Abstract
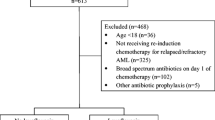
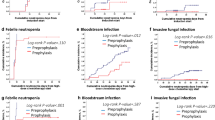
Acute myeloid leukemia (AML) patients undergoing consolidation chemotherapy with intermediate or high-dose cytarabine (IDAC/HiDAC) are often placed on prophylactic antibacterials. This practice is largely based on the benefits of prophylaxis (PPX) during induction chemotherapy. However, recent concerns regarding antibacterial prophylaxis have emerged including risk of Clostridioides difficile colitis, medication toxicities, and the potential for fostering multidrug-resistant pathogens. We therefore retrospectively explored whether antibacterial PPX is beneficial during cytarabine consolidation. Adult AML patients who received IDAC/HiDAC at our institution from January 2007 to March 2018 were evaluated for receipt of antibacterial PPX. The primary endpoint was rate of febrile neutropenia (FN); secondary endpoints were rates of unplanned hospitalization, bacteremia, infection from resistant organisms, C. difficile colitis, and death from infection. One hundred twenty patients with data from 229 IDAC/HiDAC cycles were included. Patients who received antibacterial PPX were more often hospitalized during cytarabine cycle 1 (C1) than those who received no PPX. Patients who received PPX had significantly more episodes of bacteremia, in addition to infections from resistant, predominantly Gram-positive organisms during cycle 1 of consolidation than those without PPX. Antibacterial PPX during IDAC/HiDAC consolidation treatment at our institution did not decrease the rates of FN, hospitalization, or bacteremia and was associated with higher risk of infection from drug-resistant bacteria in C1. Prospective studies examining antibacterial prophylaxis during cytarabine consolidation for AML patients are necessary, with strong consideration made for institution-specific protocols.

Similar content being viewed by others
References
De Kouchkovsky I, Abdul-Hay M (2016) Acute myeloid leukemia: a comprehensive review and 2016 update. Blood Cancer J 6:e441
Shallis RM, Wang R, Davidoff A, Ma X, Zeidan AM (2019) Epidemiology of acute myeloid leukemia: recent progress and enduring challenges. Blood Rev 36:70–87
Dohner H, Estey E, Grimwade D et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
Iqbal M, Phan M, Machiorlatti M (2016) Impact of duration of neutropenia and lymphopenia on AML patients undergoing induction chemotherapy. Blood 128:5178
Buckley SA, Othus M, Vainstein V, Abkowitz JL, Estey EH, Walter RB (2014) Prediction of adverse events during intensive induction chemotherapy for acute myeloid leukemia or high-GRADE myelodysplastic syndromes. Am J Hematol 89:423–428
Gafter-Gvili A, Fraser A, Paul M et al (2005) Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy. Cochrane Database Syst Rev (4):CD004386
Gafter-Gvili A, Fraser A, Paul M et al (2012) Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy. Cochrane Database Syst Rev 1:CD004386
Mikulska M, Averbuch D, Tissot F et al (2018) Fluoroquinolone prophylaxis in haematological cancer patients with neutropenia: ECIL critical appraisal of previous guidelines. J Inf Secur 76:20–37
Leibovici L, Paul M, Cullen M, Bucaneve G, Gafter-Gvili A, Fraser A, Kern WV (2006) Antibiotic prophylaxis in neutropenic patients: new evidence, practical decisions. Cancer 107:1743–1751
Bainschab A, Quehenberger F, Greinix HT, Krause R, Wölfler A, Sill H, Zebisch A (2016) Infections in patients with acute myeloid leukemia treated with low-intensity therapeutic regimens: risk factors and efficacy of antibiotic prophylaxis. Leuk Res 42:47–51
Lee SSF, Fulford AE, Quinn MA, Seabrook J, Rajakumar I (2018) Levofloxacin for febrile neutropenia prophylaxis in acute myeloid leukemia patients associated with reduction in hospital admissions. Support Care Cancer 26:1499–1504
Chung SJ, Miller RA, Permpalung N, Baker AW, Diehl LF, Rizzieri DA, Alexander BD (2019) Fluoroquinolone prophylaxis reduces febrile neutropenia, bloodstream infections from mucosal translocations, and intensive care admissions in high risk hematological patients, a single center experience. Leuk Lymphoma 60:488–492
Wolf J, Tang L, Flynn PM, Pui CH, Gaur AH, Sun Y, Inaba H, Stewart T, Hayden RT, Hakim H, Jeha S (2017) Levofloxacin prophylaxis during induction therapy for pediatric acute lymphoblastic leukemia. Clin Infect Dis 65:1790–1798
Owattanapanich W, Chayakulkeeree M (2019) Efficacy of levofloxacin as an antibacterial prophylaxis for acute leukemia patients receiving intensive chemotherapy: a systematic review and meta-analysis. Hematology 24:362–368
Bucaneve G, Micozzi A, Menichetti R et al (2005) Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. N Engl J Med 353:988–998
Rangaraj G, Granwehr BP, Jiang Y, Hachem R, Raad I (2010) Perils of quinolone exposure in cancer patients: breakthrough bacteremia with multidrug-resistant organisms. Cancer 116:967–973
Sousa J, Alves G, Fortuna A, Falcao A (2014) Third and fourth generation fluoroquinolone antibacterials: a systematic review of safety and toxicity profiles. Curr Drug Saf 9:89–105
Spellberg B, Doi Y (2015) The rise of fluoroquinolone-resistant Escherichia coli in the community: scarier than we thought. J Infect Dis 212:1853–1855
Przybylski DJ, Reeves DJ (2018) Impact of fluoroquinolone prophylaxis on documented infections in patients with febrile neutropenia. Infect Dis (Lond) 50:395–398
Mihu CN, Rhomberg PR, Jones RN, Coyle E, Prince RA, Rolston KV (2010) Escherichia coli resistance to quinolones at a comprehensive cancer center. Diagn Microbiol Infect Dis 67:266–269
Rapoport B, Klastersky J, Raftopoulos H et al (2016) The emerging problem of bacterial resistance in cancer patients; proceedings of a workshop held by MASCC “Neutropenia, Infection and Myelosuppression” Study Group during the MASCC annual meeting held in Berlin on 27-29 June 2013. Support Care Cancer 24:2819–2826
Kawasaki Y, Kimura SI, Nakano H, Mashima K, Shirato Y, Kawaguchi SI, Toda Y, Ochi SI, Nagayama T, Minakata D, Yamasaki R, Morita K, Ashizawa M, Yamamoto C, Hatano K, Sato K, Oh I, Fujiwara SI, Ohmine K, Kako S, Muroi K, Kanda Y (2019) Comparison of neutropenia profiles in different treatment protocols for acute myeloid leukemia using the D-index. Int J Hematol 109:470–476
Krauth MT, Florian S, Bohm A et al (2006) Immunological characterization and antibacterial function of persisting granulocytes in leukemic patients receiving pulse cytosine arabinoside-consolidation chemotherapy on days 1, 3, and 5. J Immunol 176:1759–1768
Kusick K, Gallagher EM, Yeh JY (2011) Fluoroquinolone prophylaxis in acute myeloid leukemia (AML) patients undergoing post-remission chemotherapy reduces hospital admission rates. Blood 118:2570
Saini L, Rostein C, Atenafu EG, Brandwein JM (2013) Ambulatory consolidation chemotherapy for acute myeloid leukemia with antibacterial prophylaxis is associated with frequent bacteremia and the emergence of fluoroquinolone resistant E. coli. BMC Infect Dis 13:284
Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, Langston AA, Nastoupil LJ, Rajotte M, Rolston KV, Strasfeld L, Flowers CR (2018) Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J Clin Oncol 36:3043–3054
Maertens JA, Girmenia C, Bruggemann RJ et al (2018) European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European Conference on Infections in Leukaemia. J Antimicrob Chemother 73:3221–3230
Baden LR, Swaminathan S, Angarone M, Blouin G, Camins BC, Casper C, Cooper B, Dubberke ER, Engemann AM, Freifeld AG, Greene JN, Ito JI, Kaul DR, Lustberg ME, Montoya JG, Rolston K, Satyanarayana G, Segal B, Seo SK, Shoham S, Taplitz R, Topal J, Wilson JW, Hoffmann KG, Smith C (2016) Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 14:882–913
Cullen M, Steven N, Billingham L, Gaunt C, Hastings M, Simmonds P, Stuart N, Rea D, Bower M, Fernando I, Huddart R, Gollins S, Stanley A, Simple Investigation in Neutropenic Individuals of the Frequency of Infection after Chemotherapy +/- Antibiotic in a Number of Tumours (SIGNIFICANT) Trial Group (2005) Antibacterial prophylaxis after chemotherapy for solid tumors and lymphomas. N Engl J Med 353:988–998
Gudiol C, Bodro M, Simonetti A, Tubau F, González-Barca E, Cisnal M, Domingo-Domenech E, Jiménez L, Carratalà J (2013) Changing aetiology, clinical features, antimicrobial resistance, and outcomes of bloodstream infection in neutropenic cancer patients. Clin Microbiol Infect 19:474–479
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR, Infectious Diseases Society of America (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 52:e56–e93
Buffie CG, Bucci V, Stein RR, McKenney PT, Ling L, Gobourne A, No D, Liu H, Kinnebrew M, Viale A, Littmann E, van den Brink MRM, Jenq RR, Taur Y, Sander C, Cross JR, Toussaint NC, Xavier JB, Pamer EG (2015) Precision microbiome reconstitution restores bile acid mediated resistance to Clostridium difficile. Nature 517:205–208
Ziegler M, Han JH, Landsburg D et al (2019) Impact of Levofloxacin for the prophylaxis of bloodstream infection on the gut microbiome in patients with hematologic malignancy. Open Forum Infect Dis 6:ofz252
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, Srinivasan A, Dellit TH, Falck-Ytter YT, Fishman NO, Hamilton CW, Jenkins TC, Lipsett PA, Malani PN, May LS, Moran GJ, Neuhauser MM, Newland JG, Ohl CA, Samore MH, Seo SK, Trivedi KK (2016) Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 62:e51–e77
Funding
DF has received research support from Astellas and Viracor-Eurofins, and consultant fee from Viracor-Eurofins.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
A waiver for informed consent was granted by our institutional review board since this was a retrospective study where a number of the patients involved were deceased.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vale, C.A., Egan, P.C., Ingham, R. et al. Antibiotic use during cytarabine consolidation in acute myeloid leukemia. Ann Hematol 100, 79–84 (2021). https://doi.org/10.1007/s00277-020-04238-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04238-5