.02.040
Guillén U, Cummings JJ, Bell EF, Hosono S, Frantz AR, Maier RF, Whyte RK, Boyle E, Vento M, Widness JA, Kirpalani H (2012) International survey of transfusion practices for extremely premature infants. Semin Perinatol 36:244–247. https://doi.org/10.1053/j.semperi.2012.04.004
Chen HL, Tseng HI, Lu CC, Yang SN, Fan HC, Yang RC (2009) Effect of blood transfusions on the outcome of very low body weight preterm infants under two different transfusion criteria. Pediatr Neonatol 50:110–116. https://doi.org/10.1016/s1875-9572(09)60045-0
Kirpalani H, Bell EF, Hintz SR, Tan S, Schmidt B, Chaudhary AS, Johnson KJ, Crawford MM, Newman JE, Vohr BR et al (2020) Higher or Lower Hemoglobin Transfusion Thresholds for Preterm Infants. N Engl J Med 383:2639–2651. https://doi.org/10.1056/NEJMoa2020248
Whyte RK, Kirpalani H, Asztalos EV, Andersen C, Blajchman M, Heddle N, LaCorte M, Robertson CM, Clarke MC, Vincer MJ et al (2009) Neurodevelopmental outcome of extremely low birth weight infants randomly assigned to restrictive or liberal hemoglobin thresholds for blood transfusion. Pediatrics 123:207–213. https://doi.org/10.1542/peds.2008-0338
Ibrahim M, Ho SK, Yeo CL (2014) Restrictive versus liberal red blood cell transfusion thresholds in very low birth weight infants: a systematic review and meta-analysis. J Paediatr Child Health 50:122–130. https://doi.org/10.1111/jpc.12409
Liu Y, Zhuang Y, Lv B, Liao JR (2022) Long-term effects of liberal versus restricted red blood cell transfusions in extremely low birth weight infants: a meta analysis. Chin J Neonatol 37:59–64. https://doi.org/10.3760/cma.j.issn.2096-2932.2022.01.014
Wang P, Wang X, Deng H, Li L, Chong W, Hai Y, Zhang Y (2021) Restrictive versus liberal transfusion thresholds in very low birth weight infants: A systematic review with meta-analysis. PLoS One 16:e0256810. https://doi.org/10.1371/journal.pone.0256810
Zhang YS, Zheng WW, Liu CQ (2022) Effects of liberal versus restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: a systematic review and meta-analysis of randomized trials. J Clin Transfus Lab Med 24:211–218. https://doi.org/10.3969/j.issn.1671-2587.2022.02.016
Fan Y, Zhang MR, Jiang TH (2021) Comparative effectiveness of restrictive and liberal blood transfusion therapy in the treatment of anemia in premature infants. Shandong Med J 61:69–72
Liu Y, Wang LJ, Han MQ (2012) The effect of different transfusion measures on the clinical outcome in preterm infants. Chin J Primary Med Pharm 2096-2097. https://doi.org/10.3760/cma.j.issn.1008-6706.2012.14.008
Wang BH, Wu YM, Wang KX, Guo JJ, Zhang X (2013) The effect of the restrictive transfusion and non-restrictive transfusion on clinical outcome of very low birth weight (VLBW) premature infants with anemia disease. J Chin Phys 15:1666–1669. https://doi.org/10.3760/cma.j.issn.1008-1372.2013.12.022
Wu SM, Yang ZZ, Zhou JM (2017) Analysis of the comparative effectiveness of different transfusion strategies for the treatment of extremely low-birth weight infants with severe anemia. Inner Mongolia Med J 49:212–213. https://doi.org/10.16096/J.cnki.nmgyxzz.2017.49.02.035
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Bowden J, Tierney JF, Copas AJ, Burdett S (2011) Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol 11:41. https://doi.org/10.1186/1471-2288-11-41
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Spineli LM, Pandis N (2020) Meta-analysis: Random-effects model. Am J Orthod Dentofac Orthop 157:280–282. https://doi.org/10.1016/j.ajodo.2019.10.007
Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1:97–111. https://doi.org/10.1002/jrsm.12
Palma Perez S, Delgado Rodriguez M (2006) Practical considerations on detection of publication bias. Gac Sanit 20(Suppl 3):10–16. https://doi.org/10.1157/13101085
Bell EF, Strauss RG, Widness JA, Mahoney LT, Mock DM, Seward VJ, Cress GA, Johnson KJ, Kromer IJ, Zimmerman MB (2005) Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics 115:1685–1691. https://doi.org/10.1542/peds.2004-1884
Blank J, Sheagren T, Vajaria J, Mangurten H, Benawra R, Puppala B (1984) The role of RBC transfusion in the premature infant. Am J Dis Child 138:831–833. https://doi.org/10.1001/archpedi.1984.02140470031010
Franz AR, Engel C, Bassler D, Rüdiger M, Thome UH, Maier RF, Krägeloh-Mann I, Kron M, Essers J, Bührer C, Rellensmann G, Rossi R, Bittrich HJ, Roll C, Höhn T, Ehrhardt H, Avenarius S, Körner HT, Stein A et al (2020) Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: The ETTNO randomized clinical trial. JAMA 324:560–570. https://doi.org/10.1001/jama.2020.10690
Kirpalani H, Whyte RK, Andersen C, Asztalos EV, Heddle N, Blajchman MA, Peliowski A, Rios A, LaCorte M, Connelly R et al (2006) The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 149:301–307. https://doi.org/10.1016/j.jpeds.2006.05.011
Widness JA, Madan A, Grindeanu LA, Zimmerman MB, Wong DK, Stevenson DK (2005) Reduction in red blood cell transfusions among preterm infants: results of a randomized trial with an in-line blood gas and chemistry monitor. Pediatrics 115:1299–1306. https://doi.org/10.1542/peds.2004-1680
Zhu Z, Hua X, Yu Y, Zhu P, Hong K, Ke Y (2020) Effect of red blood cell transfusion on the development of retinopathy of prematurity: A systematic review and meta-analysis. PLoS One 15:e0234266. https://doi.org/10.1371/journal.pone.0234266
Parmar J, Pawar V, Warathe A, Singh M, Bajaj R, Kumar J, Thukral A, Chawla D, Kumar P, Deorari A (2021) Rationalising oxygen usage in a level II special newborn care unit in Madhya Pradesh, India. BMJ Open Qual 10. https://doi.org/10.1136/bmjoq-2021-001386
Ryu J (2022) New Aspects on the Treatment of Retinopathy of Prematurity: Currently Available Therapies and Emerging Novel Therapeutics. Int J Mol Sci 23. https://doi.org/10.3390/ijms23158529
Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW (2000) Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 105:E51. https://doi.org/10.1542/peds.105.4.e51
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK (2007) The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology 92:73–82. https://doi.org/10.1159/000100805
Juul SE, Comstock BA, Wadhawan R, Mayock DE, Courtney SE, Robinson T, Ahmad KA, Bendel-Stenzel E, Baserga M, LaGamma EF, Downey LC, Rao R, Fahim N, Lampland A, Frantz Iii ID, Khan JY, Weiss M, Gilmore MM, Ohls RK et al (2020) A Randomized Trial of Erythropoietin for Neuroprotection in Preterm Infants. N Engl J Med 382:233–243. https://doi.org/10.1056/NEJMoa1907423
Funding
This study was supported by the Hainan Provincial Natural Science Foundation of China (822QN491) and Hainan Province Clinical Medical Center (QWYH202175).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Xiaoling Fu
(II) Administrative support: Xingdan Zhao
(III) Provision of study materials or patients: Xingdan Zhao
(IV) Collection and assembly of data: Aihan Weng
(V) Data analysis and interpretation: Qian Zhang
(VI) Manuscript writing: All authors
(VII) Final approval of manuscript: All authors
Corresponding author
Ethics declarations
Ethics approval
This article is a meta-analysis. The data comes from published articles and does not require ethical approval and written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information

Figure S1.
Risk of bias summary (a) and graph (b). (PNG 729 kb)

Figure S2.
Fixed-effects meta-analysis of physiological measurements between restrictive and liberal transfusion thresholds. SD, standard difference; IV, inverse variance; CI, confidence interval. (PNG 766 kb)

Figure S3.
Fixed-effects meta-analysis of transfusion-related indicators between restrictive and liberal transfusion thresholds. SD, standard difference; IV, inverse variance; CI, confidence interval. (PNG 1136 kb)

Figure S4.
Fixed-effects meta-analysis of clinical outcomes between restrictive and liberal transfusion thresholds. CPAP, continuous positive airway pressure; SD, standard difference; IV, inverse variance; CI, confidence interval. (PNG 1270 kb)
Table S1.
Detailed search strategy. (DOCX 21 kb)
Table S2.
Transfusion thresholds for two transfusion strategies among all eligible studies. (DOCX 18 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fu, X., Zhao, X., Weng, A. et al. Comparative efficacy and safety of restrictive versus liberal transfusion thresholds in anemic preterm infants: a meta-analysis of 12 randomized controlled trials. Ann Hematol 102, 283–297 (2023). https://doi.org/10.1007/s00277-022-05072-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-05072-7