Abstract
Purpose
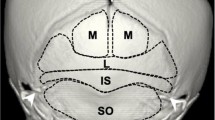
This investigation aimed to study the types of external occipital protuberance (EOP) with special reference to Type 3 (spine type). Detailed information will be useful for clinicians to manage occipital headaches or issues related to the biomechanics of the neck and for accurate radiological interpretations.
Methods
Thirty-one dry intact cadaveric skulls were studied for EOP classification. In Type III EOP cases, the size of EOP was noticed using different modalities and compared. The superior nuchal lines and external occipital crest were observed for their prominence and any variation.
Results
42% of the skulls belong to Type 1, 51.5% to Type 2, and 6.5% to Type 3 EOP. Superior nuchal lines and external occipital crest were more prominent in Types 2 and 3 EOP. In Type 3 EOP cases, the mean length, width, and thickness of the spine as measured directly on the skull were 16.63 mm; 20.1 mm, and 7.82 mm respectively, the same as radiograph findings. CT examination revealed the average volume as 0.95 cm3. Out of two Type 3 EOP cases, the spine with larger values for its size was having a lesser volume value in CT.
Conclusions
Plain lateral radiography is a reliable method to measure the length and thickness of spinous EOP. However, more values of these parameters for morphometry of the EOP spine do not mean more volume of EOP and vice versa. Detailed information regarding the occurrence of occipital spur and its morphology will be of great importance to neurosurgeons, sports, physicians, emergency departments, and radiologists.



Similar content being viewed by others
Availability of data and materials
The data are available on request, from the corresponding author.
References
Bogduk N (1981) The anatomy of occipital neuralgia. Clin Exp Neurol 17:167–184
Gómez Zubiaur A, Alfageme F, López-Negrete E, Roustan G (2019) Type 3 external occipital protuberance (spine type): ultrasonographic diagnosis of an uncommon cause of subcutaneous scalp pseudotumor in adolescents. Actas Dermosifiliogr. https://doi.org/10.1016/j.ad.2018.04.015
Gülekon IN, Turgut HB (2003) The external occipital protuberance: can it be used as a criterion in the determination of sex? J Forensic Sci 48:513–516
Iwanaga J, Singh V, Ohtsuka A, Hwang Y, Kim HJ, Moryś J et al (2021) Acknowledging the use of human cadaveric tissues in research papers: recommendations from anatomical journal editors. Clin Anat 34:2–4
Jacques T, Jaouen A, Kuchcinski G et al (2020) Enlarged external occipital protuberance in young French individuals’ head CT: stability in prevalence, size, and type between 2011 and 2019. Sci Rep 10:6518. https://doi.org/10.1038/s41598-020-63554-y
Kadri PAS, Al-Mefty O (2007) Anatomy of the nuchal ligament and its surgical applications. Neurosurgery 61:301–304
Marshall RC, Abela C, Eccles S (2015) Painful exostosis of the external occipital protuberance. J Plast Reconstr Aesthet Surg 68(11):e174–e176. https://doi.org/10.1038/s41598-018-21625-1
Nevo O, Bronshtein M (2010) Fetal transient occipital bone protuberance during early pregnancy. Prenat Diagn 30:879–881. https://doi.org/10.1002/pd.2580
Sattur M, Korson C, Henderson F Jr, Kalhorn S (2019) Presentation and management of traumatic occipital spur fracture. Am J Emerg Med 37:1005.e1-1005.e2. https://doi.org/10.1016/j.ajem.2019.01.043
Satyarthee GD (2019) External occipital protuberance projecting as downward curved horn presenting with intractable occipital pain: report of a first case. J Pediatr Neurosci 14:173–174. https://doi.org/10.4103/jpn.JPN_94_18
Shahar D, Sayers MGL (2016) A morphological adaptation? The prevalence of enlarged external occipital protuberance in young adults. J Anat 229:286–291
Shahar D, Sayers MGL (2018) Prominent exostosis projecting from the occipital squama more substantial and prevalent in young adults than older age groups. Sci Rep 8:3354
Shahar D, Evans J, Sayers MGL (2018) Large enthesophytes in teenage skulls: mechanical, inflammatory and genetic considerations. Clin Biomech (Bristol, Avon) 53:60–64
Singh R (2012) Bony tubercle at external occipital protuberance and prominent ridges. J Craniofac Surg 23:1873–1874
Srivastava M, Asghar A, Srivastava NN, Gupta N, Jain A, Verma J (2018) An anatomic morphological study of occipital spurs in human skulls. J Craniofac Surg 29:217–219. https://doi.org/10.1097/SCS.0000000000004205
Standring S (2007) Gray’s anatomy, 14th edn. Churchill Livingstone Elsevier, London, p 411
Sundar R, Yuvaraj Babu K (2020) Morphometric analysis of external occipital crest. Biosc Biotech Res Comm. https://doi.org/10.21786/bbrc/13.8/101
Tubbs RS, Mortazavi MM, Loukas M, D’Antoni AV, Shoja MM, Chern JJ et al (2011) Anatomical study of the third occipital nerve and its potential role in occipital headache/neck pain following midline dissections of the craniocervical junction. J Neurosurg Spine 15:71–75
Varghese E, Samson RS, Kumbargere SN, Pothen M (2017) Occipital spur: understanding a normal yet symptomatic variant from orthodontic diagnostic lateral cephalogram. BMJ Case Rep. https://doi.org/10.1136/bcr-2017220506
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research and teaching could be performed. Results from such research can potentially increase scientific knowledge and can improve patient care. Therefore, these donors and their families deserve our highest respect [4].
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
AS: Project development, Data collection, Data analysis and management, manuscript writing, approval of the final version. PC: Data management, Data analysis, approval of the final version. PS: Project development, Data analysis, manuscript editing, approval of the final version.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no competing interests.
Ethical approval
The study is approved by Institutional Ethical Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singal, A., Chaudhary, P. & Singh, P. External occipital protuberance classification with special reference to spine type and its clinical implications. Surg Radiol Anat 45, 555–561 (2023). https://doi.org/10.1007/s00276-023-03133-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03133-8