Abstract
Purpose
Proximal splenic artery embolization (pSAE) has been advocated as a valuable tool to ameliorate portal hyper-perfusion (PHP). The purpose of this study was to determine the safety and efficacy of pSAE to treat refractory ascites (RA) and/or refractory hydrothorax (RH) in the setting of PHP post-liver transplant.
Material and Methods
A total of 30 patients who underwent pSAE for RA and/or RH after liver transplantation (LT) between January 2007 and December 2017 were analyzed retrospectively. The patients were divided into groups according to the time frame from pSAE to clinical resolution in order to identify predictors of RA/RH response to the procedure.
Results
Twenty-four (80%) patients responded to pSAE within three months, whereas 6 (20%) still required additional treatments for RA/RH at three months post-pSAE. In all cases clinical symptoms resolved within six months. Complications after pSAE were as follows: 2 cases of splenic infarction (6.6%), one case of post-splenic embolization syndrome (3.3%), one case of hepatic artery thrombosis (3.3%) and one case of portal vein (PV) thrombosis (3.3%). Increased intraoperative PV flow volume and increased pre-pSAE PV velocity, as well as higher estimated glomerular filtration rate were associated with early RA/RH resolution.
Conclusion
pSAE is safe and effective in treating RA and RH due to PHP after LT. This study suggests that clinical parameters indicating more severe PHP and better kidney function are possible predictors for early response to pSAE.






Similar content being viewed by others
Abbreviations
- eGFR:
-
Estimated glomerular filtration rate
- HABR:
-
Hepatic artery buffer response
- LT:
-
Liver transplantation
- MELD:
-
Model for end stage liver disease
- PHP:
-
Portal hyper-perfusion
- pSAE:
-
Proximal splenic artery embolization
- PV:
-
Portal vein
- RA:
-
Refractory ascites
- RH:
-
Refractory hydrothorax
- US:
-
Ultrasound
References
Ostojic A, Petrovic I, Silovski H, Kosuta I, Sremac M, Mrzljak A. Approach to persistent ascites after liver transplantation. World J Hepatol. 2022;14(9):1739–46.
Garbuzenko DV, Arefyev NO. Hepatic hydrothorax: an update and review of the literature. WJH. 2017;9(31):1197–204.
Nishida S, Gaynor JJ, Nakamura N, Butt F, Illanes HG, Kadono J, et al. Refractory ascites after liver transplantation: an analysis of 1058 liver transplant patients at a single center. Am J Transplant. 2006;6(1):140–9.
Siqueira F, Kelly T, Saab S. Refractory ascites: pathogenesis, clinical impact, and management. Gastroenterol Hepatol. 2009;5(9):647–56.
Quintini C, Hirose K, Hashimoto K, Diago T, Aucejo F, Eghtesad B, et al. “Splenic artery steal syndrome” is a misnomer: the cause is portal hyperperfusion, not arterial siphon. Liver Transpl. 2008;14(3):374–9.
Quintini C, D’Amico G, Brown C, Aucejo F, Hashimoto K, Kelly DM, et al. Splenic artery embolization for the treatment of refractory ascites after liver transplantation. Liver Transpl. 2011;17(6):668–73.
Kelly DM, Miller C. Understanding the splenic contribution to portal flow: the role of splenic artery ligation as inflow modification in living donor liver transplantation. Liver Transpl. 2006;12(8):1186–8.
Hiraki Y, Uchida K, Nishida S, Levi DM, Selvaggi G, Tekin A, et al. A case report of severe hepatic artery vasospasm induced by hepatic arterial buffer response after liver transplantation. Transpl Proc. 2016;48(9):3167–70.
Sanada Y, Mizuta K, Urahashi T, Ihara Y, Wakiya T, Okada N, et al. Hepatic arterial buffer response after pediatric living donor liver transplantation: report of a case. Transpl Proc. 2011;43(10):4019–24.
Spitzer AL, Dick AAS, Bakthavatsalam R, Halldorson JB, Salvalaggio PR, Reyes JD, et al. Intraoperative portal vein blood flow predicts allograft and patient survival following liver transplantation. HPB. 2010;12(3):166–73.
Anisa-Nutu O, Justo-Alonso I, Marcacuzco-Quinto AA, Calvo-Pulido J, Jiménez-Romero LC. Complete splenic embolization for the treatment of refractory ascites after liver transplantation. Rev Esp Enferm Dig. 2018;3:257–9.
Eipel C, Abshagen K, Vollmar B. Regulation of hepatic blood flow: The hepatic arterial buffer response revisited. World J Gastroenterol. 2010;16(48):6046–57.
Pinto S, Reddy SN, Horrow MM, Ortiz J. Splenic artery syndrome after orthotopic liver transplantation: a review. Int J Surg. 2014;12(11):1228–34.
Piano S, Tonon M, Angeli P. Management of ascites and hepatorenal syndrome. Hepatol Int. 2018;12(S1):122–34.
Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, et al. The management of ascites in cirrhosis: report on the consensus conference of the international ascites club. Hepatology. 2003;38(1):258–66.
Porcel JM. Management of refractory hepatic hydrothorax: current opinion in pulmonary medicine. Curr Opin Pulm Med. 2014;20(4):352–7.
Hadduck TA, McWilliams JP. Partial splenic artery embolization in cirrhotic patients. World J Radiol. 2014;6(5):160–8.
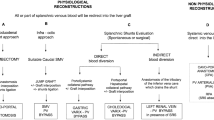
Pereira K, Salsamendi J, Fan J. An approach to diagnosis and endovascular treatment of refractory ascites in liver transplant: a pictorial essay and clinical practice algorithm. Exp Clin Transpl. 2015;13(5):387–93.
Cheng YF, Huang TL, Chen TY, Concejero A, Tsang LLC, Wang CC, et al. Liver graft-to-recipient spleen size ratio as a novel predictor of portal hyperperfusion syndrome in living donor liver transplantation. Am J Transpl. 2006;6(12):2994–9.
Presser N, Quintini C, Tom C, Wang W, Liu Q, Diago-Uso T, et al. Safety and efficacy of splenic artery embolization for portal hyperperfusion in liver transplant recipients: a 5-year experience: SAE for portal hyperperfusion. Liver Transpl. 2015;21(4):435–41.
Meighani A, Jafri SMR, Raoufi M, Salgia R. Splenic artery embolization for treatment of refractory ascites after liver transplantation: ACG case reports journal. ACG Case Rep J. 2016;3(2):136–8.
Pravisani R, Baccarani U, Adani G, Lorenzin D, Vit A, Cherchi V, et al. Splenic artery syndrome as a possible cause of late onset refractory ascites after liver transplantation: management with proximal splenic artery embolization. Transpl Proc. 2016;48(2):377–9.
Koconis KG, Singh H, Soares G. Partial splenic embolization in the treatment of patients with portal hypertension: a review of the English language literature. J Vasc Interv Radiol. 2007;18(4):463–81.
Ekeh AP, Kauffman S. Complications arising from splenic artery embolization: a review of an 11-year experience. Am J Surg. 2013;205(3):5.
Madoff DC, Denys A, Wallace MJ, Murthy R, Gupta S, Pillsbury EP, et al. Splenic arterial interventions: anatomy, indications, technical considerations, and potential complications. Radiographics. 2005;25(Suppl_1):S191-211.
Zhang L, Zhang ZG, Long X, Liu FL, Zhang WG. Severe complications after splenic artery embolization for portal hypertension due to hepatic cirrhosis. Risk Manag Healthc Policy. 2020;13:135–40.
Kim H, Suh KS, Jeon YM, Park MS, Choi Y, Mori S, et al. Partial splenic artery embolization for thrombocytopenia and uncontrolled massive ascites after liver transplantation. Transpl Proc. 2012;44(3):755–6.
Acknowledgements
None.
Funding
There were no external funding resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
D’Amico, G., Partovi, S., Del Prete, L. et al. Proximal Splenic Artery Embolization for Refractory Ascites and Hydrothorax Post-Liver Transplant. Cardiovasc Intervent Radiol 46, 470–479 (2023). https://doi.org/10.1007/s00270-023-03376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03376-3