Abstract
Purpose
The purpose of this study is to provide a morphometric description of the bony margins of the interlaminar spaces by level in the cervical spine for guidance of safe posterior cervical surgical dissection and decompression. We also aim to describe the impact of increasing static cervical lordosis on the overlap between the lamina.
Methods
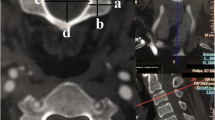
Morphometric measurements of the interlaminar space were performed on 100 consecutive cervical spine CT scans of patients ranging in age from 18 to 50 years were selected. Three raters performed measurements of the interlaminar height measured using two techniques (true interlaminar height and surgical interlaminar height), and interlaminar width from C2–C3 to C7–T1.
Results
In total, 100 patients were included. The true interlaminar height was greatest at C2–3, C3–4, C4–5 (5.2 ± 1.4–1.8 mm) and smallest at C6–7 (4.4 ± 1.3 mm). Surgical interlaminar height was greatest at C3–4 (4.2 ± 1.7) and smallest at C6–7 (3.0 ± 1.3 mm). The widest interlaminar space was observed at C3–4 (27.1 ± 2.1 mm) and most narrow at C7–T1 (20.9 ± 2.4 mm). Following multivariate regression, male gender was associated with greater interlaminar widths at each cervical level between C4 and T1 (Table 2). While greater patient height was associated with larger interlaminar height (true and surgical) and width at C2–3 and C4–5, weight was not independently associated with the interlaminar measurements. Increasing C2–C7 lordosis was significantly associated with decreasing true and surgical interlaminar heights at all levels except C7–T1, but was not associated with differences between interlaminar width.
Conclusion
The study provides a morphometric analysis of interlaminar anatomy in the cervical spine. Surgeons can apply this information in their pre-operative plan to safely approach the posterior cervical spine.



Similar content being viewed by others
References
Akhgar J, Terai H, Rahmani MS et al (2017) Anatomical analysis of the relation between human ligamentum flavum and posterior spinal bony prominence. J Orthop Sci 22:260–265
Baba S, Ikuta K, Ikeuchi H, Shiraki M, Komiya N, Kitamura T, Senba H, Shidahara S (2016) Risk factor analysis for C5 palsy after double-door laminoplasty for cervical spondylotic myelopathy. Asian Spine J 10:298–308
Bazaldúa CJJ, González LA, Gómez SA, Villarreal SE, Velázquez GSE, Sánchez UA, Elizondo-Omaña RE, Guznán LS (2011) Morphometric study of cervical vertebrae C3–C7 in a population from northeastern Mexico. Int J Morphol 29:325–330
Blizzard DJ, Gallizzi MA, Sheets C, Klement MR, Kleeman LT, Caputo AM, Eure M, Brown CR (2015) The role of iatrogenic foraminal stenosis from lordotic correction in the development of C5 palsy after posterior laminectomy and fusion. J Orthop Surg Res 10:160
Chen MN, Kang JD (2009) Cerebrospinal fluid leaks in anterior and posterior cervical spine surgery. Semin Spine Surg 21:161–166
Choi K-C, Ahn Y, Kang B-U, Ahn S-T, Lee S-H (2013) Motor palsy after posterior cervical foraminotomy: anatomical consideration. World Neurosurg 79:405.e1–4
El Aziz GSA, Zaki SM, El-Fark MMO, Mustafa HN, Al-Shali RA, Hamdy RM, Bangash M (2019) Morphohistometric study of the ligamentum flavum in cervical, thoracic and lumbar vertebrae: comparative approach. Eur j anat 23:315–323
Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, Okawa A, Takahashi K, Konishi H (2008) A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament. Spine 33:E990–E993
Huang MC, McGrail KM (2006) Incidental durotomy in cervical spinal surgery. Semin Spine Surg 18:230–234
Jack A, Ramey WL, Dettori JR, Tymchak ZA, Oskouian RJ, Hart RA, Chapman JR, Riew D (2019) Factors associated with C5 palsy following cervical spine surgery: a systematic review. Global Spine J 9:881–894
Kim S, Lee S-H, Kim E-S, Eoh W (2014) Clinical and radiographic analysis of C5 palsy after anterior cervical decompression and fusion for cervical degenerative disease. J Spinal Disord Tech 27:436–441
Koo TK, Li MY (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropract Med 15:155–163
Lee H-J, Ahn J-S, Shin B, Lee H (2017) C4/5 foraminal stenosis predicts C5 palsy after expansive open-door laminoplasty. Eur Spine J 26:2340–2347
Lee TH, Kim SJ, Chung IH (2012) Morphometrical study of uncinate processes and vertebral body of cervical spine. J Korean Neurosurg Soc 51:247–252
Lubelski D, Derakhshan A, Nowacki AS, Wang JC, Steinmetz MP, Benzel EC, Mroz TE (2014) Predicting C5 palsy via the use of preoperative anatomic measurements. Spine J 14:1895–1901
Miyazaki M, Takita C, Yoshiiwa T, Itonaga I, Tsumura H (2010) Morphological analysis of the cervical pedicles, lateral masses, and laminae in developmental canal stenosis. Spine 35:E1381–E1385
Prabavathy G, Philip XC, Arthi G, Sadeesh T (2017) Morphometric study of cervical vertebrae C3–C7 in South Indian population—a clinico-anatomical approach. Ital J Anat Embryol 122:49–57
Rahmani MS, Terai H, Akhgar J et al (2017) Anatomical analysis of human ligamentum flavum in the cervical spine: special consideration to the attachments, coverage, and lateral extent. J Orthop Sci 22:994–1000
Raveendranath V, Kavitha T, Umamageswari A (2019) Morphometry of the uncinate process, vertebral body, and lamina of the C3–7 vertebrae relevant to cervical spine surgery. Neurospine 16:748–755
Srivastava A, Nanda G, Mahajan R, Nanda A, Batra S, Mishra N, Pandita N, Chhabra HS (2019) Feasibility of sub-axial cervical laminar screws, including C7, in the Indian population: a study on 50 patients using computed tomography-based morphometry measurements. Asian Spine J 13:7–12
Wu FL, Sun Y, Pan SF, Zhang L, Liu ZJ (2014) Risk factors associated with upper extremity palsy after expansive open-door laminoplasty for cervical myelopathy. Spine J 14:909–915
Xu R, Burgar A, Ebraheim NA, Yeasting RA (1999) The quantitative anatomy of the laminas of the spine. Spine 24:107–113
Funding
No funding was devoted to this study.
Author information
Authors and Affiliations
Contributions
PKL: project development, data collection, and manuscript writing. AAP: data collection, data analysis, and manuscript writing. MES: data collection and manuscript writing. JW: data collection and manuscript writing. TJA: project development and manuscript writing. HJK: project development and manuscript writing. VL: project development and manuscript writing. SI: project development and manuscript writing. SAQ: project development and manuscript writing. YK: project development, manuscript writing, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Louie, P.K., Perez, A.A., Steinhaus, M.E. et al. Morphometric analysis of cervical interlaminar space for posterior surgical approach and decompression. Surg Radiol Anat 43, 873–879 (2021). https://doi.org/10.1007/s00276-020-02612-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-020-02612-6