Abstract
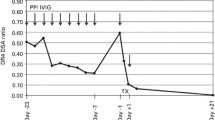
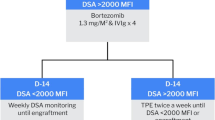
Donor-specific anti-human leukocyte antigen (HLA) antibody (DSA) is associated with a higher incidence of graft failure and mortality in HLA-mismatched allograft settings. However, the optimal protocol of desensitization for patients with positive DSA remains uncertain. We investigated the effectiveness of a desensitization protocol, including rituximab, high-dose intravenous immunoglobulin (IVIG), and a single session of plasma exchange (PE), for haploidentical allograft recipients with a high mean fluorescence intensity (MFI) level of DSA (≥ 5,000). Eleven patients with hematological disease who had positive DSA (median, 11,676, range 5387–20,435) were desensitized by the protocol. All of the patients achieved hematopoietic recovery. The median times for neutrophil and platelet engraftment were 13 (range, 11–26) days and 19 (range, 11–90) days, respectively. Grade II–IV acute graft-versus-host disease (GVHD) was seen in one patient and was controlled completely. Chronic cutaneous GVHD was seen in eight patients. Nine patients are alive with good performance so far. One patient suffered extramedullary relapse, and one patient died of transplantation-associated thrombotic microangiopathy. The 1-year probability of overall survival was 81.8%. These results suggest that successful desensitization could be obtained by a combination of rituximab, high-dose IVIG, and PE for haploidentical allograft recipients with high MFI levels of DSA.

Similar content being viewed by others
References
Ciurea SO, Thall PF, Milton DR et al (2015) Complement-binding donor-specific anti-hla antibodies and risk of primary graft failure in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 21(8):1392–1398
Spellman S, Bray R, Rosen-Bronson S et al (2010) The detection of donor-directed, HLA-specific alloantibodies in recipients of unrelated hematopoietic cell transplantation is predictive of graft failure. Blood 115(13):2704–2708
Bramanti S, Calafiore V, Longhi E et al (2019) Donor-specific anti-HLA antibodies in haploidentical stem cell transplantation with post-transplantation cyclophosphamide: risk of graft failure, poor graft function, and impact on outcomes. Biol Blood Marrow Transplant 25(7):1395–1406
Fuji S, Oshima K, Ohashi K et al (2020) Impact of pretransplant donor-specific anti-HLA antibodies on cord blood transplantation on behalf of the Transplant Complications Working Group of Japan Society for Hematopoietic Cell Transplantation. Bone Marrow Transplant 55(4):722–728
Morin-Zorman S, Loiseau P, Taupin J-L et al (2016) Donor-specific anti-HLA antibodies in allogeneic hematopoietic stem cell transplantation. Front Immunol 7:307
Gladstone DE, Zachary AA, Fuchs EJ et al (2013) Partially mismatched transplantation and human leukocyte antigen donor-specific antibodies. Biol Blood Marrow Transplant 19(4):647–652
Chang YJ, Zhao XY, Xu LP et al (2015) Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: a prospective study with randomly assigned training and validation sets. J Hematol Oncol 8:84
Süsal C, Opelz G (2002) Kidney graft failure and presentation against HLA class I and class II antigens. Transplantation 73(8):1269–1273
Minami M, Matsushima T, Mori Y et al (2019) Successful rescue transplantation with desensitization procedure after primary graft failure due to donor-specific antibody. Bone Marrow Transplant 54(8):1374–1376
Bramanti S, Nocco A, Mauro E et al (2016) Desensitization with plasma exchange in a patient with human leukocyte antigen donor-specific antibodies before T-cell-replete haploidentical transplantation. Transfusion 56(5):1096–1100
Misra MK, Xin JJ, Brown NK et al (2019) Effective desensitization for a strong donor-specific HLA antibody in a case of HLA-mismatched allogeneic hematopoietic cell transplantation. HLA 94(3):307–311
Fasano RM, Mamcarz E, Adams S et al (2014) Persistence of recipient human leucocyte antigen (HLA) antibodies and production of donor HLA antibodies following reduced intensity allogeneic haematopoietic stem cell transplantation. Br J Haematol 166(3):425–434
La Rocca U, Perrone MP, Piciocchi A et al (2019) Anti-HLA donor-specific antibodies in allogeneic stem cell transplantation: management and desensitization protocol. Bone Marrow Transplant 54(10):1717–1720
Wang HX, Wang ZD, Zheng XL et al (2013) Hematopoietic stem cell transplantation with umbilical cord multipotent stromal cell infusion for the treatment of aplastic anemia–a single-center experience. Cytotherapy 15(9):1118–1125
Ball LM, Egeler Rm (2008) Acute GvHD: pathogenesis and classification. Bone Marrow Transplant 41(Suppl 2):S58-64
Dignan FL, Amrolia P, Clark A et al (2012) Diagnosis and management of chronic graft-versus-host disease. Br J Haematol 158(1):46–61
Ciurea SO, Cao K, Fernadez-Vina M et al (2018) The European Society for Blood and Marrow Transplantation (EBMT) Consensus Guidelines for the detection and treatment of donor-specific anti-HLA antibodies (DSA) in haploidentical hematopoietic cell transplantation. Bone Marrow Transplant 53(5):521–534
Zachary AA, Leffell MS (2014) Desensitization for solid organ and hematopoietic stem cell transplantation. Immunol Rev 258(1):183–207
Leffell MS, Jones RJ, Gladstone DE (2015) Donor HLA-specific Abs: to BMT or not to BMT? Bone Marrow Transplant 50(6):751–758
Zhang RL, He Y, Yang DL et al (2020) Combination treatment of rituximab and donor platelets infusion to reduce donor-specific anti-HLA anstibodies for stem cells engraftment in haploidentical transplantation. J Clin Lab Anal 34(7):e23261
Chang YJ, Xu LP, Wang Y et al (2020) Rituximab for desensitization during HLA-mismatched stem cell transplantation in patients with a positive donor-specific anti-HLA antibody. Bone Marrow Transplant 55(7):1326–1336
Bernardo ME, Fibbe WE (2015) Mesenchymal stromal cells and hematopoietic stem cell transplantation. Immunol Lett 168(2):215–221
Choe H, Gergis U, Hsu J et al (2019) Bortezomib and immune globulin have limited effects on donor-specific HLA antibodies in haploidentical cord blood stem cell transplantation: detrimental effect of persistent haploidentical donor-specific HLA antibodies. Biol Blood Marrow Transplant 25(2):e60–e64
Yoshihara S, Maruya E, Taniguchi K et al (2012) Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical HCT. Bone Marrow Transplant 47(4):508–515
Pan ZJ, Yuan XN, Li Y et al (2016) Dynamic detection of anti-human leukocyte antigen (HLA) antibodies but not HLA-DP loci mismatches can predict acute graft-versus-host disease and overall survival in HLA 12/12-matched unrelated donor allogeneic hematopoietic stem cell transplantation for hematological malignancies. Biol Blood Marrow Transplant 22(1):86–95
Delbos F, Barhoumi W, Cabanne L et al (2016) Donor immunization against human leukocyte class II antigens is a risk factor for graft-versus-host disease. Biol Blood Marrow Transplant 22(2):292–329
Acknowledgements
The authors are grateful for Yingjun Chang for his assistance in the design of desensitization protocol and editing this manuscript.
Funding
This work was supported by the Capital Health Development Foundation of China (2014–2-5122).
Author information
Authors and Affiliations
Contributions
WHX designed the research. ZXL and YHM performed the experiments and collected and analyzed the data. HDM, DL, ZL, LJ, XM, and LS provided technical and clinical expertise. ZXL and YHM wrote the manuscript. WHX edited the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zheng, X., Yan, H., Han, D. et al. Successful desensitization of high level donor-specific anti-HLA antibody in patients with hematological diseases receiving haploidentical allografts. Ann Hematol 101, 1777–1783 (2022). https://doi.org/10.1007/s00277-022-04844-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04844-5