Abstract
Introduction
Nonoperative management (NOM) has become the treatment of choice for hemodynamically stable patients with blunt splenic injury. Results of outcome after NOM are predominantly based on large-volume studies from level 1 trauma centers in the United States. This study was designed to assess the results of NOM in a relatively low-volume Dutch level 1 trauma center.
Methods
An analysis of a prospective trauma registry was performed for a 6-year period before (period 1) and after the introduction and implementation of splenic artery embolization (SAE) (period 2). Primary outcome was the failure rate of initial treatment.
Results
A total of 151 patients were reviewed. An increased use of SAE and a reduction of splenic operations during the second period was observed. Compared with period 1, the failure rate after observation in period 2 decreased from 25% to 10%. The failure rate after SAE in period 2 was 18%. The splenic salvage rate (SSR) after observation increased from 79% in the first period to 100% in the second period. During the second period, all patients with failure after observation were successfully treated with SAE. The SSR after SAE in periods 1 and 2 was respectively 100% and 86%.
Conclusions
SAE of patients with blunt splenic injuries is associated with a reduction in splenic operations. The failure and splenic salvage rates in this current study were comparable with the results from large-volume studies of level 1 trauma centers. Nonoperative management also is feasible in a relatively low-volume level 1 trauma center outside the United States.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma is one of the leading causes of death in people younger than age 40 years and, therefore, is an important problem in general healthcare [1–3]. The spleen is affected in 32% of patients with traumatic abdominal injuries [4].
Management of splenic injuries has changed considerably during the past 20 years. Traditionally, a laparotomy and splenectomy was performed for splenic injuries. Due to its high success rate, nonoperative management (NOM) has evolved to be the standard of care in hemodynamically stable patients.
NOM can be divided in observation or splenic artery embolization (SAE). SAE has played an increasing role in this nonoperative approach. Many reviews supported the use of SAE as an adjunct to observation. SAE can increase the success rate of NOM by stopping ongoing bleeding and by preventing delayed rupture of the spleen. Recent studies advocate the use of angiography and embolization in the presence of the following CT findings: contrast extravasation, pseudoaneurysm or arteriovenous fistula, large hemoperitoneum, and a high grade of injury (grade III–V) [5–15]. Results of outcome after NOM in blunt splenic trauma are predominantly based on large-volume studies from level 1 trauma centers in the United States [5–9, 13, 16, 17]. Trauma patient volumes in European centers often are considerably lower than in the United States. Therefore, it is questionable whether these results can be translated to centers with lower volumes of patients with blunt splenic injuries. The purpose of this study was to assess the influence of SAE on the failure of NOM and the splenic salvage rate in a relatively low-volume level 1 Dutch trauma center.
Methods
Data Collection
Patients with blunt splenic injuries treated in the Academic Medical Center (AMC) between January 1997 and June 2008 were identified from the prospectively collected data in the hospital’s trauma registry. Children younger than age 17 years and patients who died within 24 h after trauma were excluded. The AMC is a designated Dutch level 1 trauma center with 32,000 emergency department visits and 700 trauma team notifications per year. Annually, approximately 200–225 multitrauma patients are treated.
Patient demographics, including age, gender, trauma mechanism, Injury Severity Score (ISS), Glasgow Coma Scale (GCS), and associated injuries, were extracted from the computerized medical record. Furthermore, initial treatment and their indications, transfusion requirements, morbidity, mortality, and intensive care unit and overall hospital length of stay were registered.
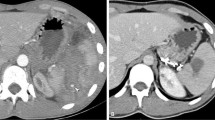
One senior trauma radiologist reevaluated all admission abdominal CT scans and classified the splenic injuries according to the American Association for the Surgery of Trauma (AAST) [18]. Grades I and II were classified as low grade and grades III–V as high grade. Data on the presence of vascular injury (contrast extravasation, pseudoaneurysm, and arteriovenous fistula), hemoperitoneum, and the extension of hemoperitoneum also were registered. Minimal hemoperitoneum was defined as intra-abdominal blood located only in the perisplenic recess. Significant hemoperitoneum was defined as intra-abdominal blood located in areas other than the perisplenic recess.
Study Periods
Two time periods were defined. At the end of the first period (1997–2002), angiography and embolization for trauma patients was introduced but not used routinely. This period was compared with a second period (2003–2008) when SAE was used routinely.
Imaging and Treatment Protocols
During both periods, hemodynamically unstable patients who were not responding to fluid resuscitation were treated primarily operatively. During period 1, the protocol dictated surgical exploration in patients with high-grade injuries (grades 3–4), independent of the hemodynamic status of the patients. Operative treatment began with four-quadrant packing before structural inspection of the abdomen. Once the spleen has been mobilized, a decision was made whether a splenectomy or a splenic salvage procedure (mesh splenorrhaphy, partial resection, adhesive, and/or coagulation techniques) was performed.
During period 1, NOM was performed in patients with low-grade (grades 1–2) injuries who were hemodynamically stable. During period 2, NOM was performed in all hemodynamically stable patients or transient responders. NOM involves admission to a unit with monitoring of vital signs, strict bed rest, frequent monitoring of red blood cell count, and serial abdominal examinations. During the second period, SAE was routinely performed 24 h/7 days per week by an experienced interventional radiologist if signs of active bleeding (contrast blush or cutoff), pseudoaneurysm, or arteriovenous fistula were detected on CT scan. Splenic arterial catheterization was performed by using the common femoral artery access. After puncture of the artery a 5-Fr sheath was introduced.
Diagnostic series of the splenic artery were obtained using a 4- or 5-Fr catheter or celiac catheter. For selective catheterization of splenic artery branches coaxial microcatheters and microguidewires were required.
Proximal embolization was performed if there was a diffuse bleeding of the spleen, if there were multiple focal bleeding vessels in the spleen, when there was time-pressure as a result of the hemodynamic situation of the patient, or when tortuosity of the splenic artery prevented selective distal embolization. Selective distal embolization was reserved for patients who had one or only a few focal bleeding vessels in the spleen and in whom the anatomy and hemodynamic situation allowed employment of this. Follow-up ultrasounds or CT scans were not routinely performed.
Study Endpoints
Primary outcome was the failure rate of initial treatment. Failure was defined as clinical (hemodynamically unstable or drop in hemoglobin/hematocrit) and radiological (a blush or significant increase of hemoperitoneum on repeat CT scan) signs of a rebleeding requiring operative or radiological (re-)interventions. The failure rate and the splenic salvage rate in both periods were compared to identify the impact of SAE. Splenic salvage was considered as patient discharge with the spleen in situ.
Secondary outcome measures were length of intensive care unit and total hospital stay, transfusion requirements during the first 24 h, and mortality rate. Mortality was coded as due to splenic injury complications or other causes.
Statistical Analysis
All statistical analyses were performed by using SPSS version 17 (SPSS, Inc., Chicago, IL). Categorical variables were calculated as percentages and compared by using Chi-square analyses or Fisher’s exact tests when appropriate. All continuous variables are presented as median with interquartile ranges (p25–p75) and were compared by using the Mann–Whitney U test. A value of P = 0.05 was considered statistically significant.
Results
A total of 151 patients with blunt splenic injury were identified. Twenty-nine patients were excluded: 6 patients died within 24 h of admission and 23 patients were children. Of the 122 included patients, the majority were young men with a mean age of 29 (range, 23–46) years. As demonstrated in Table 1, both periods were comparable for age, gender, and ISS and AAST injury grade.
In Table 1, the initial treatment is shown for both periods. The number of patients treated with observation was similar. During period 2, a significant increase of SAEs was observed: 4% during the first period versus 34% during the second period (P < 0.001). This increase correlated with the statistically significant reduction of splenic operations (46% vs. 19%; P < 0.001).
Most of the patients who underwent SAE (13/24) did so as initial treatment. In 10% of the patients, injuries to other organs were embolized during the same angiography session. Table 2 shows the failure rate after initial treatment in both periods. The overall failure rate for observation and SAE was both 17%. During the second period, the failure rate after observation was reduced from 25% to 10%. The failure rate after SAE in period 2 was 18%; SAE failed in 4 of the 22 patients due to rebleeding of the spleen.
Table 3 shows the injuries divided into low and high AAST grades per period and compared for primary treatment and outcomes. Most of the patients who failed initial treatment had high grade of injury. Twenty-five percent of the patients with high-grade injury failed initial SAE, whereas no failure of SAE was observed in patients with low-grade injury. The characteristics of the patients with failure of initial treatment are depicted in Table 4. In almost all of these patients, the reevaluated CT scan showed a contrast blush and/or a significant hemoperitoneum. Three of the four patients who failed SAE during the second period had a grade 5 injury combined with a blush and a significant hemoperitoneum on the CT scan.
The overall splenic salvage rate was 89%. Compared with period 1, the SSR after observation in period 2 increased from 79% to 100%. During the first period, six of the seven patients who failed observation underwent a splenectomy. In one patient, splenic-preserving therapy during laparotomy was performed. In the second period, all patients with failure (n = 3) after observation were successfully treated with SAE.
The splenic salvage rate after SAE in periods 1 and 2 was respectively 100% and 86%. One of the four patients with failure after initial distal selective SAE successfully underwent proximal reembolization during the second period. The other three patients underwent a splenectomy.
The median time from initial treatment to failure was 2 (range, 1–23) days. In two patients, the rebleeding occurred after being discharged from hospital. One patient with a grade 5 splenic injury, initially treated with embolization, had severe neurological impairment due to rebleeding and died 3 months later.
The mortality rate and intensive care unit and total length of stay were not different for both periods. The transfusion requirement was significantly (P < 0.01) lower during the second period (Table 1) in both nonoperative management and operative treatment.
Discussion
The primary outcome of this study was to assess the influence of SAE on the failure and splenic salvage rate. Consistent with the literature, we showed a change from operative to nonoperative management for patients with blunt splenic injury. The first successful use of SAE for a splenic injury was described by Sclafani et al [19]. In our level 1 trauma center, SAE was introduced in 1998 and since 2002 has been used routinely for hemodynamically stable patients who are considered to be at high risk of failure. In the first period we evaluated, a splenic operation was performed in almost half of the patients. In the second period, the rate of splenic operations was reduced, whereas the use of SAE increased over time.
In this study, the failure rate after observation was reduced in the second period. More frequent use of CT scan and the improvement of the quality of the CT scan could be an explanation for the clear trend of decreasing failure rate after observation in the second period. This improved CT technique may enable better patient selection for observation or SAE.
We reported a failure rate of 18% after SAE in the second period. It is not fair to compare the failure rates of SAE between the two periods because only two patients in the first period were treated with SAE. This reported failure rate is comparable with the results of a large, multicenter trial in which splenic embolization was used in 140 patients. This study reported an overall splenic salvage rate of 87% and 83% for grade 4 and 5 injuries, which were successfully managed with embolization [7].
All patients who failed initial SAE had a high grade of injury. Strikingly, in our study three of the four patients who failed SAE in the second period had a grade 5 injury combined with a vascular blush and a significant hemoperitoneum on the CT scan, suggesting that the optimal patient selection for SAE is still a topic for further research. Some authors recommend a low threshold to operate if there is evidence of a grade 3–5 injury combined with a significant hemoperitoneum [13, 20]. Furthermore, with respect to this fact one patient who failed SAE became hemodynamically unstable due to rebleeding and consequently developed severe neurological damage and died 3 months later.
Failure was observed after proximal as well as distal selective embolization (Table 4). The current literature provides little evidence of whether proximal SAE or distal selective embolization is a better treatment. Although no prospective studies that compare the results of proximal or selective embolization are described, the use of proximal SAE seems to be faster, associated with a lower failure rate of NOM, and a decreased incidence of splenic abscess or infarction [13, 21, 22]. A disadvantage of proximal SAE could be the fact that in case of rebleeding, more selective embolization is difficult due to the inaccessibility of the splenic artery.
The overall splenic savage rate was 89%. During period 2, the SSR after observation was increased, due to the successful secondary treatment with SAE of patients who failed initial treatment. In the SAE group, one patient with rebleeding could successfully be treated with subsequent proximal embolization. Despite rebleeding, SAE is a valuable minimally invasive technique to control bleeding. Historically, every patient with rebleeding was treated surgically. Currently, a second attempt of SAE can be considered, which further can increase the nonoperative splenic salvage rate [5, 7, 16].
Results of outcome after NOM in blunt splenic trauma are predominantly based on large-volume studies from level 1 trauma centers in the United States. Despite the lower patient volume in this study, the failure rate and SSR are comparable with the results of these large studies. In these studies, the SSR of nonoperative management with the use of splenic embolization ranges from 86% to 100%, with most studies reporting success rates >90% [5–9, 13, 16, 17].
The second goal of this study was to assess the effects on clinical outcome. More frequent use of SAE and consequently lesser laparotomies have the theoretical potential of decreasing length of hospital stay and blood transfusion requirements. However, in this study the ICU and total length of stay were comparable in both periods. The transfusion requirement was significantly lower in the second period. The more frequent use of SAE could not alone explain the lower transfusion rate, whereas patients with operative treatment also received fewer transfusions during period 2. Part of the explanation possibly could be the advancements in the areas of critical care and transfusion and resuscitation policies.
As with any retrospective study, our analysis has several limitations. Selection bias might have played a role. Despite protocols for diagnostics and treatment, in practice the choice of therapy was based on the clinical judgement of the attending trauma surgeon and (interventional) radiologist. The specific indication for the chosen therapy could not always be assessed from the trauma registry or electronic medical record. Furthermore, advancements in ICU treatment, transfusion protocols, improved quality of the CT scan, and SAE between the two time periods investigated could cause a bias in the results. This study did not evaluate isolated splenic trauma as in most of the published series. As a consequence, the mortality, morbidity, and transfusion requirement could reflect variability in recruitment, which is observed most modern countries (decrease number of severe road accidents during the last 15 years). Another limitation is the relatively small number of patients with blunt splenic injury in our hospital. This volume, however, is comparable to other level 1 trauma centers in Europe.
In conclusion, the increased use of SAE as an adjunct to NOM was associated with a statistically significant reduction of splenic operations.
The failure and splenic salvage rates in the current study were comparable with the results from large-volume studies of level 1 trauma centers in the United States. Comparable with the literature, a high failure rate was observed in patients with high-grade injuries combined with a contrast blush and a significant hemoperitoneum. Therefore, NOM with the adjunction of SAE in patients with low-grade injuries is feasible in a relatively low-volume level 1 trauma center outside the United States. However, the optimal treatment, especially in patients with high-grade injuries, is still a topic for further research.
References
Gaines BA (2009) Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma 67:S135–S139
Gopal V, Bisno AL (1977) Fulminant pneumococcal infections in ‘normal’ asplenic hosts. Arch Intern Med 137:1526–1530
Sauaia A, Moore FA, Moore EE et al (1995) Epidemiology of trauma deaths: a reassessment. J Trauma 38:185–193
Smith J, Caldwell E, D’Amours S, Jalaludin B, Sugrue M (2005) Abdominal trauma: a disease in evolution. ANZ J Surg 75:790–794
Dent D, Alsabrook G, Erickson BA et al (2004) Blunt splenic injuries: high nonoperative management rate can be achieved with selective embolization. J Trauma 56:1063–1067
Haan J, Ilahi ON, Kramer M, Scalea TM, Myers J (2003) Protocol-driven nonoperative management in patients with blunt splenic trauma and minimal associated injury decreases length of stay. J Trauma 55:317–321
Haan JM, Biffl W, Knudson MM et al (2004) Splenic embolization revisited: a multicenter review. J Trauma 56:542–547
Haan JM, Bochicchio GV, Kramer N, Scalea TM (2005) Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma 58:492–498
Liu PP, Lee WC, Cheng YF et al (2004) Use of splenic artery embolization as an adjunct to nonsurgical management of blunt splenic injury. J Trauma 56:768–772
Rajani RR, Claridge JA, Yowler CJ et al (2006) Improved outcome of adult blunt splenic injury: a cohort analysis. Surgery 140:625–631
Shanmuganathan K, Mirvis SE, Sherbourne CD, Chiu WC, Rodriguez A (1999) Hemoperitoneum as the sole indicator of abdominal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology 212:423–430
Shanmuganathan K, Mirvis SE, Boyd-Kranis R, Takada T, Scalea TM (2000) Nonsurgical management of blunt splenic injury: use of CT criteria to select patients for splenic arteriography and potential endovascular therapy. Radiology 217:75–82
Smith HE, Biffl WL, Majercik SD, Jednacz J, Lambiase R, Cioffi WG (2006) Splenic artery embolization: have we gone too far? J Trauma 61:541–544
Peitzman AB, Heil B, Rivera L et al (2000) Blunt splenic injury in adults: multi-institutional study of the eastern association for the surgery of trauma. J Trauma 49:177–187
Wei B, Hemmila MR, Arbabi S, Taheri PA, Wahl WL (2008) Angioembolization reduces operative intervention for blunt splenic injury. J Trauma 64:1472–1477
Haan JM (2007) Experience with splenic main coil embolization and significance of new or persistent pseudoaneurym: reembolize, operate, or observe. J Trauma 63(3):615–619
Hagiwara A, Yukioka T, Ohta S, Nitatori T, Matsuda H, Shimazaki S (1996) Nonsurgical management of patients with blunt splenic injury: efficacy of transcatheter arterial embolization. AJR Am J Roentgenol 167(1):159–166
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR (1995) Organ injury scaling: spleen and liver (1994 revision). J Trauma 38:323–324
Sclafani SJ (1995) Nonoperative salvage of computed tomography-diagnosed splenic injuries: utilization of angiography for triage and embolization for hemostasis. J Trauma 39:818–825 (discussion 826–827)
Duchesne JC, Simmons JD, Schmieg RE Jr, McSwain NE Jr, Bellows CF (2008) Proximal splenic angioembolization does not improve outcomes in treating blunt splenic injuries compared with splenectomy: a cohort analysis. J Trauma 65:1346–1351
Omert LA, Salyer D, Dunham CM, Porter J, Silva A, Protetch J (2001) Implications of the “contrast blush” finding on computed tomographic scan of the spleen in trauma. J Trauma 51:272–277
Killeen KL, Shanmuganathan K, Boyd-Kranis R, Scalea TM, Mirvis SE (2001) CT findings after embolization for blunt splenic trauma. J Vasc Interv Radiol 12:209–214
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van der Vlies, C.H., Hoekstra, J., Ponsen, K.J. et al. Impact of Splenic Artery Embolization on the Success Rate of Nonoperative Management for Blunt Splenic Injury. Cardiovasc Intervent Radiol 35, 76–81 (2012). https://doi.org/10.1007/s00270-011-0132-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0132-z