Abstract
The nutritional risk index (NRI), which is based on weight and albumin levels, is closely associated with the prognosis of many cancers. However, its prognostic value has not been investigated in patients with newly diagnosed multiple myeloma (NDMM). We aimed to assess the association between the NRI and survival outcomes in patients with NDMM. We retrospectively collected and analyzed clinical and laboratory data from patients with NDMM between 2005 and 2019 at our center. Patients were stratified into the high NRI (> 89) and low NRI (≤ 89) groups for prognostic analysis. The NRI and other variables were also explored to evaluate their prognostic value for overall survival (OS). A total of 638 patients diagnosed with NDMM were retrospectively included. Patients in the high NRI group had a significantly better median OS than those in the low NRI group (64 months vs 43 months, p < 0.001). In the multivariate analysis, a high NRI was shown to be an independent prognostic factor for OS (hazard ratio, 0.758; 95% confidence interval, 0.587–0.977; p = 0.033). Age, performance status, transplant status, and lactate dehydrogenase level were also independent prognostic factors for OS. In conclusion, our study demonstrates that the NRI is a simple and useful predictor of survival outcomes in patients with NDMM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is the second most common hematologic cancer in high-income countries and is characterized by the accumulation of monoclonal plasma cells in bone marrow and the production of immunoglobulin [1]. Because of the heterogeneity of MM, patient survival ranges from a few months to over 10 years []. Therefore, no single staging system can be used for all patients with MM, and several staging systems have been developed to predict prognosis and help risk stratification for patients with MM, including the Durie–Salmon (DS) staging system, international staging system (ISS), revised ISS (R-ISS), and Mayo Stratification of Myeloma and Risk-Adapted Therapy. All of these staging systems are based on two or three unfavorable prognostic variables [4567]. Furthermore, an increasing number of cytogenetic and non-cytogenetic parameters have been explored to investigate their potential impact on MM prognosis.
In the era of novel drug development, the survival of patients with MM has been notably improved [8]. However, some patients with MM still do not obtain survival benefits from these drugs, and this phenomenon cannot be fully explained by biological and genetic prognostic factors [9, 10]. Treatment-related complications may explain the variability in overall survival (OS) in patients with MM.
Malnutrition is common in cancer patients, with an incidence ranging from 30 to 80% [11, 12]. Kim et al. reported that the malnutrition prevalence in MM was about 70% [13]. Some studies have found that malnutrition is highly associated with worse survival in cancer patients [13,14,15]. Further, malnutrition is related to the response to treatment and the occurrence of chemotherapy-related adverse events, which decrease survival [16,17,18,19]. The nutritional risk index (NRI), which is based on weight and albumin levels, is closely associated with prognosis in many cancers [20, 21]. However, its prognostic value for newly diagnosed MM (NDMM) has not been investigated.
Therefore, in this retrospective study, we aimed to investigate the association between the NRI and survival outcomes of NDMM patients.
Patients and methods
Patients
Patients diagnosed with NDMM between 2005 and 2019 at the Sun Yat-sen University Cancer Center (SYSUCC) were eligible for inclusion in this study. Baseline clinical and laboratory data were extracted from electronic medical records, including age, sex, disease stage, performance status, transplant status, weight, and β2-microglobulin (β2-MG), lactate dehydrogenase (LDH), C-reactive protein (CRP), creatinine (CRE), hemoglobin (HGB), albumin, and calcium (Ca) levels. The inclusion criteria were age older than 18 years and availability of complete baseline clinical and laboratory data (items noted above). Patients receiving only palliative treatment, those lost to follow-up, and those lacking baseline data were excluded from our study. The final follow-up was January 2022. Our study was approved by the institutional ethics committee of the SYSUCC. Our study was retrospective; therefore, the requirement for informed consent was waived.
Statistical analyses
The NRI was calculated as follows: 1.489 × albumin (g/L) + 41.7 × (weight/usual body weight) [20, 21]. The cutoff value of the NRI was determined using maximally selected rank statistics; patients with an NRI > 89 were defined as the high NRI group, and the remaining patients were categorized into the low NRI group. Differences between the two groups were determined using the chi-square test or Fisher’s exact test. OS was defined as the interval between diagnosis and death due to any cause. The Kaplan–Meier method was used to estimate OS, and comparisons between groups were performed using the log-rank test. Univariate Cox regression analysis of OS was used to evaluate the prognostic value of the variables. Variables with p < 0.05 were included in a stepwise multivariate Cox regression analysis. A two-sided p value < 0.05 was regarded as significant. All statistical analyses were performed using R version 4.0.3 (The R Foundation, Vienna, Austria).
Results
Baseline characteristics
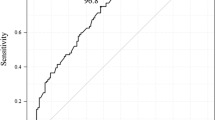
A total of 638 eligible patients were enrolled in this study. The median age of the entire cohort was 60 years (interquartile range [IQR], 53–66 years). The median ages of the high and low NRI groups were 59 years (IQR, 53–66 years) and 62 years (IQR, 57–68 years), respectively. Three hundred and eighty-seven (60.2%) patients were men. There were no significant differences in sex or LDH, CRE, or Ca levels between the two groups. However, patients in the low NRI group were more likely to be older, have more advanced tumor stage, and have lower performance status and lower levels of β2-MG, CRP, and HGB and less likely to have undergone transplantation than those in the high NRI group; the differences were statistically significant. The median OS in the entire cohort was 58 months (5-year OS, 47.8%; 95% confidence interval [CI], 43.0–53.1; Fig. 1a). The baseline patient characteristics are presented in Table 1.
Prognostic value of the DS staging system, ISS, R-ISS, and NRI for OS in MM patients
The DS staging system reflects tumor burden and does not predict the prognosis of MM; however, we evaluated its prognostic value in patients with NDMM in our study. The differences in OS between the groups were not significant (p = 0.26, Fig. 1b). Because the ISS and R-ISS staging systems have prognostic value in patients with MM, we explored their prognostic value in the entire cohort [5, 6]. The median OS of patients with ISS stages I, II, and III were 110 months, 53 months, and 45 months, respectively (p < 0.001, Fig. 1c). The median OS of patients with R-ISS stages I, II, and III were not reached, 57 months, and 25 months, respectively (p < 0.0001; Fig. 1d). Therefore, both the ISS and R-ISS staging systems predicted clinical outcome in this cohort.
We also assessed the prognostic ability of the NRI. The median OS of the low NRI group was 43 months (95% CI, 35–62 months), which was significantly shorter than that of the high NRI group (64 months; 95% CI, 56–93 months; p < 0.001; Fig. 1).
Univariate and multivariate analyses of OS
In the univariate analysis of OS, older age (> 50 years; hazard ratio [HR], 1.838; 95% CI, 1.264–2.673; p = 0.001), poor performance status (Eastern Cooperative Oncology Group [ECOG] performance status score ≥ 2; HR, 2.096; 95% CI, 1.513–2.904; p < 0.001), high serum β2-MG (> 3.5 g/L; HR, 1.700; 95% CI, 1.322–2.186; p < 0.001), high serum LDH (HR, 2.069; 95% CI, 1.583–2.704; p < 0.001), high serum CRP (HR, 1.511; 95% CI, 1.185–1.926; p < 0.001), and high serum Ca (HR, 1.524; 95% CI, 1.089–2.135; p = 0.014) levels were significantly associated with worse OS in the entire cohort. Undergoing transplantation (HR, 0.368; 95% CI, 0.222–0.610; p < 0.001), high HGB level (HR, 0.565; 95% CI, 0.414–0.772; p < 0.001), and a high NRI (> 89; HR, 0.597; 95% CI, 0.468–0.760; p < 0.001) were significantly associated with better OS. However, in the multivariate analysis, only older age (HR, 1.509; 95% CI, 1.028–2.215; p = 0.008), ECOG performance status score ≥ 2 (HR, 2.096; 95% CI, 1.513–2.904; p < 0.001), undergoing transplantation (HR, 0.497; 95% CI, 0.297–0.833; p = 0.008), high serum LDH level (HR, 1.710; 95% CI, 1.297–2.253; p < 0.001), and a high NRI (HR, 0.758; 95% CI, 0.587–0.977; p = 0.033) were identified as independent prognostic factors in NDMM patients. Table 2 shows the results of the univariate and multivariate analyses of OS.
The survival curves for the five independent prognostic factors are shown in Fig. 2. The median OS were 64 months (5-year OS, 51.0%; 95% CI, 45.0–57.7) and 43 months (5-year OS, 41.4%; 95% CI, 33.9–50.5; p < 0.001) in the high and low NRI groups, respectively.
Discussion
Our study revealed that the NRI might be an independent prognostic factor of OS in patients with NDMM. Further, older age, ECOG performance status score ≥ 2, undergoing transplantation, and high serum LDH level were also independent prognostic factors for OS in NDMM patients. Patients in the high NRI group had a significantly better OS than those in the low NRI group. Consistent with the results of previous studies in other cancers, our results suggest that malnutrition, as assessed by the NRI, may be a predictor of poor survival in patients with NDMM [22,23,24].
The NRI is a comprehensive index based on albumin and weight and has been widely used in recent years to assess prognosis in cancer [25]. In our study, a low NRI was associated with a shorter OS. Based on the formula for calculating the NRI, a low NRI can indicate either low albumin levels or low weight. In our study, the proportion of patients with a poor performance status (ECOG performance status score ≥ 2) at diagnosis was significantly higher in the low NRI group than in the high NRI group. Patients in the low NRI group also had lower serum HGB levels than those in the high NRI group. This may be related to poor tolerance to chemotherapy and may, in part, explain the unfavorable survival outcomes. Moreover, only 8.1% of patients in the low NRI group received transplants. This implies that a low NRI is associated with poor tolerance to intensive chemotherapy. Better treatment tolerance allows for the prescription of higher doses of chemotherapy, thus improving survival. In addition, in our study, patients in the low NRI group were significantly more likely to be older and have high β2-MG levels, high CRP levels, and advanced disease than those in the high NRI group, which may also account for the worse survival outcomes in the low NRI group.
Albumin, a major protein in human serum, has been used to evaluate nutritional status, and low albumin levels have been shown to be related to poor prognosis in patients with various cancers [26,27,28]. In hematologic cancers, albumin has also been shown to be a strong predictor of prognosis and is one of the factors in the ISS [5]. Albumin can potentially carry a high amount of active antitumor compounds to the tumor site via albumin association [29]. Consequently, low albumin levels lead to a decreased probability of active antitumor compounds at the tumor site, which may be one of the reasons a low NRI was associated with poor prognosis. Low albumin levels can also cause high concentrations of certain drugs that cannot be converted into harmless substances, leading to toxicity over time; therefore, patients will suffer from severe adverse effects that can account for poor prognosis.
Obesity has been regarded as a risk factor for survival in many types of cancer, but some studies have shown that a low baseline BMI is also associated with poor survival in patients with cancer [30,31,32]. Unintended weight loss is commonly a sign of cancer and a negative predictor of survival. One retrospective study reported that a loss (> 5%) of premorbid weight before chemotherapy implied poor prognosis, independent of tumor stage, histology, and performance status [19]. Although multiple studies have examined the influence of obesity on the prognosis of various cancers, few studies have examined the influence of being underweight on the prognosis of patients with MM. A Korean study reported that a low baseline BMI was associated with poor prognosis in patients with MM. Western countries have a higher proportion of obese patients than Asian countries; therefore, being underweight may play a more critical role than being obese in predicting the prognosis of Asian patients with MM.
Our study has some limitations. First, it was a retrospective study. Second, the study was performed in a single center and not in multiple centers. Third, we did not explore the potential mechanism by which the NRI affects the prognosis of NDMM. Therefore, further studies with larger sample sizes are required to verify the results.
In conclusion, we found that the NRI might be a prognostic factor for NDMM. The NRI is easy to acquire and could be a simple and useful implement for forecasting the prognosis of NDMM. Further multicenter investigations are needed to confirm these findings.
Data availability
The data supporting our study will be available by contacting the corresponding authors for reasonable reasons.
References
van de Donk N, Pawlyn C, Yong KL (2021) Multiple myeloma. Lancet 397:410–427. https://doi.org/10.1016/s0140-6736(21)00135-5
Cowan AJ, Green DJ, Kwok M, Lee S, Coffey DG, Holmberg LA, Tuazon S, Gopal AK, Libby EN (2022) Diagnosis and management of multiple myeloma: a review. JAMA 327:464–477. https://doi.org/10.1001/jama.2022.0003
Perrot A, Lauwers-Cances V, Tournay E, Hulin C, Chretien ML, Royer B, Dib M, Decaux O, Jaccard A, Belhadj K, Brechignac S, Fontan J, Voillat L, Demarquette H, Collet P, Rodon P, Sohn C, Lifermann F, Orsini-Piocelle F, Richez V, Mohty M, Macro M, Minvielle S, Moreau P, Leleu X, Facon T, Attal M, Avet-Loiseau H, Corre J (2019) Development and validation of a cytogenetic prognostic index predicting survival in multiple myeloma. J Clin Oncol 37:1657–1665. https://doi.org/10.1200/jco.18.00776
Durie BG, Salmon SE (1975) A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer 36:842–854. https://doi.org/10.1002/1097-0142(197509)36:3%3c842::aid-cncr2820360303%3e3.0.co;2-u
Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Bladé J, Boccadoro M, Child JA, Avet-Loiseau H, Kyle RA, Lahuerta JJ, Ludwig H, Morgan G, Powles R, Shimizu K, Shustik C, Sonneveld P, Tosi P, Turesson I, Westin J (2005) International staging system for multiple myeloma. J Clin Oncol 23:3412–3420. https://doi.org/10.1200/jco.2005.04.242
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, Richardson P, Caltagirone S, Lahuerta JJ, Facon T, Bringhen S, Gay F, Attal M, Passera R, Spencer A, Offidani M, Kumar S, Musto P, Lonial S, Petrucci MT, Orlowski RZ, Zamagni E, Morgan G, Dimopoulos MA, Durie BG, Anderson KC, Sonneveld P, San Miguel J, Cavo M, Rajkumar SV, Moreau P (2015) Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol 33:2863–2869. https://doi.org/10.1200/jco.2015.61.2267
Kumar SK, Mikhael JR, Buadi FK, Dingli D, Dispenzieri A, Fonseca R, Gertz MA, Greipp PR, Hayman SR, Kyle RA, Lacy MQ, Lust JA, Reeder CB, Roy V, Russell SJ, Short KE, Stewart AK, Witzig TE, Zeldenrust SR, Dalton RJ, Rajkumar SV, Bergsagel PL (2009) Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines. Mayo Clin Proc 84:1095–1110. https://doi.org/10.4065/mcp.2009.0603
Okamoto S, Ureshino H, Kidoguchi K, Kusaba K, Kizuka-Sano H, Sano H, Nishioka A, Yamaguchi K, Kamachi K, Itamura H, Yoshimura M, Yokoo M, Shindo T, Kubota Y, Ando T, Kojima K, Kawaguchi A, Sueoka E, Kimura S (2020) Clinical impact of the CONUT score in patients with multiple myeloma. Ann Hematol 99:113–119. https://doi.org/10.1007/s00277-019-03844-2
Chng WJ, Dispenzieri A, Chim CS, Fonseca R, Goldschmidt H, Lentzsch S, Munshi N, Palumbo A, Miguel JS, Sonneveld P, Cavo M, Usmani S, Durie BG, Avet-Loiseau H (2014) IMWG consensus on risk stratification in multiple myeloma. Leukemia 28:269–277. https://doi.org/10.1038/leu.2013.247
Lenhoff S, Hjorth M, Westin J, Brinch L, Bäckström B, Carlson K, Christiansen I, Dahl IM, Gimsing P, Hammerström J, Johnsen HE, Juliusson G, Linder O, Mellqvist UH, Nesthus I, Nielsen JL, Tangen JM, Turesson I (2006) Impact of age on survival after intensive therapy for multiple myeloma: a population-based study by the Nordic Myeloma Study Group. Br J Haematol 133:389–396. https://doi.org/10.1111/j.1365-2141.2006.06042.x
Ramos Chaves M, Boléo-Tomé C, Monteiro-Grillo I, Camilo M, Ravasco P (2010) The diversity of nutritional status in cancer: new insights. Oncologist 15:523–530. https://doi.org/10.1634/theoncologist.2009-0283
Isenring E, Cross G, Kellett E, Koczwara B, Daniels L (2010) Nutritional status and information needs of medical oncology patients receiving treatment at an Australian public hospital. Nutr Cancer 62:220–228. https://doi.org/10.1080/01635580903305276
Kim HS, Lee JY, Lim SH, Cho J, Kim SJ, Jang JH, Kim WS, Jung CW, Kim K (2017) Patient-Generated Subjective Global Assessment as a prognosis tool in patients with multiple myeloma. Nutrition 36:67–71. https://doi.org/10.1016/j.nut.2016.06.009
Xu J, Jie Y, Sun Y, Gong D, Fan Y (2022) Association of Global Leadership Initiative on Malnutrition with survival outcomes in patients with cancer: a systematic review and meta-analysis. Clin Nutr 41:1874–1880. https://doi.org/10.1016/j.clnu.2022.07.007
Zhang X, Pang L, Sharma SV, Li R, Nyitray AG, Edwards BJ (2021) Malnutrition and overall survival in older patients with cancer. Clin Nutr 40:966–977. https://doi.org/10.1016/j.clnu.2020.06.026
Go SI, Park S, Kang MH, Kim HG, Kim HR, Lee GW (2019) Clinical impact of prognostic nutritional index in diffuse large B cell lymphoma. Ann Hematol 98:401–411. https://doi.org/10.1007/s00277-018-3540-1
Baumgartner A, Bargetzi A, Zueger N, Bargetzi M, Medinger M, Bounoure L, Gomes F, Stanga Z, Mueller B, Schuetz P (2017) Revisiting nutritional support for allogeneic hematologic stem cell transplantation—a systematic review. Bone Marrow Transplant 52:506–513. https://doi.org/10.1038/bmt.2016.310
Maltoni M, Caraceni A, Brunelli C, Broeckaert B, Christakis N, Eychmueller S, Glare P, Nabal M, Viganò A, Larkin P, De Conno F, Hanks G, Kaasa S (2005) Prognostic factors in advanced cancer patients: evidence-based clinical recommendations—a study by the Steering Committee of the European Association for Palliative Care. J Clin Oncol 23:6240–6248. https://doi.org/10.1200/jco.2005.06.866
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass HO Jr, Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69:491–497. https://doi.org/10.1016/s0149-2918(05)80001-3
Lee S, Fujita K, Morishita T, Negoro E, Oiwa K, Tsukasaki H, Yamamura O, Ueda T, Yamauchi T (2021) Prognostic utility of a geriatric nutritional risk index in combination with a comorbidity index in elderly patients with diffuse large B cell lymphoma. Br J Haematol 192:100–109. https://doi.org/10.1111/bjh.16743
Buzby GP, Knox LS, Crosby LO, Eisenberg JM, Haakenson CM, McNeal GE, Page CP, Peterson OL, Reinhardt GF, Williford WO (1988) Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am J Clin Nutr 47(2 Suppl):366–381. https://doi.org/10.1093/ajcn/47.2.366
Przekop Z, Szostak-Węgierek D, Milewska M, Panczyk M, Zaczek Z, Sobocki J (2022) Efficacy of the Nutritional Risk Index, Geriatric Nutritional Risk Index, BMI, and GLIM-defined malnutrition in predicting survival of patients with head and neck cancer patients qualified for home enteral nutrition. Nutrients 14(6):1268. https://doi.org/10.3390/nu14061268
Xie H, Ruan G, Zhang Q, Ge Y, Song M, Zhang X, Liu X, Lin S, Zhang X, Li X, Zhang K, Yang M, Tang M, Cong M, Shi H (2022) Combination of nutritional risk index and handgrip strength on the survival of patients with cancer cachexia: a multi-center cohort study. J Inflamm Res 15:1005–1015. https://doi.org/10.2147/jir.S352250
Li WZ, Hua X, Lv SH, Liang H, Liu GY, Lu N, Bei WX, Xia WX, Xiang YQ (2021) A scoring system based on nutritional and inflammatory parameters to predict the efficacy of first-line chemotherapy and survival outcomes for de novo metastatic nasopharyngeal carcinoma. J Inflamm Res 14:817–828. https://doi.org/10.2147/jir.S296710
Nishi I, Seo Y, Hamada-Harimura Y, Yamamoto M, Ishizu T, Sugano A, Sato K, Sai S, Obara K, Suzuki S, Koike A, Aonuma K, Ieda M (2019) Geriatric nutritional risk index predicts all-cause deaths in heart failure with preserved ejection fraction. ESC Heart Fail 6:396–405. https://doi.org/10.1002/ehf2.12405
McMillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, McArdle CS (2001) Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer 39:210–213. https://doi.org/10.1207/S15327914nc392_8
Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J (2013) The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty 28:21–24. https://doi.org/10.1016/j.arth.2013.05.038
Conrad LB, Awdeh H, Acosta-Torres S, Conrad SA, Bailey AA, Miller DS, Lea JS (2018) Pre-operative core muscle index in combination with hypoalbuminemia is associated with poor prognosis in advanced ovarian cancer. J Surg Oncol 117:1020–1028. https://doi.org/10.1002/jso.24990
Aguilera-Garrido A, Del Castillo-Santaella T, Yang Y, Galisteo-González F, Gálvez-Ruiz MJ, Molina-Bolívar JA, Holgado-Terriza JA, Cabrerizo-Vílchez M, Maldonado-Valderrama J (2021) Applications of serum albumins in delivery systems: differences in interfacial behaviour and interacting abilities with polysaccharides. Adv Colloid Interface Sci 290:102365. https://doi.org/10.1016/j.cis.2021.102365
Waalkes S, Merseburger AS, Kramer MW, Herrmann TR, Wegener G, Rustemeier J, Hofmann R, Schrader M, Kuczyk MA, Schrader AJ (2010) Obesity is associated with improved survival in patients with organ-confined clear-cell kidney cancer. Cancer Causes Control 21:1905–1910. https://doi.org/10.1007/s10552-010-9618-2
Yang R, Cheung MC, Pedroso FE, Byrne MM, Koniaris LG, Zimmers TA (2011) Obesity and weight loss at presentation of lung cancer are associated with opposite effects on survival. J Surg Res 170:e75-83. https://doi.org/10.1016/j.jss.2011.04.061
Carson KR, Bartlett NL, McDonald JR, Luo S, Zeringue A, Liu J, Fu Q, Chang SH, Colditz GA (2012) Increased body mass index is associated with improved survival in United States veterans with diffuse large B-cell lymphoma. J Clin Oncol 30:3217–3222. https://doi.org/10.1200/jco.2011.39.2100
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C (2005) Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 82:777–783. https://doi.org/10.1093/ajcn/82.4.777
Funding
YW is supported by the National Natural Science Foundation of China (Grant No. 82100184), Natural Science Foundation of Guangdong (Grant No. 2022A1515012521), Science and Technology Planning Project of Guanzhou (Grant No. 202201010919), and Beijing Xisike Clinical Oncology Research Foundation (Y-Young2022–0281). YL is supported by Sun Yat-sen University Start-up Funding (Grant No. 201603), the Program for Guangdong Introducing Innovative and Entrepreneurial Teams (Grant No. 2017ZT07S096), and the National Natural Science Foundation of China (Grant No. 81873428).
Author information
Authors and Affiliations
Contributions
WY and YL designed the study. LMZ and MYH collected and analyzed the data. LMZ, SZC, and MYH wrote and revised the manuscript. All authors contributed to data analysis, drafting, or revising the article; agreed to the journal to which the article will be submitted; gave final approval of the version to be published; and agreed to be accountable for all aspects of this work.
Corresponding authors
Ethics declarations
Ethical approval
Our study was approved by the institutional ethics committee of the SYSUCC.
Informed consent
Because this was a retrospective study, the requirement for informed consent was waived.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, L., Chen, S., Huang, M. et al. Prognostic value of the nutritional risk index in patients with newly diagnosed multiple myeloma. Ann Hematol 102, 125–132 (2023). https://doi.org/10.1007/s00277-022-05059-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-05059-4