Abstract
Purpose
This study aimed to assess 5-year effectiveness and safety of femoropopliteal angioplasty with the Luminor® 35 drug-coated balloon (DCB).
Materials and Methods
The EffPac trial was a prospective, multicenter, randomized controlled trial that enrolled 171 patients of Rutherford category 2 to 4 with medium length femoropopliteal lesions. Patients were allocated 1:1 to either Luminor® 35 DCB angioplasty or plain old balloon angioplasty (POBA). Assessment at 5 years included primary patency, freedom from clinically driven target lesion revascularization (CD-TLR), clinical improvement, and target limb amputation. Long-term vital status was ascertained in 97.1% of the participants.
Results
Kaplan–Meier curves at 5 years demonstrate a primary patency of 61.4% after DCB angioplasty and 53.5% after POBA (log-rank p = 0.040) with a decreasing difference throughout the observation period. Freedom from TLR was 82.1% and 73.7%, respectively (log-rank p = 0.050). Incidence of primary clinical improvement was similar between groups (61% DCB vs. 64% POBA, p = 0.94). Major target limb amputation was necessary in one POBA-group participant. Freedom from all-cause death at 5 years was 88.5% after DCB and 86.0% after POBA (log-rank p = 0.34).
Conclusions
Primary patency after femoropopliteal DCB angioplasty remained superior to POBA throughout 5 years, however, with decreasing difference. Clinical improvement, freedom from TLR, and all-cause mortality were similar between groups over the long term. (Effectiveness of Paclitaxel-Coated Luminor® Balloon Catheter Versus Uncoated Balloon Catheter in the Superficial Femoral Artery [EffPac]; NCT02540018).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug-coated balloon (DCB) angioplasty using the antiproliferative effect of paclitaxel has been shown to reduce late lumen loss (LLL) and prevent restenosis more successfully than plain old balloon angioplasty (POBA) [1, 2]. However, effect size differs considerably across DCB types [3] and 5-year results are provided for only a few. In addition, a safety signal indicated increased long-term all-cause mortality with paclitaxel-eluting devices [4] and gave rise to a fierce debate that remains unsolved to this day [5].
Until now, data from randomized controlled trials throughout 5 years are available from the THUNDER [6], the IN.PACT SFA [7], the AcoArt [8], and the LEVANT studies [9]. The THUNDER, IN.PACT SFA, and AcoART studies found superior freedom from clinically driven target lesion revascularization (CD-TLR) after DCB compared to plain old balloon angioplasty (POBA). However, in THUNDER, neither Kaplan–Meier estimates nor information on precision are provided on primary patency. At 5 years, the LEVANT studies did only report on mortality but not on effectiveness. None of the above-mentioned studies found significant differences in all-cause mortality between DCB and POBA throughout 5 years.
The aim of the present EffPac long-term evaluation was to assess effectiveness and safety of femoropopliteal angioplasty with the Luminor® 35 (iVascular, Barcelona, Spain) DCB. In the EffPac trial, vital status at 5 years was obtained from almost all participants.
Materials and Methods
Study Design and Population
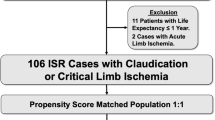
The EffPac trial was a prospective, multicenter, participant- and core laboratory-blinded, randomized controlled study to compare Luminor® 35 DCB angioplasty with POBA in patients with femoropopliteal artery disease of Rutherford category 2–4. The detailed study design and eligibility criteria were published previously [1, 10] (Supplementary Table 1). Patients of Rutherford category 2–4 and single femoropopliteal target lesions of ≤ 15 cm were enrolled at 11 German sites between September 2015 and December 2016. Participants were allocated 1:1 to either DCB or POBA. Follow-ups included clinical and ultrasonographic examination at 6, 12, 24, 42, and 60 months. In addition, upon request of the Federal Institute for Drugs and Medical Devices (BfArM, Bonn, Germany) that had been addressed to all ongoing studies on paclitaxel-coated devices in July 2019, we attempted to obtain the vital status of all participants by telephone within 5 years after the intervention (Fig. 1) [11]. Adverse events were reviewed by an independent data safety monitoring board and angiographic and ultrasonographic findings were adjudicated by blinded, independent core laboratory staff members (CoreLab Black Forest, Bad Krozingen, Germany). The study complied with the Declaration of Helsinki and Good Clinical Practice Guidelines. The Protocol was approved by the responsible ethic committees of all investigational sites and all participants provided written informed consent. The EffPac trial is registered with ClinicalTrials.gov: NCT02540018.
Participant flow in the EffPac trial through the 5-year follow-up. One hundred seventy-one patients were randomized 1:1 into groups that underwent Luminor 35 DCB angioplasty or plain old balloon angioplasty for the treatment of femoropopliteal lesions and were followed up through 60 months. Withdrawal was due to withdrawal of consent or to other reasons for loss to follow up DCB drug-coated balloon, DUS duplex ultrasonography, POBA plain old balloon angioplasty
Study Intervention
Detailed description of the study intervention was provided earlier [1, 10, 12]. Briefly, patients were randomized only after the lesion had been crossed endoluminally with a guidewire and successfully pre-dilated with a standard balloon for 60 ± 10 s in both study arms. Study device was the CE-marked Luminor® 35 DCB catheter (iVascular S.L.U., Barcelona, Spain). This DCB is coated with paclitaxel at a surface concentration of 3 µg/mm2 and an organic ester excipient. Control devices were CE-marked uncoated balloon catheters. In case of dissection, prolonged balloon inflation was required. Bailout stenting was permitted at the discretion of the investigator. Participants received acetylsalicylic acid and clopidogrel for at least 4 weeks after the intervention.
Study Outcome Measures
At 5 years, secondary long-term outcome measures included primary patency, freedom from CD-TLR, freedom from any target vessel revascularization (TVR), incidence of clinical and hemodynamic improvement, incidence of target limb amputation, and freedom from all-cause death. Primary patency was defined as absence of > 50% diameter restenosis of the target lesion by angiography or a peak systolic velocity ratio of < 2.4 by duplex ultrasonography without the need for TLR. Restenosis had to be adjudicated by the core laboratory. Any surgical or endovascular revascularization of the target lesion on grounds of symptoms was considered CD-TLR. Clinical improvement referred to improvement by at least one Rutherford category and hemodynamic improvement to an increase of the ankle-brachial index (ABI) by ≥ 0.15 or to 0.9. Primary improvement occurred if no TLR was needed, whereas secondary improvement also included participants who improved only after TLR. A post-hoc subgroup analysis on loss of primary patency on age, gender, diabetes/non-diabetes, smoker/non-smoker, lesion length, chronic total occlusion, calcification, dissection, and distal runoff vessels was conducted to assess interaction with the treatment effect.
Statistical Analysis
Categorical data are presented as counts and percentages and were compared with Fisher’s exact- or Chi-square test when unpaired and with Wilcoxon signed-rank test when paired. Continuous data are described as means with standard deviations and compared with Student t or Mann–Whitney U test. Kaplan–Meier analysis was applied to provide time point estimates of primary patency, freedom from CD-TLR, freedom from TVR, and freedom from all-cause death, and to compare groups using the log-rank test. Sixty-five months were set as cutoff for the analyses. The level of statistical significance was set at p < 0.05. Post-hoc subgroup analysis on loss of primary patency was conducted with Cox proportional regression analysis that was adjusted for centers. Due to multiple testing in the subgroup analysis, the significance level was lowered to 0.006. Data were analyzed with SAS 9.4 (SAS Institute, Cary, NC, USA) and XLSTAT (Version 2015.6.01.24026, Addinsoft, Paris, France).
Results
Study Population
We randomized 171 subjects to either DCB angioplasty (n = 85, of those 84 underwent DCB angioplasty) or POBA (n = 86). At 5 years, 55% of the DCB group participants and 53% of the POBA group participants completed the clinical follow-up, and 46% and 50% the DUS follow-up, respectively. Vital status was ascertained in 94% of DCB group-, and in 100% of the POBA group participants (Fig. 1).
Participants were mainly patients with intermittent claudication with medium length femoropopliteal lesions (DCB group 5.9 cm, POBA group 5.6 cm). Twenty-three percent of the lesions were totally occluded and 49% severely or moderately calcified. Pre-dilation was conducted in 99% of the lesions in both treatment groups (Table 1). Detailed patient, lesion, and procedure characteristics were presented earlier [10]. The results of the post-hoc subgroup analysis on loss of primary patency are shown in Fig. 3.
Effectiveness Outcomes Through 5 Years
Superiority of primary patency after DCB angioplasty over POBA sustained throughout 5 years (Kaplan–Meier point estimate at 5 years: 61.4% vs. 53.5%; log-rank p = 0.040). The advantage of DCB over POBA decreased over time (Fig. 2A, Supplementary Table 2). Post hoc analysis could not demonstrate any significant interaction of subgroups with the treatment effect (overall loss of primary patency: HR 0.55 (95%CI 0.32 to 0.94) in favor of DCB; p = 0.03) (Fig. 3). The declining gap between DCB and POBA is especially obvious in the Kaplan–Meier estimates for freedom from CD-TLR after 2 years up to 5 years (Fig. 2B). Freedom from CD-TLR at 5 years did not differ significantly between groups (DCB 82.1% vs. POBA 73.7%, log-rank p = 0.050) (Fig. 2B). Freedom from TVR was 68.1% (95%CI 54.4 to 78.5) with DCB and 69.5% (95%CI 56.6 to 79.3) with POBA (log-rank p = 0.37).
Treatment effect of Luminor 35 DCB angioplasty in femoropopliteal lesions through 5 years. A Primary patency at 5 years was achieved significantly more often with Luminor 35 DCB angioplasty than with standard balloon angioplasty and B freedom from clinically driven target lesion revascularization did not differ significantly between groups. At 60 months, standard error was 6.9% and 6.4% for primary patency and 5.2% and 5.5% for CD-TLR in the DCB and POBA group, respectively. Bars represent 95% confidence intervals. DCB drug-coated balloon, POBA plain old balloon angioplasty, CD-TLR clinically driven target lesion revascularization
Post-hoc analysis of loss of primary patency by subgroups. Hazard ratios were determined over a period of 5 years and adjusted for study centers. The dotted line shows the no-effect point and the continuous line the overall treatment effect. DCB drug-coated balloon, CTO chronic total occlusion, POBA plain old balloon angioplasty
Rutherford classification of participants remained significantly shifted to more favorable categories compared to baseline in both groups. However, with inclusion of participants who had undergone CD-TLR in the analysis, the POBA group showed a more advantageous distribution of categories than the DCB group (Fig. 4A). If CD-TLR participants were excluded from the comparison, primary clinical improvement did not differ between groups (DCB 61.4% vs. POBA 64.4%, p = 0.94) (Fig. 4B). Secondary clinical improvement was 70.5% (31 of 44 participants) and 82.2% (37 of 45 participants) after DCB angioplasty and POBA, respectively (p = 0.22). Primary and secondary hemodynamic improvement was similar between groups (DCB 45% [12 of 31] vs. POBA 39% [15 of 33], p = 0.62, and DCB 48% [15 of 31] vs. POBA 70% [23 of 33 participants], p = 0.13, respectively).
Clinical improvement according to Rutherford classification. A Change in Rutherford category from baseline to follow-ups (participants who underwent TLR included), and B clinical improvement at 5 years. The boxed p-values concern differences in change from baseline between the DCB and the POBA group. Primary clinical improvement applied if the Rutherford category declined by at least one level without preceding target lesion revascularization. DCB drug-coated balloon, POBA plain old balloon angioplasty, TLR target lesion revascularization
Safety Outcomes through 5 Years
Incidence of restenosis, target limb amputation, or all-cause death at 5 years did not differ significantly between groups. Eleven percent (9 of 80) of the participants died after DCB angioplasty, and 16% (14 of 86) after POBA. No death occurred within 30 days after the procedure and no significant difference was seen regarding causes of deaths (Table 2). Kaplan–Meier estimate of freedom from all-cause death at 5 years was similar between groups (DCB 88.5% vs. POBA 86.0%, log-rank p-value 0.34) (Fig. 5, Supplementary Table 2).
Survival through 5 years. Kaplan–Meier curves show freedom from all-cause death after Luminor 35 DCB angioplasty or standard balloon angioplasty through 5 years. At 60 months, standard error was 3.6% and 3.8% in the DCB and POBA group, respectively. Bars represent 95% confidence intervals. DCB drug-coated balloon, POBA plain old balloon angioplasty
Discussion
The present study demonstrates Luminor® 35 DCB angioplasty of femoropopliteal lesions to be superior in terms of primary patency compared to POBA throughout 5 years, however, with a declining gap. Regarding freedom from CD-TLR, the advantage of DCB was still numerically apparent but no longer significant. Over the long term, treatment groups were largely similar with regards to clinical and hemodynamic improvement. Even at 5 years, all-cause mortality did not differ between both treatment groups.
Although, advantage of DCB over POBA decreased over time, benefit of DCB concerning prevention of restenosis is still evident over the long term. Our finding supports previous reports on the final clinical outcome of CD-TLR. Both the IN-PACT SFA study [7] and the AcoArt study [8] reported on favorable results on freedom from CD-TLR with DCB compared to POBA after 5 years (74.5% vs 65.3%, p = 0.02 and 77.5% vs. 59.1%, p < 0.001, respectively). Five-year cumulative incidence of freedom from CD-TLR after DCB in the large real world IN.PACT Global study [13] was somewhat lower (69.4%).
In the EffPac trial, the difference in CD-TLR between DCB and POBA at 5 years could no longer be considered significant as it has been at 42 months [14]. Notably, incidences of freedom from CD-TLR in both EffPac groups, DCB as well as POBA, were considerably higher as in the IN-PACT SFA and the AcoArt studies. Differences in effectiveness may be based on lesion complexity and treatment strategy [3]. In the AcoArt study, the share of participants with critical limb-threatening ischemia (CLTI) and diabetes was considerably higher compared to EffPac. In addition, lesions were longer and about one-quarter were in-stent restenosis. In the IN.PACT global registry, about 80% of participants were assigned to a “broader use” group with longer lesions and a high share of in-stent restenosis (21%). In the IN-PACT SFA randomized study, participants and lesions were closer to the EffPac trial, however, bailout stenting occurred less frequently. In both the AcoArt and the IN.PACT SFA study, pre-dilation was less frequently conducted in POBA than in DCB participants, which might have contributed to poorer outcomes after POBA. Vessel preparation is crucial for long-term outcomes. Therefore, the EffPac protocol required pre-dilation with POBA mandatorily in both study arms and the randomization was performed after pre-dilatation to assure that both study arms were pre-dilated equally.
Regardless of lesion characteristics and treatment strategies, effectiveness of DCB angioplasty might also be determined by the coating design (excipient, drug, drug dose, coating technology). In vitro tests showed that, depending on the adherence of the coating, material gets partly lost already during removal of the protective cover of the balloon [15] and subsequently, during transfer to the target lesion [16]. Paclitaxel loss during removal of the protective cover was reported to be considerably higher with IN.PACT Admiral than with Luminor® 35 DCB angioplasty [15]. However, conversely, in vitro abrasion of the coating from the uninflated balloon was found to be significantly more severe with Luminor® 35 [16]. Although a strong in vitro adherence of the coating is not inevitably associated with increased in vivo drug transfer into the vessel wall, drug loss might result in both unreliable clinical efficacy and increased risk of distal particulate embolization of amorphous- or crystalline-like material. Downstream loss of paclitaxel is held accountable for fibroid necrosis and inflammation in small arteries [17] that might be associated with slow flow [18]. However, in the EffPac trial, no treatment interaction of previously identified risk factors of slow flow, such as chronic total occlusion or poor distal runoff [19] became clinically evident. However, this might be due to the limited power of our subgroup analysis. In addition, particular embolization might be more critical in patients with long lesions and CLTI.
Against the background of the controversial debate on long-term safety of paclitaxel in peripheral interventions [4, 20,21,22] we completed the vital status in almost all participants. In accordance with a recent meta-analysis on paclitaxel-coated devices for predominately claudicant participants that included 9 randomized controlled trials with 5-year results [23], all-cause mortality in the EffPac trial did not differ between treatment groups. At 5 years, the meta-analysis found a somewhat higher all-cause mortality of 18.8% after paclitaxel-coated devices and a similar all-cause mortality of 15.9% after POBA (p = 0.08). There was no significant heterogeneity between studies.
Similar to the survival curves for freedom from TLR that have been reported previously [7, 8], in the EffPac study the advantage of DCB angioplasty over POBA decreased over time. This was mainly driven by a frequent loss of patency after POBA within the first 12 months. In contrast, DCB angioplasty considerably slowed down the decline of patency loss. We do not suspect any late catch-up phenomenon from continuous neointimal growth known from drug-eluting stents in the coronary arteries [24] because the half-live of paclitaxel is reported with 45 days after a single local administration with DCB [25]. According the “leaving nothing behind” principle the avoidance of primary stenting may eliminate another trigger for neointimal hyperplasia.
As a matter of fact, we are seeing a declining gap between DCB and POBA throughout 5 years. The Kaplan–Meier curves for primary patency and freedom from CD-TLR are clearly demonstrating the vanishing effectiveness of DCB compared to POBA over time (Fig. 2). Although there is still a significant difference in primary patency between DCB angioplasty and POBA at 5 years, it can be assumed that this effect will disappear after some time.
Finally, post-hoc subgroup analysis generates the hypothesis that loss of patency in patients at older age is similar with DCB and POBA (Fig. 3). This might be due to a reduced neointimal proliferation with age. Accordingly, a previous EffPac multivariable analysis showed less LLL at 6 months with advanced age independent of whether DCB or POBA was used [26]. Whether patients with poor distal runoff benefit more from DCB remains to be assessed.
Limitations
This trial has limitations. First, although vital status was obtained almost entirely, clinical and ultrasonography follow-up was completed in only about half of the participants. Second, the study was not powered to assess a difference in long-term all-cause mortality between the treatment groups. Finally, in this study we evaluated the Luminor® 35 DCB. Thus, results cannot be transferred automatically to other DCB types.
Conclusion
Long-term follow-up of the EffPac trial showed superiority in terms of primary patency after femoropopliteal Luminor® 35 DCB angioplasty compared to POBA over a period of 5 years. This finding was reflected by freedom from TLR, however, no longer with a significant difference. No safety signal occurred. From this, we can conclude that femoropopliteal Luminor® 35 DCB angioplasty is a sustainably efficacious and safe treatment approach.
References
Teichgräber U, Aschenbach R, Scheinert D, et al. The effectiveness of the paclitaxel-coated Luminor® balloon catheter versus an uncoated balloon catheter in superficial femoral and popliteal arteries in preventing vessel restenosis or reocclusion: study protocol for a randomized controlled trial. Trials. 2016;17(1):528.
Caradu C, Lakhlifi E, Colacchio EC, et al. Systematic review and updated meta-analysis of the use of drug-coated balloon angioplasty versus plain old balloon angioplasty for femoropopliteal arterial disease. J Vasc Surg. 2019;70(3):981–95.
Klumb C, Lehmann T, Aschenbach R, Eckardt N, Teichgräber U. Benefit and risk from paclitaxel-coated balloon angioplasty for the treatment of femoropopliteal artery disease: a systematic review and meta-analysis of randomised controlled trials. EClinicalMedicine. 2019;16:42–50.
Rocha-Singh KJ, Duval S, Jaff MR, et al. Mortality and paclitaxel-coated devices: an individual patient data meta-analysis. Circulation. 2020;141(23):1859–69.
Rocha-Singh KJ, Duval S. Statistical alchemy and the road ahead. JACC Cardiovasc Interv. 2019;12(24):2525–7.
Tepe G, Schnorr B, Albrecht T, et al. Angioplasty of femoral-popliteal arteries with drug-coated balloons: 5-year follow-up of the THUNDER trial. JACC Cardiovasc Interv (1 Pt A). 2015;8:102–8.
Laird JA, Schneider PA, Jaff MR, et al. Long-term clinical effectiveness of a drug-coated balloon for the treatment of femoropopliteal lesions. Circ Cardiovasc Interv. 2019;12(6):e007702.
Xu Y, Liu J, Zhang J, et al. Long-term safety and efficacy of angioplasty of femoropopliteal artery disease with drug-coated balloons from the AcoArt I trial. J Vasc Surg. 2021;74(3):756–62.
Ouriel K, Adelman MA, Rosenfield K, et al. Safety of paclitaxel-coated balloon angioplasty for femoropopliteal peripheral artery disease. JACC Cardiovasc Interv. 2019;12(24):2515–24.
Teichgräber U, Lehmann T, Aschenbach R et al. efficacy and safety of a novel paclitaxel-nano-coated balloon for femoro-popliteal angioplasty: 1-Year Results of EffPac Trial. EuroInterventiom. 2019.
Teichgräber U, Lehmann T, Aschenbach R, et al. Two-year review on mortality and morbidity after femoropopliteal drug-coated balloon angioplasty in the randomized EffPac trial. Radiology. 2020;296(3):638–40.
Teichgräber U, Lehmann T, Aschenbach R, et al. Drug-coated Balloon Angioplasty of Femoropopliteal Lesions Maintained Superior Efficacy over Conventional Balloon: 2-year Results of the Randomized EffPac Trial. Radiology. 2020;16: 191619.
Zeller T, Brodmann M, Ansel GM et al. Paclitaxel-coated balloons for femoropopliteal peripheral arterial disease: final five-year results of the IN.PACT Global Study. EuroIntervention. 2022.
Teichgräber U, Lehmann T, Aschenbach R, et al. Femoropopliteal Drug-coated Balloon Angioplasty: Long-term Results of the Randomized EffPac Trial. Radiology. 2022;304(1):225–7.
Faenger B, Heinrich A, Hilger I, Teichgräber U. drug loss from paclitaxel-coated balloons during preparation, insertion and inflation for angioplasty: a laboratory investigation. Cardiovasc Intervent Radiol. 2022;1–12
Heinrich A, Engler MS, Güttler FV, Matthäus C, Popp J, Teichgräber UK. Systematic evaluation of particle loss during handling in the percutaneous transluminal angioplasty for eight different drug-coated balloons. Sci Rep. 2020;10(1):17220.
Torii S, Jinnouchi H, Sakamoto A, et al. Comparison of biologic effect and particulate embolization after femoral artery treatment with three drug-coated balloons in healthy swine model. J Vasc Interv Radiol. 2019;30(1):103–9.
Tang TY, Sulaiman MSB, Soon SXY, Yap CJQ, Patel A, Chong TT. Slow-flow phenomena following lower limb paclitaxel- and sirolimus-coated balloon angioplasty in the setting of chronic limb threatening ischaemia-a case series. Quant Imaging Med Surg. 2022;12(3):2058–65.
Shirai S, Hirano K, Mori S, et al. Frequency, predictors, and effect of the slow-flow phenomenon after drug-coated balloon angioplasty for femoropopliteal lesions. Heart Vessels. 2021;36(12):1818–24.
Freisinger E, Koeppe J, Gerss J, et al. Mortality after use of paclitaxel-based devices in peripheral arteries: a real-world safety analysis. Eur Heart J. 2020;41(38):3732–9.
Secemsky EA, Barrette E, Bockstedt L, et al. Long-term safety of drug-coated devices for peripheral revascularisation. EuroIntervention. 2021;17(7):590–8.
Nordanstig J, James S, Andersson M, et al. Mortality with paclitaxel-coated devices in peripheral artery disease. N Engl J Med. 2020;383(26):2538–46.
Dinh K, Limmer AM, Chen AZL, et al. Mortality rates after paclitaxel-coated device use in patients with occlusive femoropopliteal disease: an updated systematic review and meta-analysis of randomized controlled trials. J Endovasc Ther. 2021;28(5):755–77.
Sgueglia GA, Cortese B, Gaspardone A. Late catch-up phenomenon after drug-eluting balloon angioplasty. Int J Cardiol. 2013;168(2):638–9.
Speck U, Cremers B, Kelsch B, et al. Do pharmacokinetics explain persistent restenosis inhibition by a single dose of paclitaxel? Circ Cardiovasc Interv. 2012;5(3):392–400.
Mietz S, Lehmann T, Teichgräber U. Multivariable regression analysis of clinical data from the randomized-controlled EffPac trial: efficacy of femoropopliteal drug-coated balloon angioplasty. Cardiovasc Interv Radiol. 2020;43(6):840–9.
Acknowledgements
The authors thank Isabella Schiller, Nicole Brillinger, and Tabitha Heller (Center of Clinical Trials Jena, Jena, Germany) for data management, and Laura Graziani (Department of Radiology, Jena University Hospital, Jena, Germany) for study coordination.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was supported by iVascular S.L.U., Barcelona, Spain and Endoscout, Freiburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
UT is a consultant for iVascular. TZ is co-principal investigator of the ILICO study, a study sponsored by iVascular. All other authors declare that they have no conflict of interest with respect to this article.
Ethical Approval
The study protocol was approved by the Friedrich-Schiller-University ethics committee. In addition, the study protocol had been approved by the local ethics committees of all participating sites. The study was conducted according to the Declaration of Helsinki.
Informed Consent
Written, informed consent to participate in the study was obtained from all patients.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Teichgräber, U., Lehmann, T., Ingwersen, M. et al. Long-Term Effectiveness and Safety of Femoropopliteal Drug-Coated Balloon Angioplasty : 5-Year Results of the Randomized Controlled EffPac Trial. Cardiovasc Intervent Radiol 45, 1774–1783 (2022). https://doi.org/10.1007/s00270-022-03265-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03265-1