Abstract
Background
Preoperative inflammatory markers were shown to be associated with prognosis following surgery for hepato-pancreato-biliary cancer. Yet little evidence exists about their role in patients with colorectal liver metastases (CRLM). This study aimed to examine the association between selected preoperative inflammatory markers and outcomes of liver resection for CRLM.
Methods
Data from the Norwegian National Registry for Gastrointestinal Surgery (NORGAST) was used to capture all liver resections performed in Norway within the study period (November 2015–April 2021). Preoperative inflammatory markers were Glasgow prognostic score (GPS), modified Glasgow prognostic score (mGPS) and C-reactive protein to albumin ratio (CAR). The impact of these on postoperative outcomes, as well as on survival were studied.
Results
Liver resections for CRLM were performed in 1442 patients. Preoperative GPS ≥ 1 and mGPS ≥ 1 were present in 170 (11.8%) and 147 (10.2%) patients, respectively. Both were associated with severe complications but became non-significant in the multivariable model. GPS, mGPS, CAR were significant predictors for overall survival in the univariable analysis, but only CAR remained such in the multivariable model. When stratified by the type of surgical approach, CAR was a significant predictor for survival after open but not laparoscopic liver resections.
Conclusions
GPS, mGPS and CAR have no impact on severe complications after liver resection for CRLM. CAR outperforms GPS and mGPS in predicting overall survival in these patients, especially following open resections. The prognostic significance of CAR in CRLM should be tested against other clinical and pathology parameters relevant for prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have examined the relationship between preoperative inflammatory markers and prognosis (recurrence, survival) in patients operated for hepato-pancreato-biliary cancer [1,2,3,4]. As for patients with colorectal liver metastases (CRLM), there is a limited number of such studies most of which suffer from a relatively small sample size [5,6,7,8,9,10,11,12]. Furthermore, these reports are predominantly based on single-center experiences, which somewhat limits the generalizability of their findings.
Minimally invasive liver resections are increasingly replacing open procedures in the management of CRLM due to less postoperative morbidity, faster recovery and comparable oncologic outcomes [13,14,15,16]. At the same time, minimally invasive approach has been shown to be associated with less postoperative inflammatory response compared with open surgery, presumably due to less intraoperative trauma [17]. Thus, the role of preoperative inflammatory markers in CRLM should be considered through the prism of the surgical approach used.
The goal of this study was to examine the association between selected preoperative inflammatory markers and outcomes of liver resection for CRLM using data from a national registry. We also analyzed how the predictive markers performed in subgroups stratified by surgical approach and the extent of liver resection.
Material and Methods
Study Design
In this nationwide cohort study, prospectively collected data from the Norwegian National Registry for Gastrointestinal Surgery (NORGAST) was used. Specific information about NORGAST and centralization of the health care system in Norway has been provided elsewhere [18, 19]. This also applies to details about data collection, procedure coding and inclusion/exclusion criteria for NORGAST [18, 20, 21].
Patients with CRLM who had undergone liver resection within the study period (November 2015–April 2021) were included. The associations between preoperative inflammatory markers and postoperative outcomes, as well as survival were studied. Inflammatory markers included Glasgow prognostic score, modified Glasgow prognostic score and C-reactive protein to albumin ratio (GPS, mGPS and CAR, respectively). The last follow-up date was May 31st, 2021. Patients with incomplete information on preoperative C-reactive protein and/or albumin were excluded from the analysis as were those diagnosed with liver lesions of any histological entity other than CRLM (Fig. 1).
The manuscript was written and completed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [22]. All patients included in NORGAST have given written informed consent for storing their data in the registry. Also, NORGAST holds a data storage license from the Norwegian Data Authority. Finally, this study was approved by the Regional Ethics Committee (2021/268695).
Definitions
GPS, mGPS and CAR were estimated based upon serum C-reactive protein and albumin levels registered at the last preoperative work-up. GPS 0 denoted normal serum C-reactive protein and albumin levels, while mGPS 0 was used for normal serum C-reactive protein and any albumin levels. GPS and mGPS scored 1 in case of elevated serum C-reactive protein (>10 mg/L) and normal albumin levels. Also, GPS 1 was used for cases with normal C-reactive protein level and hypoalbuminemia (< 35 g/L). Finally, both GPS and mGPS scored 2 if elevated serum C-reactive protein level together with hypoalbuminemia were present. Given the relatively small number of patients with preoperative GPS 2 and mGPS 2, these were studied together with those having GPS 1 and mGPS 1, respectively. This allowed for balancing study groups and reducing the risk for type II error. CAR was analyzed as a continuous variable.
Liver resections were performed either open or laparoscopically. Laparoscopic liver resection was defined as a procedure performed through minimally-invasive approach where laparotomy incisions were done only for either trocar insertion or specimen extraction. Conversion to open surgery was defined as laparotomy at any time during surgery, not specifically related to the extraction of the specimen or trocar insertion. Minor and major hepatectomy included resection of <3 and ≥ 3consecutive liver segments, respectively. Postoperative complications were defined and graded based on the modified Accordion system [23]. Grade ≥ III complications were defined as severe. Postoperative mortality was defined as death within 90 days after surgery. Overall survival was defined as the time between the date of surgery and the date of death from any cause or the date of censoring.
Statistics
Parameters are presented in the form of continuous or categorical data. Normally distributed continuous data are shown as means (standard deviation), while non-normally distributed (skewed) continuous data are shown as medians (range). Student’s t-test and Mann–Whitney U test are used for normally and non-normally distributed continuous data, respectively. Categorical data are shown in frequencies (percentages) and analyzed by using the Chi-square and Fisher’s exact tests. A two-tailed p-value < 0.05 is considered statistically significant. Parameters significant in the univariable analysis are included in the multivariable binary logistic regression model with backward selection.
The impact of inflammatory markers on survival is examined by using the log-rank test and univariable Cox regression analysis. Parameters significant at p < 0.05 in the univariable analyses are entered into multivariable model to identify independent prognostic factors.
Results
A total number of 1442 patients underwent liver resection for CRLM at five university centers including 311 (21.6%) major hepatectomies. Preoperative GPS was graded as 0, 1 and 2 in 1272 (88.2%), 149 (10.3%) and 21 (1.5%) patients, respectively, while preoperative mGPS was 0, 1 and 2 in 1295 (89.8%), 126 (8.7%) and 21 (1.5%) patients, respectively. Laparoscopic procedures were performed in 720 (49.9%) patients. Severe complications occurred in 255 (17.7%) including 47 (3.3%) reoperations. Ninety-day mortality was observed in 13 (0.9%) cases.
Inflammatory Markers and Perioperative Results
There were statistically significant differences between the patients with GPS 0 and ≥1 in terms of preoperative weight loss, ECOG score, ASA score, CAR, as well as proportions of laparoscopic and major liver resections (Table 1). Differences in these parameters were also observed in patients with mGPS 0 and mGPS ≥ 1, except weight loss which was similar between the groups. The use of neoadjuvant chemotherapy was more common among the patients with mGPS ≥ 1 compared to those with mGPS 0 (52.4 vs 43.5%, p = 0.04).
Patients with severe complications had more weight loss, greater proportion of severe lung diseases and more frequent use of neoadjuvant chemotherapy (Table 2). Both GPS ≥ 1 and mGPS ≥ 1 were associated with severe complications. So were weight loss, presence of severe lung disease, neoadjuvant chemotherapy, and performing major liver resection. The latter turned out to be the only predictor for severe complications in the multivariable analysis.
Analysis of specific types of severe complications demonstrated that GPS and mGPS were associated with single-organ failure after liver resection (suppl. Table 1). However, these associations were not statistically significant in the multivariable model (suppl. table 2). Subgroup analyses in patients undergoing minor/major liver resection and open/laparoscopic surgery did not reveal any statistically significant association between the inflammatory markers and severe complications (suppl. Tables 3, 4, 5, 6).
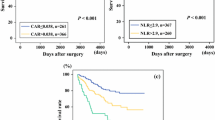
Inflammatory Markers and Survival
Median follow-up was 25 (1–67) months. Three- and 5-year survival were 66.4% and 47.9%, respectively. Both GPS 0 and mGPS 0 resulted in significantly longer survival compared with GPS ≥ 1 and mGPS ≥ 1, respectively (Fig. 2). Parameters such as age, ECOG score, ASA score, CAR and severe complications were also associated with survival in the univariable analysis (Table 3). In the multivariable model, age, ECOG ≥ 2, ASA, CAR and severe complications were the only significant prognostic factors.
Subgroup analyses were performed in patients undergoing laparoscopic and open resection for CRLM (Table 4). In the multivariable analysis, CAR was the only prognostic factor following open resections (1.41 (1.14–1.73), p = 0.001). For laparoscopic resections, ECOG ≥ 2 and severe complications were the only significant prognostic factors in the multivariable model. In patients undergoing minor hepatectomy, factors such as age, ECOG ≥ 2, ASA score, CAR and severe complications were significant for prognosis (suppl. table 4). As for major hepatectomy, the impact of CAR was marginal (1.27 (0.99–1.63), p = 0.055), while other parameters were not significant in the multivariable analysis.
Discussion
This study suggests that preoperative CAR outperforms GPS and mGPS when considering their impact on overall survival after liver resection for CRLM. To the best of our knowledge, this is the largest study assessing the prognostic role of preoperative inflammatory markers in patients operated for CRLM. Furthermore, this is the first report examining the performances of all C-reactive protein and albumin-based inflammatory markers (GPS, mGPS and CAR) in these patients. Unlike previously published reports our study includes a complete national dataset allowing for a full coverage of CRLM resections performed on a nationwide basis within the study period. Our findings do not agree with those reported by Solaini and co-workers, who found that preoperative GPS was more sensitive than CAR in predicting overall survival [8]. Nevertheless, our results are in line with those from Haruki et al. suggesting better prognostic ability for CAR compared with mGPS [6].
Our findings indicate that the prognostic role of preoperative CAR is relevant for open, but not for laparoscopic liver resections. As mentioned above, reduced systemic inflammation was observed following laparoscopic liver resection for CRLM when compared with its open counterpart [17]. Building upon these and our findings, one may assume that while the negative impact of preoperative inflammation is further aggravated by open surgery, laparoscopy may alleviate these effects, thereby providing benefits in patients with increased preoperative CAR. We also found that severe complications led to worse prognosis in patients undergoing laparoscopic surgery, but not in those undergoing open surgery. Putting this in the context of surgical technique and postoperative inflammation, one can speculate that severe complications arising after laparoscopic resections nullify or significantly diminish the inflammation-related benefits of laparoscopy, while such changes are less pronounced for open surgery. These hypotheses require further investigation focused specifically on perioperative changes in inflammatory markers, their relationship with surgical technique, complications, and prognosis.
This study also assessed the associations between the preoperative inflammatory markers and perioperative outcomes. GPS ≥ 1 but not mGPS ≥ 1 was associated with preoperative weight loss, while none of them was linked to body mass index before surgery. Preoperative weight loss was a significant predictor for severe complications in the univariable analysis although not statistically significant in the final model. These findings require further scrutiny as weight loss may indicate patient frailty and possible increased risk for postoperative complications. Both GPS ≥ 1 and mGPS ≥ 1 were associated with higher ECOG and ASA scores, as well as with performing open surgery and major hepatectomy. The last two might be surrogate markers of disease spread or greater tumor size. Unfortunately, NORGAST does not hold data for TNM-stage, so this assumption cannot be tested. At the same time, none of the preoperative inflammatory markers was associated with severe complications following surgery. Subgroup analyses in patients undergoing minor and major hepatectomy also did not reveal any association between the preoperative inflammatory markers and postoperative complications.
There are several important limitations with this study. Primarily, although data collection was conducted prospectively in the registry, the protocol for analysis was constructed after the inclusion period. Secondly, as NORGAST is designed for all types of gastro-intestinal and hepato-pancreato-biliary resections, several CRLM-specific pathology and clinical parameters were not registered. Also, molecular prognostic factors in CRLM such as RAS status, bRAF and MSI have not been a part of this registry. That somewhat limits the reliability and interpretation of prognostic factors determined in the multivariable analysis. It would be desirable to test the prognostic significance of CAR by analyzing it together with all the clinical, pathology and molecular parameters relevant for CRLM. Third, data on recurrence, its site and recurrence-free survival was not registered, so these parameters could not be studied in the context of preoperative inflammatory markers. Finally, data on some baseline characteristics were incomplete in a negligible proportion of cases (< 1%).
Conclusions
Preoperative inflammatory markers have no correlation with postoperative severe complications in patients undergoing liver resection for CRLM. Preoperative CAR outperforms GPS and mGPS in predicting overall survival following liver resection for CRLM, especially for patients undergoing open procedures. The prognostic significance of CAR needs to be tested against other clinical, pathology and molecular parameters that are relevant for prognosis.
References
Jansson H, Cornillet M, Björkström NK et al (2020) Prognostic value of preoperative inflammatory markers in resectable biliary tract cancer—validation and comparison of the Glasgow Prognostic Score and Modified Glasgow Prognostic Score in a Western cohort. Eur J Surg 46(5):804–810
Liu Z, Jin K, Guo M et al (2017) Prognostic value of the CRP/Alb ratio, a novel inflammation-based score in pancreatic cancer. Ann Surg Oncol 24(2):561–568
Sui K, Okabayashi T, Umeda Y et al (2021) Prognostic utility of the glasgow prognostic score for the long-term outcomes after liver resection for intrahepatic cholangiocarcinoma: a multi-institutional study. World J Surg 45(1):279–290
Shiba H, Misawa T, Fujiwara Y et al (2015) Glasgow prognostic score predicts outcome after surgical resection of gallbladder cancer. World J Surg 39(3):753–758
Kobayashi T, Kawakamil M, Hara Y et al (2014) Combined evaluation of the Glasgow prognostic score and carcinoembryonic antigen concentration prior to hepatectomy predicts postoperative outcomes in patients with liver metastasis from colorectal cancer. Hepatogastroenterology 61(133):1359–1362
Haruki K, Shiba H, Horiuchi T et al (2017) Impact of the C-reactive protein to albumin ratio on long-term outcomes after hepatic resection for colorectal liver metastases. Am J Surg 214(4):752–756
Okimoto S, Kobayashi T, Tashiro H et al (2017) Significance of the Glasgow Prognostic Score for patients with colorectal liver metastasis. Int J Surg 42:209–214
Solaini L, Atmaja BT, Arumugam P et al (2016) The role of perioperative inflammatory-based prognostic systems in patients with colorectal liver metastases undergoing surgery. A cohort study Int J Surg 36(Pt A):8–12
Kobayashi T, Teruya M, Kishiki T et al (2010) Elevated C-reactive protein and hypoalbuminemia measured before resection of colorectal liver metastases predict postoperative survival. Dig Surg 27(4):285–290
Ishizuka M, Kita J, Shimoda M et al (2009) Systemic inflammatory response predicts postoperative outcome in patients with liver metastases from colorectal cancer. J Surg Oncol 100(1):38–42
Halazun KJ, Aldoori A, Malik HZ et al (2008) Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol 34(1):55–60
Køstner AH, Kersten C, Löwenmark T et al (2016) The prognostic role of systemic inflammation in patients undergoing resection of colorectal liver metastases: C-reactive protein (CRP) is a strong negative prognostic biomarker. J Surg Oncol 114(7):895–899
Fretland AA, Dagenborg VJ, Bjornelv GMW et al (2018) Laparoscopic versus open resection for colorectal liver metastases: The OSLO-COMET randomized controlled trial. Ann Surg 267(2):199–207
Aghayan DL, Kazaryan AM, Dagenborg VJ et al (2021) Long-term oncologic outcomes after laparoscopic versus open resection for colorectal liver metastases: a randomized trial. Ann Intern Med 174(2):175–182
Syn NL, Kabir T, Koh YX et al (2020) Survival advantage of laparoscopic versus open resection for colorectal liver metastases: a meta-analysis of individual patient data from randomized trials and propensity-score matched studies. Ann Surg 272(2):253–265
Robles-Campos R, Lopez-Lopez V, Brusadin R et al (2019) Open versus minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc 33(12):3926–3936
Fretland AA, Sokolov A, Postriganova N et al (2015) Inflammatory response after laparoscopic versus open resection of colorectal liver metastases: data from the Oslo-CoMet Trial. Medicine 94(42):e1786
Nymo LS, Soreide K, Kleive D et al (2019) The effect of centralization on short term outcomes of pancreatoduodenectomy in a universal health care system. HPB 21(3):319–327
Lassen K, Nymo LS, Kørner H et al (2018) The New National Registry for Gastrointestinal Surgery in Norway: NoRGast. Scand J Surg 107(3):201–207
Soreide K, Olsen F, Nymo LS et al (2018) A nationwide cohort study of resection rates and short-term outcomes in open and laparoscopic distal pancreatectomy. HPB 21(6):669–678
Nymo LS, Kleive D, Waardal K et al (2020) Centralizing a national pancreatoduodenectomy service: striking the right balance. BJS open 4(5):904–913
von Elm E, Altman DG, Egger M et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Porembka MR, Hall BL, Hirbe M et al (2010) Quantitative weighting of postoperative complications based on the accordion severity grading system: demonstration of potential impact using the american college of surgeons national surgical quality improvement program. J Am Coll Surg 210(3):286–298
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahakyan, M.A., Brudvik, K.W., Angelsen, JH. et al. Preoperative Inflammatory Markers in Liver Resection for Colorectal Liver Metastases: A National Registry-Based Study. World J Surg 47, 2213–2220 (2023). https://doi.org/10.1007/s00268-023-07035-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07035-z