Abstract
Background
The value of the neutrophil–lymphocyte ratio (NLR) along with the severity of mitral stenosis (MS) in predicting the outcome of percutaneous balloon mitral commissurotomy (PBMC) has not been studied.
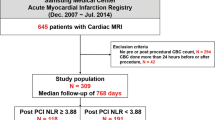
Patients and methods
Patients with severe MS undergoing PBMC between 2013 and 2014 in a university hospital were prospectively enrolled. Complete blood cell count was obtained upon admission and NLRs were calculated. The correlations between NLR with immediate PBMC success and restenosis in 1 year were evaluated.
Results
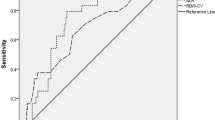
In all, 102 patients (80 women) with a mean age of 44.5 ± 13.1 years were enrolled in the study. NLR on admission was 2.6 ± 0.8 and mitral valve area (MVA) was 0.89 ± 0.18 cm2. Patients with a lower MVA at baseline had a higher NLR (p = 0.016). The rate of immediate success was 63 % for PBMC. There was no difference in NLR between patients with regard to early and late failures, as well as those who developed restenosis of the valve. Smaller valve area and the rate of valvular dilatation during PBMC were the only independent factors that predicted early and late failure, respectively.
Conclusion
NLR at the time of treatment was not useful in predicting procedural outcome or restenosis during follow-up of patients undergoing PBMC.
Zusammenfassung
Hintergrund
Bisher wurde die Bedeutung des Neutrophilen-Lymphozyten-Quotienten (NLQ) im Zusammenhang mit dem Schweregrad der Mitralstenose (MS) zur Vorhersage des Ergebnisses der perkutanen Ballon-Mitralkomissurotomie (PBMC) nicht untersucht.
Methoden
Patienten mit schwergradiger MS, bei denen zwischen 2013 und 2014 eine PBMC in einer Universitätsklinik erfolgte, wurden prospektiv in die Studie aufgenommen. Bei Aufnahme wurde ein großes Blutbild erstellt und der NLQ berechnet. Dann wurden die Korrelationen zwischen NLQ und unmittelbarem Erfolg der PBMC sowie einer Restenose nach einem Jahr ermittelt.
Ergebnisse
102 Patienten (davon 80 Frauen) mit einem Durchschnittsalter von 44,5 ± 13,1 Jahren wurden in die Studie eingeschlossen. Der NLQ bei Aufnahme lag bei 2,6 ± 0,8; und die Mitralöffnungsfläche (MVA) betrug 0,89 ± 0,18 cm2. Patienten mit niedriger MVA zu Beginn der Studie wiesen einen höheren NLQ auf (p = 0,016). Die unmittelbare Erfolgsrate betrug für die PBMC 63 %. Es gab keinen Unterschied beim NLQ zwischen den Patienten mit Früh- und Spätversagen der Therapie sowie denjenigen, bei denen eine Restenose der Klappe auftrat. Eine kleinere Klappenöffnungsfläche und die Rate der valvulären Dilatation während der PBMC waren die einzigen unabhängigen Faktoren, die sich als Prädiktoren für ein Früh- bzw. Spätversagen dieses Verfahrens eigneten.
Schlussfolgerung
Der NLQ zum Zeitpunkt der Therapie eignete sich nicht zur Vorhersage des Therapieergebnisses oder einer Restenose im Verlauf der Nachbeobachtung bei Patienten mit PBMC.
Similar content being viewed by others
References
Pourafkari L, Ghaffari S, Bancroft GR, Tajlil A, Nader ND (2015) Factors associated with atrial fibrillation in rheumatic mitral stenosis. Asian Cardiovasc Thorac Ann 23(1):17–23. doi:10.1177/0218492314530134
Carabello BA (2005) Modern management of mitral stenosis. Circulation 112(3):432–437. doi:10.1161/CIRCULATIONAHA.104.532498
Pourafkari L, Seyedhosseini S, Kazemi B, Esmaili H, Aslanabadi N (2014) Changes in serum NT-pro BNP and left atrial BNP levels after Percutaneous Transvenous mitral Commissurotomy in sinus rhythm versus atrial Firilation. J Cardiovasc Thorac Res 6(3):175–179. doi:10.15171/jcvtr.2014.007
Bhat T, Teli S, Rijal J, Bhat H, Raza M, Khoueiry G, Meghani M, Akhtar M, Costantino T (2013) Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther 11(1):55–59. doi:10.1586/erc.12.159
Aydinli B, Demir A, Guclu CY, Bolukbasi D, Unal EU, Koculu R, Selcuk G (2016) Hematological predictors and clinical outcomes in cardiac surgery. J Anesth. doi:10.1007/s00540-016-2197-y
Dentali F, Conte G, Guasti L (2016) Neutrophil-to-lymphocyte ratio: a new prognostic factor even in patients with heart failure. Pol Arch Med Wewn 126(3):116–117. doi:10.20452/pamw.3331
Ghaffari S, Nadiri M, Pourafkari L, Sepehrvand N, Movasagpoor A, Rahmatvand N, Rezazadeh Saatloo M, Ahmadi M, Nader ND (2014) The predictive value of total neutrophil count and neutrophil/lymphocyte ratio in predicting in-hospital mortality and complications after STEMI. J Cardiovasc Thorac Res 6(1):35–41. doi:10.5681/jcvtr.2014.007
Kaya A, Kurt M, Tanboga IH, Isik T, Gunaydin ZY, Kaya Y, Topcu S, Sevimli S (2014) Relation of neutrophil to lymphocyte ratio with the presence and severity of stable coronary artery disease. Clin Appl Thromb Hemost 20(5):473–477. doi:10.1177/1076029612473517
Akboga MK, Akyel A, Sahinarslan A, Yayla C, Alsancak Y, Gokalp G, Nurkoc S, Abaci A (2015) Neutrophil-to-lymphocyte ratio is increased in patients with rheumatic mitral valve stenosis? Anatol J Cardiol 15(5):380–384. doi:10.5152/akd.2014.5399
Polat N, Yildiz A, Yuksel M, Bilik MZ, Aydin M, Acet H, Akil MA, Oylumlu M, Kaya H, Ertas F, Cil H (2014) Association of neutrophil-lymphocyte ratio with the presence and severity of rheumatic mitral valve stenosis. Clin Appl Thromb Hemost 20(8):793–798. doi:10.1177/1076029613514131
Krasuski RA, Bush A, Kay JE, Mayes CE Jr., Wang A, Fleming J, Pierce C, Kisslo KB, Harrison JK, Bashore TM (2003) C‑reactive protein elevation independently influences the procedural success of percutaneous balloon mitral valve commissurotomy. Am Heart J 146(6):1099–1104. doi:10.1016/S0002-8703(03)00506-4
Ostovan M, Aslani A, Abounajmi S, Razazi V (2014) Mitral valve restenosis after percutaneous transmitral valvuloplasty, role of continuous inflammation. J Cardiovasc Thorac Res 6(3):191–195. doi:10.15171/jcvtr.2014.010
Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF (1988) Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 60(4):299–308
Inoue K, Owaki T, Nakamura T, Kitamura F, Miyamoto N (1984) Clinical application of transvenous mitral commissurotomy by a new balloon catheter. J Thorac Cardiovasc Surg 87(3):394–402
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Creager MA, Curtis LH, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Stevenson WG, Yancy CW, American College of Cardiology/American Heart Association (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 148(1):e1–e132. doi:10.1016/j.jtcvs.2014.05.014
Badoz M, Arrigo M, Iung B, Amioglu G, Yilmaz MB, Meneveau N, Sadoune M, Brunette A, Mebazaa A, Seronde MF (2016) Role of cardiovascular biomarkers for the assessment of mitral stenosis and its complications. Eur J Intern Med. doi:10.1016/j.ejim.2016.05.008
Yetkin E, Erbay AR, Ileri M, Turhan H, Balci M, Cehreli S, Yetkin G, Demirkan D (2001) Levels of circulating adhesion molecules in rheumatic mitral stenosis. Am J Cardiol 88(10):1209–1211
Harikrishnan S, Rajeev E, Tharakan JA, Thomas T, Ajith K, Sivasankaran S, Krishnamoorthy KM, Santhosh D, Krishnakumar N, Namboodiri KK (2006) Acute phase reactants predict mitral regurgitation following mitral valvuloplasty. Int J Cardiol 112(1):127–129. doi:10.1016/j.ijcard.2005.11.031
Xu T, Zhang L, Geng ZH, Wang HB, Wang JT, Chen M, Geng JG (2007) P‑selectin cross-links PSGL-1 and enhances neutrophil adhesion to fibrinogen and ICAM-1 in a Src kinase-dependent, but GPCR-independent mechanism. Cell Adh Migr 1(3):115–123
Wang S, Zhang Z, Fang F, Gao X, Sun W, Liu H (2011) The neutrophil/lymphocyte ratio is an independent prognostic indicator in patients with bone metastasis. Oncol Lett 2(4):735–740. doi:10.3892/ol.2011.304
Azab B, Camacho-Rivera M, Taioli E (2014) Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLOS ONE 9(11):e112361. doi:10.1371/journal.pone.0112361
Sung HH, Jeon HG, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM (2015) Clinical significance of prognosis using the neutrophil-lymphocyte ratio and erythrocyte sedimentation rate in patients undergoing radical nephroureterectomy for upper urinary tract urothelial carcinoma. BJU Int 115(4):587–594. doi:10.1111/bju.12846
Baysal E, Burak C, Cay S, Aksu T, Altintas B, Yaylak B, Sevuk U, Bilge O (2015) The neutrophil to lymphocyte ratio is associated with severity of rheumatic mitral valve stenosis. J Blood Med 6:151–156. doi:10.2147/JBM.S82423
Ozturk D, Erturk M, Celik O, Ozyilmaz S, Akturk F, Cakmak HA, Aksu H, Pusuroglu H, Yalcin AA, Uslu N (2014) The role of the neutrophil/lymphocyte ratio in patients with rheumatic mitral stenosis as an indicator of spontaneous echocardiographic contrast. Kardiol Pol 72(10):969–976. doi:10.5603/KP.a2014.0093
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Separham, L. Pourafkari, H. Boudagh, S. Ghaffari, N. Aslanabadi, and N.D. Nader declare that they have no competing interest.
The research protocol was approved by the local institutional review board and was conducted in accordance with the Helsinki Declaration.
Rights and permissions
About this article
Cite this article
Separham, A., Pourafkari, L., Bodagh, H. et al. Predicting outcome after percutaneous balloon mitral commissurotomy. Herz 42, 509–514 (2017). https://doi.org/10.1007/s00059-016-4488-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4488-3
Keywords
- Percutaneous coronary intervention
- Balloon valvuloplasty
- Mitral valve stenosis
- Rheumatic heart disease
- Outcome