Abstract
Purpose
Data on the long-term safety and effectiveness of drug-coated balloons (DCBs) for the treatment of long femoropopliteal atherosclerotic lesions in the real-world setting are rare. This study reports 3 year and 5 year outcomes of the pre-specified 150 mm balloon sub-cohort of the IN.PACT Global Study.
Methods
The IN.PACT Global Study was a prospective, multicentre, international, single-arm study evaluating the performance of the IN.PACT Admiral DCB in real-world patients with femoropopliteal atherosclerotic disease. This pre-specified 150 mm DCB cohort analysis comprised 107 participants (111 lesions) with all target lesions treated with at least one 150 mm DCB.
Results
Mean lesion length was 20.3 ± 9.2 cm; 18.0% had in-stent restenosis, 58.6% were totally occluded, and 17.1% were severely calcified. Through 60 months, the Kaplan–Meier estimate of freedom from clinically driven target lesion revascularization (CD-TLR) was 72.7% [95% confidence interval (CI):62.4%–80.5%]. The safety composite endpoint (freedom from device/procedure-related death through 30 days; freedom from target limb major amputation and clinically driven target vessel revascularization through 5 years) was 70.5%. The cumulative incidence of major amputation was 1.0% and all-cause mortality was 18.4% through 60 months. Freedom from CD-TLR rates in the provisional stented and non-stented subgroups through 36 months were 64.0% [95% CI: 46.1%–77.3%] and 81.9% [95% CI: 69.7%–89.6%] (log-rank p = 0.074), respectively.
Conclusions
The results demonstrate sustained long-term safety of the 150 mm IN.PACT Admiral DCB for long femoropopliteal atherosclerotic lesions in real-world patients. In particular, the results show that DCB angioplasty is an effective revascularization modality in long complex lesions. ClinicalTrials.gov identifier: NCT01609296.
Level of Evidence.
Level 3, Cohort Study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endovascular strategies have been considered as first-line therapy for revascularization in patients with peripheral artery disease (PAD) and femoropopliteal lesions up to 25 cm in length [1]. Among these, the paclitaxel drug-coated balloon (DCB) has emerged as a significant innovation that provides effective clinical outcomes without a permanent scaffold. For femoropopliteal arterial lesions, several randomized controlled trials (RCTs) have demonstrated the superior performance of DCBs compared to standard percutaneous transluminal angioplasty (PTA) [2,3,4,5,6,7]. While these promising outcomes recognized DCBs as a preferred choice over PTA, the lesions included in most RCTs are limited to shorter and less complex lesions, while longer lesions are often excluded. Although single-arm studies suggest the potential of DCBs for long lesions through 1 and 2 year follow-up [8,9,10], there are no long-term data available in real-world settings. Moreover, data on long balloons for long lesions are not available
The IN.PACT Global Study was a large prospective study designed to evaluate the performance of the paclitaxel-coated IN.PACT Admiral DCB (Medtronic, Dublin, Ireland) for the treatment of real-world patients with atherosclerotic disease of the superficial femoral artery (SFA) and/or the entire popliteal artery. A prospective analysis of a pre-specified cohort of participants with long lesions treated with the 150 mm IN.PACT Admiral DCB within the IN.PACT Global Study is presented in this paper. Herein, we report the 3 year and 5 year outcomes of the 150 mm cohort.
Methods
Study Design
The IN.PACT Global Study, a prospective, multicenter, international, single-arm clinical study, was designed to assess the safety and effectiveness of a paclitaxel-coated DCB for the treatment of real-world patients. In the full cohort, 1535 participants were enrolled across 64 sites in 26 countries from Europe, the Middle East, Asia, North Africa, Australia, Canada, and Latin America from 2012 to 2014. Outcomes from the full clinical cohort through 3 years have been previously reported [11,12,13]. The study included participants with intermittent claudication and/or rest pain [Rutherford categories (RC) 2–4] because of obstructive disease of the femoropopliteal artery. Lesions were located in the full native SFA and/or the full popliteal artery (P1–P3). Minimal selection criteria were applied to better represent the patient profile treated in the actual clinical practice in accordance with real-world evidence [14]. The present analysis included a pre-specified as-treated cohort, in which all target lesions were treated with at least one 150 mm DCB, thus assessing the treatment effect of long balloons for long complex lesions. Participants were followed for a total of 60 months. Participants had hospital visit evaluations through 36 months. At 48 and 60 months, participants had phone follow-up and the occurrence of reintervention, adverse events, and health status were assessed.
An independent Clinical Events Committee (CEC) managed by Syntactx, New York, NY, USA adjudicated all major adverse events (MAEs) including clinically driven target lesion revascularizations (CD-TLRs), clinically driven target vessel revascularizations (CD-TVRs) major target limb amputation, thrombosis at the target lesion site, and deaths through 60 months after the index procedures.
The institutional review board or ethics committee at each study site approved the study protocol. Informed consent was obtained from all patients prior to enrollment. The study was conducted in accordance with the Declaration of Helsinki, good clinical practice guidelines, and applicable laws as specified by all relevant governmental bodies. The trial was registered on the National Institutes of Health website (ClinicalTrials.gov identifier: NCT01609296).
Outcome Measures
Assessments through 36 months included freedom from CD-TLR; the safety endpoint, a composite of freedom from device- and procedure-related mortality through 30 days and freedom from major target limb amputation and CD-TVR within 36 months after the index procedure; primary sustained clinical improvement, defined as a sustained upward shift of at least 1 RC compared to baseline without the need for repeated TLR or surgical revascularization in amputation-free surviving patients; secondary sustained clinical improvement, defined as a sustained upward shift of at least 1 RC compared with baseline, including the need for repeated TLR or surgical revascularization in amputation-free surviving patients; and the incidence of MAEs (all-cause mortality, CD-TVR, major target limb amputation, and thrombosis at the target lesion site), CD-TLR, any TVR, and any TLR. Assessments through 60 months included the safety composite endpoint, and the incidence of MAEs. CD-TLR was defined as any reintervention within the target lesion(s) because of symptoms or drop of ankle-brachial index (ABI) of ≥ 20% or > 0.15 when compared with post-index procedure baseline ABI; CD-TVR was defined as any reintervention within the target vessel due to symptoms or a reduction in ABI ≥ 20% or > 0.15 when compared with the post-index procedure baseline ABI; severe calcification was defined as a circumference ≥ 180° on both sides of the vessel at the same location and lengths greater than or equal to half of the total lesion length [15]. All repeat interventions on the target limbs, including TLR, TVR, and the clinically driven status, were reviewed and adjudicated by the CEC.
Statistical Analysis
All baseline demographics and clinical characteristics were summarized on a participant basis and lesion characteristics were summarized on a lesion basis, unless otherwise specified. For baseline characteristics, continuous variables are described as mean ± standard deviation; dichotomous and categorical variables are described as counts and proportions. The outcome analysis was performed at a patient level. The Kaplan–Meier method was used to evaluate time-to-event data for freedom from CD-TLR and freedom from mortality through 60 months and cumulative incidence for other outcomes where applicable. The Kaplan–Meier analysis for CD-TLR by provisional stent usage was truncated at 1080 days because fewer than 30 patients were in the stent group at the start of 1080 days. Confidence intervals (95%) for the Kaplan–Meier method were derived using the log–log method. The difference in the survival curves between subgroups was assessed using the log-rank test. Time to event was also summarized using the restricted mean survival time (RMST) with a horizon of 1080 days and 1800 days for 3 years and 5 years, respectively. The RMST is the average time to an event within a fixed time period and corresponds to the area under the survival curve from the start of follow-up to the fixed time point. It incorporates participants with events, censoring, and those with complete follow-up through the time period without an event. Estimates are presented with the 95% confidence interval (CI) where applicable. All summaries were based on non-missing assessments. Time is presented in years and months where 1 year equals 360 days and one month equals 30 days. A significance level of 0.05 was used and no adjustment was made for multiple testing. Statistical analyses were performed using SAS (version 9.4; SAS Institute, Cary, NC, USA).
Results
Participant Population
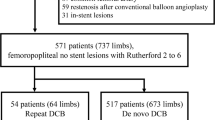
In the 150 mm DCB cohort, 119 participants were enrolled, of which 12 patients either did not receive a DCB or did not have all target lesions treated with at least one 150 mm DCB. The remaining 107 participants had all target lesions treated with at least one 150 mm DCB, referred to here as the as-treated 150 mm DCB cohort and included in the analysis (Fig. 1). Baseline demographics and lesion characteristics of the as-treated 150 mm cohort are reported in Table 1 and Table 2. The mean age of participants was 68.0 ± 9.3 years and 76.6% were male. Within this cohort, a significant percentage of participants had diabetes mellitus (41.1%), hyperlipidemia (75.7%), and coronary artery disease (38.8%). The mean lesion length was 20.3 ± 9.2 cm (median 18.0 cm, range 3.0–42.0 cm). Among lesions, 18.0% were in-stent restenosis (ISR) and 58.6% were totally occluded. Most of the lesions were calcified (87.4%) including 17.1% that were severely calcified (circumference ≥ 180° on both sides of the vessel at the same location and lengths greater than or equal to half of the total lesion length). The participant flow through 60 months is shown in Fig. 1. The follow-up compliance rates at 36 and 60 months were 93.0% (80/86) and 92.4% (73/79), respectively.
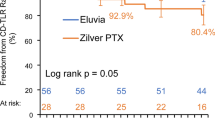
Effectiveness and Safety Outcomes Through 36 Months
The Kaplan–Meier estimate of freedom from CD-TLR in the 150 mm DCB cohort was 75.2% (95% CI: 65.2%–82.6%; Fig. 2). The RMST to first CD-TLR with a time horizon of 36 months was 948.4 days (95% CI: 897.0–999.8 days; Table 3). Primary and secondary sustained clinical improvement rates were 65.5% (55/84) and 82.7% (67/81), respectively (Table 3). The Kaplan–Meier estimate of freedom from CD-TLR in the stented versus non-stented subgroups within the as-treated 150 mm cohort was 64.0% (95% CI 46.1%–77.3%) versus 81.9% (95% CI 69.7%–89.6%; log-rank p = 0.074; Fig. 3), respectively.
Kaplan–Meier estimate of freedom of CD-TLR through 36 months in the stented versus non-stented subsets of the IN.PACT Global as-treated 150 mm DCB cohort. The baseline characteristics of these two subsets are reported in Supplementary Table 1. Bars represent the 95% confidence intervals. CD-TLR, clinically driven target lesion revascularization
The safety endpoint, a composite of freedom from device- and procedure-related mortality through 30 days and freedom from major target limb amputation and CD-TVR within 36 months, was 74.2% (Table 3). The cumulative incidence of all-cause death was 13.1% through 36 months. There was only one case of target limb major amputation through 36 months (cumulative incidence rate of 1.0%); this patient was classified as RC 6 at baseline, enrolled due to protocol deviation. The rate of thrombosis at the target lesion site was 2.0%. The cumulative incidence for the MAE composite (all-cause death, major target limb amputation, CD-TVR, thrombosis at the target lesion site) rate was 35.8% through 3 years (Table 3).
Effectiveness and Safety Outcomes Through 60 Months
Through 60 months, the Kaplan–Meier estimate of freedom from CD-TLR in the 150 mm DCB cohort was 72.7% (95% CI: 62.4%–80.5%; Fig. 2). The Kaplan–Meier estimate of the safety composite endpoint was 70.5% (Table 4) and the freedom from all-cause mortality was 81.6% (95% CI: 72.4%–88.0%; Fig. 4). There was no additional major target limb amputation between 36- and 60-month follow-up. The cumulative incidence of CD-TVR was 29.5% through 60 months.
Discussion
Long lesions, along with chronic total occlusions (CTO) and calcified lesions of the femoropopliteal vessel bed, are seen frequently in daily practice yet are some of the most challenging lesions to treat. PTA performs poorly in longer lesions (> 10 cm) with 1 year restenosis rates of over 70% [16]. High rates of restenosis have also been reported after stenting with bare metal stents (BMS) in long SFA lesions. ISR occurs with a frequency of 20%–40% at 1 year for lesions < 15 cm [17,18,19]. There is a paucity of data for longer femoropopliteal lesions (> 15 cm), but the rate of ISR in these long lesions after stenting is likely to be upwards of 50%. Furthermore, these restenotic lesions often present with diffuse ISR, which represents an additional challenge.
The current analysis reports outcomes from the pre-specified 150 mm DCB cohort of the IN.PACT Global Study, which is distinct from the IN.PACT Global long lesion imaging cohort (clinical cohort) published previously [8]. In the as-treated 150 mm cohort, participants had all target lesions treated with at least one 150 mm DCB, whereas the balloon size was not restricted in the clinical cohort. Similar to the clinical cohort, participants had complex, calcified, and long femoropopliteal lesions. The results demonstrated sustained safety and clinical benefit of the 150 mm long IN.PACT Admiral DCB for long lesions with low rates of reinterventions and low major amputations through 5 years. Previously, a meta-analysis reported an association between the use of paclitaxel-coated devices and late mortality [20], although patient-level meta-analyses and large real-world registries could not authenticate the findings [21,22,23,24,25,26,27,28,29,30,31]. Nonetheless, to address the concern of long-term safety in this cohort, safety outcomes were analyzed out to 5 years and results showed sustained safety throughout the 5 year follow-up.
There are limited global registries that reported outcomes through 3 or 5 years. We compared the results of the present study to that of RCTs even though the inclusion criteria of RCTs are mostly restricted to less complex and shorter lesions. The Kaplan–Meier estimate of freedom from CD-TLR was 75.2% through 3 years in this 150 mm DCB cohort compared to 84.5% for DCBs in the IN.PACT SFA RCT [5], 83.6%–85.3% for drug-eluting stents (DES) [32; 33] and 69.7%–75.5% for BMS [34; 35]. A 4 year freedom from CD-TLR of 76.7% was reported for the DCB arm in the ILLUMENATE Pivotal study [36]. There were only two reinterventions reported between 3 and 4 years, and none past 4 years; as a result, the freedom from CD-TLR was well sustained through 5 years (72.7%) in this 150 mm DCB cohort. The 5 year freedom from CD-TLR rate (72.7%) was comparable to the freedom from CD-TLR rates of the DCB arm in prior RCTs: 79% in the THUNDER trial [37], 74.5% in the IN.PACT SFA trial [38] and 83.1% in the Zilver PTX RCT [33]. Of note, the mean lesion lengths were much shorter in the aforementioned RCTs (6.6–8.9 cm) compared to the 150 mm cohort of the current study (20.3 cm). The 5 year freedom from CD-TLR of 72.7% in the 150 mm cohort is also favorable compared to the full clinical cohort of the IN.PACT Global Study (69.4%; mean lesion length 12.1 cm) [39], suggesting that treating long lesions with long balloons may be more effective than multiple overlapped balloons.
The provisional stenting rate of 36.4% in this 150 mm cohort is higher than those reported for DCB RCTs [3; 7], which is expected considering the longer mean lesion length (20.3 cm), and the presence of CTO (58.6%) and severely calcified lesions (17.1%) in the 150 mm cohort. Furthermore, this provisional stenting rate is in line with other long lesion cohorts of DCB studies; 35.7% in the long lesion cohort of the Lutonix Global SFA registry [40] and 39.4% in the long lesion imaging cohort of the IN.PACT Global study [41]. The Kaplan–Meier freedom from CD-TLR estimates were numerically higher in the non-stented group (81.9% non-stented vs. 64.0% stented), although the difference was not statistically significant. While the sample sizes were too small to allow any definitive conclusion, it is interesting to see a marked drop in the freedom from CD-TLR at 24 months in the stented subgroup. This may suggest a signal toward decreased effectiveness for provisional stents in long lesions. However, these exploratory findings will need to be confirmed in a larger prospective analysis. The results also suggest that vessel preparation strategies that reduce the need for provisional stenting may improve DCB outcomes further.
Despite the long and complex lesions, the results of this study demonstrated durable safety of treatment with long DCBs in this patient population. The freedom from the safety composite endpoint was high (70.5%) through 5 years. There was only one major target limb amputation (RC 6 at baseline and to be considered a protocol deviation) through 5 years and no device- or procedure-related deaths were found. The cumulative incidence of thrombosis at the target lesion site was also low through 5 years (3.2%). The 5 year all-cause mortality rate of 18.4% in the present study was consistent with the 5 year rates reported (10%–52%) among patients diagnosed with PAD in epidemiologic studies [42; 43]. The 5 year freedom from mortality (survival) rate reported in the present study (81.6%) was also aligned with the rates observed in PAD endovascular studies. Miura et al. reported an 83.4% 5 year survival in an overall claudicant patient population but a survival rate of 53.5% in high-risk claudicant patients. [44] In another retrospective analysis of consecutive patients who underwent femoropopliteal endovascular interventions, Kumins et al. reported 4 year survival rates of 80.7%–46.6% in patients treated with paclitaxel-coated devices and survival rates of 64.4%–32.8% in patients treated with non-paclitaxel devices [45]. The authors also concluded that the paclitaxel-treated group had an improved survival rate compared to the non-paclitaxel group in younger patients (< 60 years). Previously, two pool analyses reports have demonstrated the lack of an association between mortality and this DCB [46; 47].
Limitations: This is a prospective and pre-specified cohort, yet it was enrolled non-consecutively. Other limitations include the single-arm design of the study and a lack of an active comparator group, unlike RCTs. Therefore, the results could not be compared directly with other modalities. Clinic visits were conducted through 3 years; however, only phone follow-up data were available for 4 and 5 years. Anatomical data were not available for analysis of follow-up outcomes in this cohort.
Conclusion
The results of this analysis demonstrate sustained long-term safety of the 150 mm IN.PACT Admiral DCB for the treatment of obstructive, long femoropopliteal atherosclerotic lesions in real-world patients. The results also show that DCB angioplasty is an effective revascularization modality in long complex lesions.
Impact on Daily Practice
There are limited long-term publications on the safety and effectiveness of paclitaxel-coated DCBs for the treatment of long and complex femoropopliteal atherosclerotic lesions in the real-world setting. The long-term outcomes from this global cohort showed that the 150 mm IN.PACT Admiral DCB is safe with no device- or procedure-related deaths, has low rates of amputation, and is highly effective as a standalone therapy or in conjunction with provisional stenting in the treatment of long SFA and popliteal complex lesions.
Change history
28 August 2022
The citations for Fig. 3 and Fig. 4 on page 8 have been switched to their correct positions.
Abbreviations
- ABI:
-
Ankle-Brachial Index
- BMS:
-
Bare Metal Stent
- CEC:
-
Clinical Events Committee
- CD-TLR:
-
Clinically Driven Target Lesion Revascularization
- CD-TVR:
-
Clinically Driven Target Vessel Revascularization
- CTO:
-
Chronic Total Occlusion
- DCB:
-
Drug-Coated Balloon
- DES:
-
Drug-Eluting Stent
- ISR:
-
In-Stent Restenosis
- MAE:
-
Major Adverse Event
- PAD:
-
Peripheral Artery Disease
- PTA:
-
Percutaneous Transluminal Angioplasty
- RC:
-
Rutherford Category
- RCT:
-
Randomized Controlled Trial
- SFA:
-
Superficial Femoral Artery
References
Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763–816.
Laird JR, Schneider PA, Tepe G, et al. Durability of treatment effect using a drug-coated balloon for femoropopliteal lesions: 24-month results of in: PACT SFA. J Am Coll Cardiol. 2015;66(21):2329–38.
Tepe G, Laird J, Schneider P, et al. Drug-coated balloon versus standard percutaneous transluminal angioplasty for the treatment of superficial femoral and popliteal peripheral artery disease: 12-month results from the in: PACT SFA randomized trial. Circulation. 2015;131(5):495–502.
Iida O, Soga Y, Urasawa K, et al. Drug-coated balloon vs standard percutaneous transluminal angioplasty for the treatment of atherosclerotic lesions in the superficial femoral and proximal popliteal arteries: 1 year results of the MDT-2113 SFA Japan randomized trial. J Endovasc Ther. 2018;25(1):109–17.
Schneider PA, Laird JR, Tepe G, et al. Treatment effect of drug-coated balloons is durable to 3 years in the femoropopliteal arteries: long-term results of the in: PACT SFA randomized trial. Circ Cardiovasc Interv. 2018;11(1):e005891.
Krishnan P, Faries P, Niazi K, et al. Stellarex drug-coated balloon for treatment of femoropopliteal disease: twelve-month outcomes from the randomized ILLUMENATE pivotal and pharmacokinetic studies. Circulation. 2017;136(12):1102–13.
Rosenfield K, Jaff MR, White CJ, et al. Trial of a paclitaxel-coated balloon for femoropopliteal artery disease. N Engl J Med. 2015;373(2):145–53.
Scheinert D, Micari A, Brodmann M, et al. Drug-coated balloon treatment for femoropopliteal artery disease. Circ Cardiovasc Interv. 2018;11(10):e005654.
Micari A, Nerla R, Vadala G, et al. 2-Year results of paclitaxel-coated balloons for long femoropopliteal artery disease: evidence from the SFA-long study. JACC Cardiovasc Interv. 2017;10(7):728–34.
Tepe G, Zeller T, Moscovic M, et al. Paclitaxel-coated balloon angioplasty for the treatment of infrainguinal arteries: 24-month outcomes in the full cohort of BIOLUX P-III global registry. Cardiovasc Intervent Radiol. 2021;44(2):207–17.
Zeller T, Brodmann M, Micari A, et al. Drug-coated balloon treatment of femoropopliteal lesions for patients with intermittent claudication and ischemic rest pain. Circ Cardiovasc Interv. 2019;12(1):e007730.
Micari A, Brodmann M, Keirse K, et al. Drug-coated balloon treatment of femoropopliteal lesions for patients with intermittent claudication and ischemic rest pain: 2-Year results from the IN: PACT global study. JACC Cardiovasc Interv. 2018;11(10):945–53.
Torsello G, Stavroulakis K, Brodmann M, et al. Three-year sustained clinical efficacy of drug-coated balloon angioplasty in a real-world femoropopliteal cohort. J Endovasc Ther. 2020;27(5):693–705.
Jarow JP, LaVange L, Woodcock J. Multidimensional evidence generation and FDA regulatory decision making: defining and using “real-world” data. JAMA. 2017;318(8):703–4.
Dattilo R, Himmelstein SI, Cuff RF. The compliance 360 degrees Trial: a randomized, prospective, multicenter, pilot study comparing acute and long-term results of orbital atherectomy to balloon angioplasty for calcified femoropopliteal disease. J Invasive Cardiol. 2014;26(8):355–60.
Capek P, McLean GK, Berkowitz HD. Femoropopliteal angioplasty factors influencing long-term success. Circulation. 1991;83(2 Suppl):I70-80.
Schillinger M, Sabeti S, Loewe C, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354(18):1879–88.
Chalmers N, Walker PT, Belli AM, et al. Randomized trial of the smart stent versus balloon angioplasty in long superficial femoral artery lesions: the super study. Cardiovasc Intervent Radiol. 2013;36(2):353–61.
Laird JR, Katzen BT, Scheinert D, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the resilient randomized trial. Circ Cardiovasc Interv. 2010;3(3):267–76.
Katsanos K, Spiliopoulos S, Kitrou P, Krokidis M, Karnabatidis D. Risk of death following application of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2018;7(24):e011245.
Secemsky EA, Kundi H, Weinberg I, et al. Association of survival with femoropopliteal artery revascularization with drug-coated devices. JAMA Cardiol. 2019;4(4):332–40.
Bertges DJ, Sedrakyan A, Schermerhorn ML, et al. RS01 mortality after paclitaxel coated balloon angioplasty and stenting of superficial femoral and popliteal artery. J Vasc Surg. 2019;69(6):e98–9.
Donas KP, Sohr A, Pitoulias GA, Alfonso F, Torsello G. Long-term mortality of matched patients with intermittent claudication treated by high-dose paclitaxel-coated balloon versus plain balloon angioplasty: a real-world study. Cardiovasc Intervent Radiol. 2020;43(1):2–7.
Freisinger E, Koeppe J, Gerss J, et al. Mortality after use of paclitaxel-based devices in peripheral arteries: a real-world safety analysis. Eur Heart J. 2020;41(38):3732–9.
Kumins NH, King AH, Ambani RN, et al. (2020) Paclitaxel-coated peripheral artery devices are not associated with increased mortality. J Vasc Surg
Behrendt CA, Sedrakyan A, Peters F, et al. (2020) Long term survival after femoropopliteal artery revascularisation with paclitaxel coated devices: a propensity score matched cohort analysis. Eur J Vasc Endovasc Surg
Dinh K, Gomes ML, Thomas SD, et al. Mortality after paclitaxel-coated device use in patients with chronic limb-threatening ischemia: a systematic review and meta-analysis of randomized controlled trials. J Endovasc Ther. 2020;27(2):175–85.
Nordanstig J, James S, Andersson M, et al. Mortality with paclitaxel-coated devices in peripheral artery disease. N Engl J Med. 2020;383(26):2538–46.
Gutierrez JA, Rao SV, Jones WS, et al. Survival and causes of death among veterans with lower extremity revascularization with paclitaxel-coated devices: insights from the veterans health administration. J Am Heart Assoc. 2021;10(4):e018149.
Ullah W, Zghouzi M, Sattar Z, et al. Safety and efficacy of drug-coated balloon for peripheral artery revascularization-a systematic review and meta-analysis. Catheter Cardiovasc Interv. 2022;99(4):1319–26.
Secemsky EA, Song Y, Schermerhorn M, Yeh RW. Update from the longitudinal assessment of safety of femoropopliteal endovascular treatment with paclitaxel-coated devices among medicare beneficiaries: the SAFE-PAD study. Circ Cardiovasc Interv. 2022;181(8):1071–80.
Muller-Hulsbeck S, Keirse K, Zeller T, Schroe H, Diaz-Cartelle J. Long-term results from the MAJESTIC Trial of the eluvia paclitaxel-eluting stent for femoropopliteal treatment: 3-year follow-up. Cardiovasc Intervent Radiol. 2017;40(12):1832–8.
Dake MD, Ansel GM, Jaff MR, et al. (2016) Durable clinical effectiveness with paclitaxel-eluting stents in the femoropopliteal artery: 5-year results of the Zilver PTX randomized trial. circulation, 133(15): 1472–1483; discussion 1483
Laird JR, Katzen BT, Scheinert D, et al. (2012) Nitinol stent implantation vs. balloon angioplasty for lesions in the superficial femoral and proximal popliteal arteries of patients with claudication: three-year follow-up from the RESILIENT randomized trial. J Endovasc Ther, 19(1): 1–9
Rocha-Singh KJ, Bosiers M, Schultz G, et al. A single stent strategy in patients with lifestyle limiting claudication: 3-year results from the durability II trial. Catheter Cardiovasc Interv. 2015;86(1):164–70.
Lyden SP, Faries PL, Niazi KAK, et al. (2022) No Mortality Signal With Stellarex Low-Dose Paclitaxel DCB: ILLUMENATE Pivotal 4-Year Outcomes. J Endovasc Ther:15266028211068769
Tepe G, Schnorr B, Albrecht T, et al. (2015) Angioplasty of femoral-popliteal arteries with drug-coated balloons: 5-year follow-up of the THUNDER trial. JACC Cardiovasc Interv, 8(1 Pt A):102–108
Laird JA, Schneider PA, Jaff MR, et al. Long-Term Clinical Effectiveness of a Drug-Coated Balloon for the Treatment of Femoropopliteal Lesions. Circ Cardiovasc Interv. 2019;12(6): e007702.
Zeller T, Brodmann M, Ansel GM, et al. (2022) Paclitaxel-coated balloons for femoropopliteal peripheral arterial disease: final five-year results of the IN.PACT Global Study. EuroIntervention. https://doi.org/10.4244/EIJ-D-21-01098.
Thieme M, Von Bilderling P, Paetzel C, et al. The 24-Month Results of the Lutonix Global SFA Registry: Worldwide Experience With Lutonix Drug-Coated Balloon. JACC Cardiovasc Interv. 2017;10(16):1682–90.
Scheinert D (2018) Drug-Coated Balloon Treatment for Femoropopliteal Artery Disease: The IN.PACT Global Study Long Lesion Imaging Cohort. Circ Cardiovasc Interv, 11:e005654
Caro J, Migliaccio-Walle K, Ishak KJ, Proskorovsky I. The morbidity and mortality following a diagnosis of peripheral arterial disease: long-term follow-up of a large database. BMC Cardiovasc Disord. 2005;5:14.
Mueller T, Hinterreiter F, Luft C, Poelz W, Haltmayer M, Dieplinger B. Mortality rates and mortality predictors in patients with symptomatic peripheral artery disease stratified according to age and diabetes. J Vasc Surg. 2014;59(5):1291–9.
Miura T, Soga Y, Miyashita Y, et al. Five-year prognosis after endovascular therapy in claudicant patients with iliofemoral artery disease. J Endovasc Ther. 2014;21(3):381–8.
Kumins NH, King AH, Ambani RN, et al. Paclitaxel-coated peripheral arterial devices are associated with reduced mortality in younger patients. Ann Vasc Surg. 2021;70:70–8.
Schneider PA, Laird JR, Doros G, et al. Mortality not correlated with paclitaxel exposure: an independent patient-level meta-analysis of a drug-coated balloon. J Am Coll Cardiol. 2019;73(20):2550–63.
Schneider PA, Brodmann M, Mauri L, et al. Paclitaxel exposure: long-term safety and effectiveness of a drug-coated balloon for claudication in pooled randomized trials. Catheter Cardiovasc Interv. 2020;96(5):1087–99.
Dorros G, Cowley MJ, Simpson J, et al. Percutaneous transluminal coronary angioplasty: report of complications from the national heart, lung, and blood institute PTCA registry. Circulation. 1983;67(4):723–30.
Acknowledgements
The authors would like to acknowledge Stefanie Deckers, MS (Medtronic) for clinical support and Sangeeta Yendrembam, PhD (Medtronic) for medical writing assistance in accordance with Good Publication Practice guidelines (http://www.ismpp.org/gpp3).
Funding
Open access funding provided by Medical University of Graz. This study was funded by Medtronic. The funder of the study was involved in the study design, data collection, data analysis, data interpretation, and provided medical writing support. The authors had full access to all the data, interpretation and manuscript writing and had full and final responsibility for the decision to submit for publication. Authors received no specific funding for this work or for preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
Marianne Brodmann has received speaking honoraria from Bard Peripheral Vascular, Biotronik, Medtronic, Philips‐Spectranetics, Shockwave, Bayer Healthcare, and VIVA Physicians; and is a consultant for Bard Peripheral Vascular, Bayer, Biotronik, Intact Vascular, Medtronic, Philips‐Spectranetics, Sanofi, and Shockwave.
Wouter Lansink has received speaking honoraria from Abbott, Bard Peripheral, Biotronik, Boston Scientific, Medtronic, and Philips-Spectranetics and has received clinical trial funds from Bard Peripheral, Biotronik, Boston Scientific, I-vascular, Medtronic, and Philips-Spectranetics.
Katharina Guetl has nothing to disclose.
Antonio Micari has served as a member of the advisory board for Boston Scientific and Medtronic and has served as a consultant for Bard, Boston Scientific, and Terumo.
Jeremiah Menk is a full-time employee of Medtronic Inc., Minneapolis, MN.
Thomas Zeller has received honoraria from Abbott Vascular, Biotronik, Boston Scientific, Cook Medical, Gore and Associates, Medtronic, Philips‐Spectranetics, TriReme, Shockwave, and Veryan; has served as a consultant for Bayer, B. Braun, Boston Scientific, Cook Medical, Gore and Associates, Intact Vascular, Medtronic, Shockwave, Philips-Spectranetics, Veryan, and Vesper Medical; has received research, clinical trial, or drug study funds from 480 biomedical, Bard Peripheral Vascular, B. Braun, Biotronik, Cook Medical, Gore and Associates, Intact Vascular, Med Alliance, Medtronic, Philips-Spectranetics, Terumo, TriReme, and Shockwave; and owns common stock in QT Medical and Veryan.
Ethical Approval.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
The Institutional Review Board or Ethics Committee at each study site approved the study protocol.
Consent for Publication
For this type of study, consent for publication is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brodmann, M., Lansink, W., Guetl, K. et al. Long-Term Outcomes of the 150 mm Drug-Coated Balloon Cohort from the IN.PACT Global Study. Cardiovasc Intervent Radiol 45, 1276–1287 (2022). https://doi.org/10.1007/s00270-022-03214-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03214-y