Abstract
Purpose
To investigate the predictability of local tumor progression (LTP) after microwave ablation (MWA) in colorectal carcinoma liver metastases (CRLM) patients by magnetic resonance imaging (MRI) radiomics and clinical characteristics-based combined model.
Materials and Methods
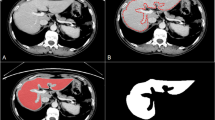
Forty-two consecutive CRLM patients (67 tumors) with post-MWA complete response at 1st month MRI were included in this retrospective study. One hundred and eleven radiomics features were extracted for each tumor and for each phase by manual segmentation from pre-treatment MRI T2 fat-suppressed (Phase 2) and early arterial phase T1 fat-suppressed sequences (Phase 1). A clinical model was constructed using clinical data, two combined models were created with feature reduction and machine learning by combining clinical data and Phase 2 and Phase 1 radiomics features. The predicting performance for LTP development was investigated.
Results
LTP developed in 7 patients (16.6%) and 11 tumors (16.4%). In the clinical model, the presence of extrahepatic metastases before MWA was associated with a high probability of LTP (p < 0.001). The pre-treatment levels of carbohydrate antigen 19–9 and carcinoembryonic antigen were higher in the LTP group (p = 0.010, p = 0.020, respectively). Patients with LTP had statistically significantly higher radiomics scores in both phases (p < 0.001 for Phase 2 and p = 0.001 for Phase 1). The classification performance of the combined model 2, created by using clinical data and Phase 2-based radiomics features, achieved the highest discriminative performance in predicting LTP (p = 0,014; the area under curve (AUC) value 0.981 (95% CI 0.948–0.990). The combined model 1, created using clinical data and Phase 1-based radiomics features (AUC value 0,927 (95% CI 0.860–0.993, p < 0.001)) and the clinical model alone [AUC value of 0.887 (95% CI 0.807–0.967, p < 0.001)] had similar performance.
Conclusion
Combined models based on clinical data and radiomics features obtained from T2 fat-suppressed and early arterial-phase T1 fat-suppressed MRI are valuable markers in predicting LTP after MWA in CRLM patients. Large-scale studies with internal and external validations are needed to come to a firm conclusion on the predictability of radiomics models in CRLM patients.






Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. https://doi.org/10.3322/caac.21708.
Valderrama-Treviño AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Javé EE. Hepatic metastasis from colorectal cancer. Euroasian J Hepatogastroenterol. 2017;7(2):166–75. https://doi.org/10.5005/jp-journals-10018-1241.
McNally SJ, Parks RW. Surgery for colorectal liver metastases. Dig Surg. 2013;30(4–6):337–47. https://doi.org/10.1159/000351442.
Akgül Ö, Çetinkaya E, Ersöz Ş, Tez M. Role of surgery in colorectal cancer liver metastases. World J Gastroenterol. 2014;20(20):6113–22. https://doi.org/10.3748/wjg.v20.i20.6113.
Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J. Colorectal cancer liver metastases—a population-based study on incidence, management and survival. BMC Cancer. 2018;18(1):78. https://doi.org/10.1186/s12885-017-3925-x.
Cummings LC, Payes JD, Cooper GS. Survival after hepatic resection in metastatic colorectal cancer: a population-based study. Cancer. 2007;109(4):718–26. https://doi.org/10.1002/cncr.22448.
Petre EN, Sofocleous C. Thermal ablation in the management of colorectal cancer patients with oligometastatic liver disease. Visc Med. 2017;33(1):62–8. https://doi.org/10.1159/000454697.
Takahashi H, Berber E. Role of thermal ablation in the management of colorectal liver metastasis. Hepatobiliary Surg Nutr. 2020;9(1):49–58. https://doi.org/10.21037/hbsn.2019.06.08.
Puijk RS, Dijkstra M, van den Bemd BAT, Ruarus AH, Nieuwenhuizen S, Geboers B, et al. Improved outcomes of thermal ablation for colorectal liver metastases: a 10-year analysis from the prospective amsterdam CORE registry (AmCORE). Cardiovasc Intervent Radiol. 2022;45(8):1074–89. https://doi.org/10.1007/s00270-022-03152-9.
Meijerink MR, Puijk RS, van Tilborg AAJM, Henningsen KH, Fernandez LG, Neyt M, et al. Radiofrequency and microwave ablation compared to systemic chemotherapy and to partial hepatectomy in the treatment of colorectal liver metastases: a systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2018;41(8):1189–204. https://doi.org/10.1007/s00270-018-1959-3.
Ruers T, Van Coevorden F, Punt CJ, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017. https://doi.org/10.1093/jnci/djx015.
Puijk RS, Ruarus AH, Vroomen LGPH, van Tilborg AAJM, Scheffer HJ, Nielsen K, et al. COLLISION Trial Group .Colorectal liver metastases: surgery versus thermal ablation (COLLISION)—a phase III single-blind prospective randomized controlled trial. BMC Cancer. 2018;18(1):821. https://doi.org/10.1186/s12885-018-4716-8.
Meijerink MR, Puijk RS, van den Tol PMP. COLLISION trial seeks to answer time-honored question: “thermal ablation or surgery for colorectal liver metastases?” Cardiovasc Intervent Radiol. 2019;42(8):1059–61. https://doi.org/10.1007/s00270-019-02236-3.
De Cobelli F, Della CA. Thermal ablation for colorectal liver metastases: the time has come. Cardiovasc Intervent Radiol. 2022;45:1090–1. https://doi.org/10.1007/s00270-022-03198-9.
van Amerongen MJ, Jenniskens SFM, van den Boezem PB, Fütterer JJ, de Wilt JHW. Radiofrequency ablation compared to surgical resection for curative treatment of patients with colorectal liver metastases—a meta-analysis. HPB (Oxford). 2017;19(9):749–56. https://doi.org/10.1016/j.hpb.2017.05.011.
Wang LJ, Zhang ZY, Yan XL, Yang W, Yan K, Xing BC. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: a propensity score analysis. World J Surg Oncol. 2018;16(1):207. https://doi.org/10.1186/s12957-018-1494-3.
Takahashi H, Kahramangil B, Berber E. Local recurrence after microwave thermosphere ablation of malignant liver tumors: results of a surgical series. Surgery. 2018;163(4):709–13.
Abreu de Carvalho LF, Logghe B, Van Cleven S, Vanlander A, Moura Ribeiro S, Geboes K, et al. Local control of hepatocellular carcinoma and colorectal liver metastases after surgical microwave ablation without concomitant hepatectomy. Langenbecks Arch Surg. 2021;406(8):2749–57. https://doi.org/10.1007/s00423-021-02219-4.
Puijk RS, Ahmed M, Adam A, Arai Y, Arellano R, de Baère T, et al. Consensus Guidelines for the definition of time-to-event end points in image-guided tumor ablation: results of the SIO and DATECAN initiative. Radiology. 2021;301(3):533–40. https://doi.org/10.1148/radiol.2021203715.
Rompianesi G, Pegoraro F, Ceresa CD, Montalti R, Troisi RI. Artificial intelligence in the diagnosis and management of colorectal cancer liver metastases. World J Gastroenterol. 2022;28(1):108–22. https://doi.org/10.3748/wjg.v28.i1.108.
Taghavi M, Staal F, Gomez Munoz F, Imani F, Meek DB, et al. CT-based radiomics analysis before thermal ablation to predict local tumor progression for colorectal liver metastases. Cardiovasc Intervent Radiol. 2021;44(6):913–20. https://doi.org/10.1007/s00270-020-02735-8.
Staal FCR, Taghavi M, van der Reijd DJ, Gomez FM, Imani F, Klompenhouwer EG, et al. Predicting local tumour progression after ablation for colorectal liver metastases: CT-based radiomics of the ablation zone. Eur J Radiol. 2021;141:109773. https://doi.org/10.1016/j.ejrad.2021.109773.
Nieuwenhuizen S, Puijk RS, van den Bemd B, Aldrighetti L, Arntz M, van den Boezem PB, et al. Resectability and ablatability criteria for the treatment of liver only colorectal metastases: multidisciplinary consensus document from the COLLISION Trial Group. Cancers (Basel). 2020;12(7):1779. https://doi.org/10.3390/cancers12071779.
Crocetti L, de Baére T, Pereira PL, Tarantino FP. CIRSE standards of practice on thermal ablation of liver tumours. Cardiovasc Intervent Radiol. 2020;43(7):951–62. https://doi.org/10.1007/s00270-020-02471-z.
Tibshirani R. Regression shrinkage and selection via the lasso. J R Statl Soc. 1996;58(1):267–88.
Unal I. Defining an optimal cut-point value in ROC analysis: an alternative approach. Comput Math Methods Med. 2017;2017:3762651. https://doi.org/10.1155/2017/3762651.
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. https://doi.org/10.1002/sim.2929.
Qin S, Liu GJ, Huang M, Huang J, Luo Y, Wen Y, et al. The local efficacy and influencing factors of ultrasound-guided percutaneous microwave ablation in colorectal liver metastases: a review of a 4-year experience at a single center. Int J Hyperthermia. 2019;36(1):36–43. https://doi.org/10.1080/02656736.2018.1528511.
Mimmo A, Pegoraro F, Rhaiem R, Montalti R, Donadieu A, Tashkandi A, et al. Microwave ablation for colorectal liver metastases: a systematic review and pooled oncological analyses. Cancers (Basel). 2022;14(5):1305. https://doi.org/10.3390/cancers14051305.
Knott EA, Ziemlewicz TJ, Lubner SJ, Swietlik JF, Weber SM, Zlevor AM, et al. Microwave ablation for colorectal cancer metastasis to the liver: a single-center retrospective analysis. J Gastrointest Oncol. 2021;12(4):1454–69. https://doi.org/10.21037/jgo-21-159.
Vogl TJ, Zitsch M, Albrecht M, D’Angelo T, Basten L, Gruber-Rouh T, et al. Long-term outcomes following percutaneous microwave ablation for colorectal cancer liver metastases. Int J Hyperthermia. 2022;39(1):788–95. https://doi.org/10.1080/02656736.2022.2077991.
Urbonas T, Anderson EM, Gordon-Weeks AN, Kabir SI, Soonawalla Z, Silva MA, et al. (2019) Factors predicting ablation site recurrence following percutaneous microwave ablation of colorectal hepatic metastases. HPB (Oxford).21(9): 1175–1184. doi: https://doi.org/10.1016/j.hpb.2019.01.007.
van Dam PJ, van der Stok EP, Teuwen LA, Van den Eynden GG, Illemann M, Frentzas S, et al. International consensus guidelines for scoring the histopathological growth patterns of liver metastasis. Br J Cancer. 2017;117(10):1427–41. https://doi.org/10.1038/bjc.2017.334.
Kong BT, Fan QS, Wang XM, Zhang Q, Zhang GL. Clinical implications and mechanism of histopathological growth pattern in colorectal cancer liver metastases. World J Gastroenterol. 2022;28(26):3101–15. https://doi.org/10.3748/wjg.v28.i26.3101.
Peng S, Huang P, Yu H, Wen Y, Luo Y, Wang X, et al. Prognostic value of carcinoembryonic antigen level in patients with colorectal cancer liver metastasis treated with percutaneous microwave ablation under ultrasound guidance. Medicine (Baltimore). 2018; 97(10): e0044. doi: https://doi.org/10.1097/MD.0000000000010044.
Cho JY, Lee YJ, Han HS, Yoon YS, Kim J, Choi Y, et al. Role of gadoxetic acid-enhanced magnetic resonance imaging in the preoperative evaluation of small hepatic lesions in patients with colorectal cancer. World J Surg. 2015;39(5):1161–6. https://doi.org/10.1007/s00268-015-2944-5.
Schulz A, Viktil E, Godt JC, Johansen CK, Dormagen JB, Holtedahl JE, et al. Diagnostic performance of CT, MRI and PET/CT in patients with suspected colorectal liver metastases: the superiority of MRI. Acta Radiol. 2016;57(9):1040–8. https://doi.org/10.1177/0284185115617349.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahveranova, A., Balli, H.T., Aikimbaev, K. et al. Prediction of Local Tumor Progression After Microwave Ablation in Colorectal Carcinoma Liver Metastases Patients by MRI Radiomics and Clinical Characteristics-Based Combined Model: Preliminary Results. Cardiovasc Intervent Radiol 46, 713–725 (2023). https://doi.org/10.1007/s00270-023-03454-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03454-6