Abstract
Objective
The aim of this study is to investigate the potential association of neutrophil–lymphocyte ratio (NLR) between primary patency of percutaneous transluminal angioplasty (PTA) in hemodialysis arteriovenous fistula stenosis and type (Conventional and Drug-Eluting) of balloons used in PTA.
Material-Method
This retrospective study consists of 78 patients with significant arteriovenous fistulas stenosis who were treated with PTA by using Drug-Eluting Balloon (DEB) (n = 29) or Conventional Balloon (CB) (n = 49). NLR was calculated from preinterventional blood samples. All patients were classified into two groups. Group A; primary patency <12 months (43/78), Group B; primary patency ≥12 months (35/78). Cox regression analysis and Kaplan–Meier method were used to determine respectively independent factors affecting the primary patency and to compare the primary patency for the two balloon types.
Results
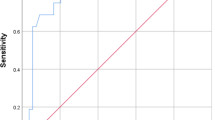
NLR ratio and balloon type of the two groups were significantly different (p = 0.002, p = 0.010). The cut-off value of NLR was 3.18 for determination of primary patency, with sensitivity of 81.4 % and specificity of 51.4 %. Primary patency rates between PTA with DEB and CB displayed statistically significant differences (p < 0.05). The cut-off value was 3.28 for determination of 12-month primary patency with the conventional balloon group; sensitivity was 81.8 % and specificity was 81.3 %. There was no statistical relation between NLR levels and the drug-eluting balloon group in 12-month primary patency (p = 0.927).
Conclusion
Increased level of NLR may be a risk factor in the development of early AVF restenosis after successful PTA. Preferring Drug-Eluting Balloon at an increased level of NLR can be beneficial to prolong patency.




Similar content being viewed by others
References
Kazemzadeh GH, Modaghegh MHS, Ravari H, Daliri M, Hoseini L, Nataghi M. Primary patency rate of native AV fistula: long term follow up. Int J Clin Exp Med. 2012;5:173–8.
III. NKF-K/DOQI Clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis. 2001; 37:S137–81.
Allon M, Robbin ML. Increasing arteriovenous fistulas in hemodialysis patients: problems and solutions. Kidney Int. 2002;62:1109–24.
Juncos JP, Grande JP, Kang L, et al. MCP-1 contributes to arteriovenous fistula failure. J Am Soc Nephrol. 2011;22(1):43–8.
Schepers A, Eefting D, Bonta PI, et al. Anti-MCP-1 gene therapy inhibits vascular smooth muscle cells proliferation and attenuates vein graft thickening both in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2006;26:2063–9.
Marrone D, Pertosa G, Simone S, et al. Local activation of interleukin 6 signaling is associated with arteriovenous fistula stenosis in hemodialysis patients. Am J Kidney Dis. 2007;49(5):664–73.
Roy-Chaudhury P, Khan R, Campos B, et al. Pathogenetic role for early focal macrophage infiltration in a pig model of arteriovenous fistula (AVF) stenosis. J Vasc Access. 2014;15(1):25–8.
Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138–50.
Chang CJ, Ko PJ, Hsu LA, et al. Highly increased cell proliferation activity in the restenotic hemodialysis vascular access after percutaneous transluminal angioplasty: implication in prevention of restenosis. Am J Kidney Dis. 2004;43:74–84.
Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992;42:1390–7.
Lee T, Ullah A, Allon M, et al. Decreased cumulative access survival in arteriovenous fistulas requiring interventions to promote maturation. Clin J Am Soc Nephrol. 2011;6:575–81.
Portugaller RH, Kalmar PI, Deutschmann H. The eternal tale of dialysis access vessels and restenosis: are drug-eluting balloons the solution? J Vasc Access. 2014;15(6):439–47.
Kitrou P, Spiliopoulos S, Katsanos K, Papachristou E, Siablis Karnabatidis D. Paclitaxel-coated balloon angioplasty versus plain balloon angioplasty for dysfunctional arteriovenous fistulae: 1 year results of a prospective randomized controlled trial. J Vasc Interv Radiol. 2015;26:348–54.
Patanè D, Giuffrida S, Morale W, et al. Drug-eluting balloon for the treatment of failing hemodialytic radiocephalic arteriovenous fistulas: our experience in the treatment of juxta-anastomotic stenoses. J Vasc Access. 2014;15(5):338–43.
Campos RP. Do Nascimento MM, Chula DC, Do Nascimento DE, Riella MC. Stenosis in hemodialysis arteriovenous fistula: evaluation and treatment. Hemodial Int. 2006;10:152–61.
Hayashi R, Huang E, Nissenson AR. Vascular access for hemodialysis Nat Clin Pract Nephrol. 2006;2(9):504–13.
Stolic R. Most important chronic complications of arteriovenous fistulas for hemodialysis. Med Princ Pract. 2013;22(3):220–8.
Roy-Chaudhury P, Kelly BS, Miller MA, et al. Venous neointimal hyperplasia in polytetrafluoroethylene dialysis grafts. Kidney Int. 2001;59:2325–34.
Joviliano EE, Piccinato CE, Joviliano RD, Moriya T, Evora PRB. Inflammatory markers and restenosis in peripheral percutaneous angioplasty with intravascular stenting: current concepts. Ann Vasc Surg. 2011;25:846–55.
Rectenwald JE, Moldawer LL, Huber TS, et al. Direct evidence for cytokine involvment in neointimal hyperplasia. Circulation. 2000;3:1697–702.
Exner M, Schillinger M, Minar E, et al. Interleukin 6 genotype and restenosis after balloon angioplasty: initial observation. Radiology. 2004;231:839–44.
Yilmaz H, Bozkurt A, Cakmak M, et al. Relationship between late arteriovenous fistula (AVF) stenosis and neutrophil-lymphocyte ratio (NLR) in chronic hemodialysis patients. Ren Fail. 2014;36(9):1390–4.
Shimazawa M, Watanabe S, Kondo K, Hara H, Nakashima M, Umemura K. Neutrophil accumulation promotes intimal hyperplasia after photochemically induced arterial injury in mice. Eur J Pharmacol. 2005;520:156–63.
Turmel-Rodrigues L, Boutin JM, Camiade C, Brillet G, Fodil-Chérif M, Mouton A. Percutaneous dilation of the radial artery in nonmaturing autogenous radial-cephalic fistulas for haemodialysis. Nephrol Dial Transplant. 2009;24:3782–8.
Mantha M, Killen JP, Baer R, Moffat J. Percutaneous maintenance and salvage of dysfunctional arteriovenous fistulae and grafts by nephrologists in Australia. Nephrology. 2011;16:46–52.
Heye S, Maleux G, Vaninbroukx J, Claes K, Kuypers D, Oyen R. Factors influencing technical success and outcome of percutaneous balloon angioplasty in de novo native hemodialysis arteriovenous fistulas. Eur J Radiol. 2012;81:2298–303.
Romann A, Beaulieu MC, Rhéaume P, Clement J, Sidhu R, Kiaii M. Risk factors associated with arteriovenous fistula failure after first radiologic intervention. J Vasc Access. 2016;17(2):167–74.
Axel DI, Kunert W, Goeggelmann C, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96:636–45.
Micari A, Vadala G, Castriota F, et al. 1-year results of Paclitaxel-coated balloons for long femoropopliteal artery disease: evidence from the SFA-long study. JACC Cardiovasc Interv. 2016;9(9):950–6.
Werk M, Albrecht T, Meyer DR, et al. Paclitaxel-coated balloons reduce restenosis after femoro-popliteal angioplasty: evidence from the randomized PACIFIER trial. Circ Cardiovasc Interv. 2012;5:831–40.
Scheinert D, Duda S, Zeller T, et al. TheLEVANT I (Lutonix paclitaxel-coated balloon for the prevention of femoropopliteal restenosis) trial for femoropopliteal revascularization: first-inhuman randomized trial of low-dose drug-coated balloon versus uncoated balloon angioplasty. J Am Coll Cardiol Intv. 2014;7:10–9.
Baerlocher MO, Kennedy SA, Rajebi MR, Baerlocher FJ, et al. Meta-analysis of drug-eluting balloon angioplasty and drug-eluting stent placement for infrainguinal peripheralarterial disease. J Vasc Interv Radiol. 2015;26(4):459–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this retrospective type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Çildağ, M.B., Çildağ, S. & Köseoğlu, Ö.F.K. The Relationship Between Neutrophil–Lymphocyte Ratio and Primary Patency of Percutaneous Transluminal Angioplasty in Hemodialysis Arteriovenous Fistula Stenosis When Using Conventional and Drug-Eluting Balloons. Cardiovasc Intervent Radiol 39, 1702–1707 (2016). https://doi.org/10.1007/s00270-016-1442-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-016-1442-y