Abstract
Objectives
To evaluate the efficacy and safety of TAE/TACE versus emergency surgery (ES) for spontaneous rupture of HCC (rHCC).
Methods
Eight databases (Web of Science, Pubmed, Embase, Cochrane Library, ClinicalTrial.gov, Wanfang, CNKI and VIP) were searched to obtain all related literature from the inception dates to October 2019. Subgroup analyses based on the kind of study design and kind of embolization were conducted.
Results
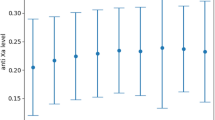
Twenty-one studies comparing TAE/TACE with ES were eligible. A total of 974 rHCC participants (485 participants treated with TACE/TAE and 489 participants treated with ES) were included in the present meta-analysis. TAE/TACE group was associated with lower risk of complications (OR = 0.36; 95% CI, 0.22–0.57; P < 0.0001) and in-hospital mortality (OR = 0.52; 95% CI, 0.29–0.94; P = 0.03) compared with ES group. In addition, no significant difference in successful hemostasis (OR = 1.67; 95% CI, 0.85–3.28; P = 0.13) and 1-year survival (OR = 1.08; 95% CI, 0.79–1.48; P = 0.64) between TAE/TACE and ES groups was demonstrated.
Conclusions
TAE/TACE had comparable outcomes to ES in terms of successful hemostasis and 1-year survival. Meanwhile, TAE/TACE was significantly superior to ES in terms of complications and in-hospital mortality. Therefore, TAE/TACE may be recommended as a preferable treatment for rHCC.







Similar content being viewed by others
References
Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma: a systematic review. Arch Surg. 2006;141(2):191–8.
Chiappa A, Zbar A, Audisio RA, et al. Emergency liver resection for ruptured hepatocellular carcinoma complicating cirrhosis. Hepatogastroenterology. 1999;46(26):1145–50.
Hai L, Yong-Hong P, Yong F, et al. One-stage liver resection for spontaneous rupture of hepatocellular carcinoma. World J Surg. 2005;29(10):1316–8.
Yeh CN, Lee WC, Jeng LB, et al. Spontaneous tumour rupture and prognosis in patients with hepatocellular carcinoma. Br J Surg. 2002;89:1125–9.
Yoshida H, Mamada Y, Taniai N, et al. Long-term results of elective hepatectomy for the treatment of ruptured hepatocellular carcinoma. J Hepato Biliary Pancreat Surg. 2008;15(2):178–82.
Lin XJ. The efficacy and prognosis analysis of transarterial chemoembolization versus surgery in the treatment of spontaneous rupture of hepatocellular carcinoma. J Med Theor Pract. 2018;31(24):3697–9.
Xu KY, Huang YH, Tao CL, et al. The outcome of patients with spontaneous ruptured hepatocellular carcinoma: comparing surgical resection and tanscatheter aterial embolization for therapy. J Hepato Pancreato Biliary Surg. 2014;26(1):9–11.
Chen MY. The outcome of emergency surgery versus transarterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma [D]. Fujian: Fujian medical university; 2011.
Zhang GJ, Wu SD, Sun QX, et al. The study of hepatectomy on patients of spontaneous rupture of small hepatocellular carcinoma after TACE. J Hepato Pancreato Biliary Surg. 2014;26(3):188–91.
Battula N, Madanur M, Priest O, et al. Spontaneous rupture of hepatocellular carcinoma: a Western experience. Am J Surg. 2009;197(2):164–7.
Li Q, Ao GK, Duan F, et al. Incidence and therapeutic frequency of extrahepatic collateral arteries in transcatheter arterial chemoembolization of hepatocellular carcinoma: Experience from 182 patients with survival time more than 3 years. Eur J Radiol. 2015;84(12):2555–63.
Miyayama S, Matsui O, Taki K, et al. Extrahepatic blood supply to hepatocellular carcinoma: angiographic demonstration and transcatheter arterial chemoembolization. Cardiovasc Interv Radiol. 2006;29(1):39–48.
Moustafa AS, Abdel Aal AK, Ertel N, et al. Chemoembolization of hepatocellular carcinoma with extrahepatic collateral blood supply: anatomic and technical considerations. Radiographics. 2017;37(3):963–77.
Park SI, Lee DY, Won JY, et al. Extrahepatic collateral supply of hepatocellular carcinoma by the intercostal arteries. J Vasc Interv Radiol. 2003;14(4):461–8.
Llovet JM. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol. 2005;40(3):225–35.
Lau K, Wong WW, Chan JK, et al. Emergency transcatheter embolization of ruptured hepatocellular carcinomas with tortuous conventional or aberrant hepatic vascular anatomy, or parasitic supply. Australas Radiol. 2007;51(2):190–5.
Li T, Huang XH, Lin RF, et al. The comparation of transarterial embolization, open surgery and conservative management in the treatment of ruptured hepatocellular carcinoma. J Clin Res. 2013;30(8):1639–41.
Kirikoshi H, Saito S, Yoneda M, et al. Outcomes and factors influencing survival in cirrhotic cases with spontaneous rupture of hepatocellular carcinoma: a multicenter study. BMC Gastroenterol. 2009;9:29.
Kim JY, Lee JS, Oh DH, et al. Transcatheter arterial chemoembolization confers survival benefit in patients with a spontaneously ruptured hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2012;24(6):640–5.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ (Clin Res ed). 2004;328(7454):1490.
Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester (UK): Wiley; 2008.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
Dersimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Yang Z, Han G, Wu Q, et al. Patency and clinical outcomes of transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stents versus bare stents: a meta-analysis. J Gastroenterol Hepatol. 2010;25(11):1718–25.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Chevalier TL, Scagliotti G, Natale R, et al. Efficacy of gemcitabine plus platinum chemotherapy compared with other platinum containing regimens in advanced non-small-cell lung cancer: a meta-analysis of survival outcomes. Lung Cancer. 2005;47(1):69–80.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Dai Y, Guo T, Xu JF, et al. Analysis on curative and influencing factors on prognosis of spontaneous rupture of hepatocellular carcinoma. Mod J Integr Tradit Chin West Med. 2014;23(24):2653–8.
Ji YF, Kang YM, Song JJ, et al. The diagnosis and treatment of spontaneous rupture of hepatocellular carcinoma:27 cases report. Ningxia Med J. 2011;33(8):761–2.
Jian YP. The comparative study of transarterial embolization versus surgery in the treatment of spontaneous rupture of hepatocellular carcinoma. Mod Diagn Treat. 2016;27(1):135–6.
Jin YJ, Jin JW, Park SW, et al. Survival outcome of patients with spontaneously ruptured hepatocellular carcinoma treated surgically or by transarterial embolization. World J Gastroenterol. 2013;19(28):4537–44.
Li J, Yu XF, Bao SY, et al. The efficacy comparation of three therapies in the treatment of spontaneous rupture of hepatocellular carcinoma. J Clin Surg. 2002;10(3):174–5.
Lin HM, Lei LM, Zhu J, et al. Risk factor analysis of perioperative mortality after ruptured bleeding in hepatocellular carcinoma. World J Gastroenterol. 2014;20(40):14921–6.
Lou C, Wang YJ, Nie FH, et al. Clinical analysis of spontaneous rupture and bleeding of primary cancer in 26 cases. J Hepato Pancreato Biliary Surg. 2006;18(6):359–63.
Luo XP, Miu JQ, Huang HR, et al. The curative effect of hemorrhage due to spontaneous rupture in hepatocellular carcinoma by different methods. Chin J Prim. 2006;13(10):1603–4.
Meng XM. The efficacy of TAE in the management of hemorrhage caused by spontaneous rupture in hepatocellular carcinoma. Shandong Med. 2009;49(50):59–60.
Pan JG. The efficacy of transarterial embolization versus surgery in the treatment of spontaneous rupture and bleeding of hepatocellular carcinoma. Heilongjiang Med Pharm. 2017;40(2):120–1.
Shang LM, Zhu GZ, Peng MH, et al. The clinical experience of spontaneous rupture and bleeding of hepatocellular carcinoma, 82 cases report. Guangxi Med J. 2013;35(10):1380–4.
Shen SQ, Yang YF, Ge NJ, et al. Evaluation of interventional and surgical treatments for the hemorrhage of ruptured hepatocellular carcinoma. J Interv Radiol. 2010;19(7):544–6.
Wang JY, Liang JL, Hao DS, et al. Emergent hepatectomy and transcatheter arterial embolization for spontaneous rupture of primary hepatocellular carcinoma. Clin Med China. 2009;25(11):1185–7.
Xie FW, Huang JY, Chen J. Emergent hepatectomy and transcatheter arterial embolization for spontaneous rupture of primary hepatocellular carcinoma. Haerbin Med. 2016;36(1):19–211.
Yang HT, Chen KF, Wei YG, et al. Treatment of spontaneous ruptured hepatocellular carcinoma: a single-center study. Pak J Med Sci. 2014;30(3):472–6.
Yang YF, Cheng HY, Xu AM, et al. Tanscatheter embolization for hemorrhage due to spontaneous rupture in hepatocellular carcinoma. Chin J Oncol. 2002;24(3):285–7.
Zhong F, Cheng XS, He K, et al. Treatment outcomes of spontaneous rupture of hepatocellular carcinoma with hemorrhagic shock: a multicenter study. Springer Plus. 2016;5:1101.
Zhou YQ, Liu YG. Clinical treatment of 92 cases of spontaneous rupture and bleeding of hepatocellular carcinoma. J Mod Med Health. 2015;31(19):2952–4.
Liu C, Ngan H, Lo C, et al. Ruptured hepatocellular carcinoma as a complication of transarterial oily chemoembolization. Br J Surg. 1998;85(4):512–4.
Okezie O, Deangelis G. Spontaneous rupture of hepatoma: a misdiagnosed surgical emergency. Ann Surg. 1974;179(2):133–5.
Zhu LX, Meng XL, Fan ST. Elasticity of small artery in patient with spontaneous rupture of hepatocellular carcinoma. Hepatol Res. 2004;29(1):13–7.
Moris D, Chakedis J, Sun SH, et al. Management, outcomes, and prognostic factors of ruptured hepatocellular carcinoma: a systematic review. J Surg Oncol. 2018;117(3):341–53.
Hsueh KC, Fan HL, Chen TW, et al. Management of spontaneously ruptured hepatocellular carcinoma and hemoperitoneum manifested as acute abdomen in the emergency room. World J Surg. 2012;36(11):2670–76.
Zhu Q, Li J, Yan JJ, et al. Predictors and clinical outcomes for spontaneous rupture of hepatocellular carcinoma. World J Gastroenterol. 2012;18(48):7302–7.
Facciorusso A, Bellanti F, Villani R, et al. Transarterial chemoembolization vs bland embolization in hepatocellular carcinoma: A meta-analysis of randomized trials. United Eur Gastroenterol J. 2017;5(4):511–8.
Marelli L, Stigliano R, Triantos C, et al. Transarterial therapy for hepatocellular carcinoma: which technique is more effective?. A systematic review of cohort and randomized studies. Cardio Vasc Interv Radiol. 2007;30(1):6–25.
Xie ZB, Ma L, Wang XB, et al. Transarterial embolization with or without chemotherapy for advanced hepatocellular carcinoma: a systematic review. Tumor Biol. 2014;35(9):8451–9.
Zheng RS, Sun KX, Zhang SW, et al. Report of cancer epidemiology in china, 2015. Chin J Oncol. 2019;41(1):19–28.
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, X., Chen, C., Liu, Q. et al. A Meta-analysis of TAE/TACE Versus Emergency Surgery in the Treatment of Ruptured HCC. Cardiovasc Intervent Radiol 43, 1263–1276 (2020). https://doi.org/10.1007/s00270-020-02514-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02514-5