Abstract
Background
Major abdominal surgery is associated with bleeding and venous thromboembolism (VTE) risks. Chemoprophylaxis prevents VTE but increases bleeding risk. When compared with pre- and intra-operative chemoprophylaxis, recent evidence suggests that starting chemoprophylaxis postoperatively lowers the risk of bleeding without compromising VTE protection. This study investigates whether an optimal window exists in the postoperative period for initiating chemoprophylaxis in patients undergoing major abdominal surgery.
Methods
Analysis of pooled data from four multicenter PROTECTinG studies, which investigated the timing of perioperative chemoprophylaxis on bleeding and VTE outcomes following major abdominal surgery. Patients that commenced chemoprophylaxis postoperatively were separated into quartiles based on timing of administration within the first 24 h post-surgery.
Results
Overall, 4729 (Abdominal visceral resection N = 668, cholecystectomies N = 573, major ventral hernia repair N = 1701, antireflux surgery N = 1787) consecutive patients had chemoprophylaxis commenced within 24 h following elective surgery. Baseline characteristics were comparable between quartiles. Across quartiles and within each procedural type, the timing of starting chemoprophylaxis was not associated with bleeding (2.6, 1.7, 2.7 and 3.2%, p = 0.130) or clinical VTE (0.8, 0.2, 0.8 and 0.5%, p = 0.131), and did not predict their occurrences on multivariate analysis.
Conclusion
Chemoprophylaxis can be safely started at any time within 24 h post-skin closure in major abdominal surgery, without affecting bleeding or VTE risks. This finding encourages the standardization of chemoprophylaxis timing in the postoperative period to pre-defined times during the day to improve workflow efficiency and chemoprophylaxis compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) is an important preventable postoperative complication associated with significant morbidity, mortality and economic burden [1]. Major abdominal surgery incurs a high risk of VTE [2]. Consequently, it is standard practice to administer chemical and mechanical thromboprophylaxis in the perioperative setting [3]. Although chemoprophylaxis decreases VTE risk, it also increases bleeding risk [4]. Thus, when prescribing chemoprophylaxis, the risk and consequences of VTE need to be balanced against that of bleeding. Guidelines exist to facilitate chemoprophylaxis prescription but they do not specify the optimal timing of administration [5].
The PROTECTinG (Perioperative Timing of Elective Chemical Thromboprophylaxis in General Surgery) research group within the VERITAS (Victorian-collaborative for Education, Research, Innovation, Training and Audit by Surgical trainees) collaborative was established to address this gap in perioperative guidelines. Our studies have shown that postoperative chemoprophylaxis is favored over early (preoperative and intraoperative) administration in the settings of elective cholecystectomy [6], major abdominal resection [7], ventral hernia repair [8], and anti-reflux surgery. These findings were subsequently validated in patients with high baseline VTE risk [9], and by meta-analysis of published literature, which focused on patients undergoing major abdominal surgery [10]. Together, these studies have conclusively demonstrated that following major abdominal surgery, postoperative chemoprophylaxis results in a lower risk of bleeding without compromising VTE protection when compared with early administration. Additionally, other studies have demonstrated that therapeutic anticoagulation (using oral agents for patients with atrial fibrillation) can be safely restarted 24 h after skin-closure without an increased bleeding risk [11, 12]. Unfortunately, these studies do not report on VTE endpoints. Therefore, what remains unknown is the optimal timing of starting chemoprophylaxis in the postoperative period following major abdominal surgery.
The relative paucity of evidence directing timing of chemoprophylaxis has contributed to considerable variation in practice between hospitals and surgeons [3]. Furthermore, as identified by the Australian Commission on Safety and Quality in Health Care, despite internationally recognized guidelines recommending VTE risk assessment and provision of thromboprophylaxis, not all patients are receiving this standard-of-care [13]. As highlighted by multiple studies, usage rates are consistently suboptimal [14, 15], with one large study reporting only 62% of at-risk surgical patients receiving appropriate chemoprophylaxis [2]. There are many reasons for poor compliance, however, this is often due to a failure to prescribe or administer chemoprophylaxis during busy clinical schedules. In this context, knowledge of an ideal window for initiating chemoprophylaxis in the postoperative period, if one exists, taking into account bleeding and VTE risks, will greatly facilitate guideline development and standardization of thromboprophylactic practices. Such a system-wide approach will help ensure that all patients receive appropriate chemoprophylaxis in the postoperative period.
Accordingly, we undertook a multicenter study to determine whether an optimal window exists in the postoperative period for commencing chemoprophylaxis in patients undergoing major abdominal surgery.
Methods
Study design
A retrospective analysis of pooled data from 4 multicenter studies was conducted by PROTECTinG investigators, which examined the impact of perioperative timing of chemoprophylaxis following elective cholecystectomies [6], abdominal visceral resections [7], major ventral hernia repairs [8], and anti-reflux surgery. Details of these studies are summarized in Table S1-2. Patients were identified from prospectively maintained databases or from each hospital’s administrative database using the Australian Classification of Health Interventions procedural codes [3]. All patients had chemoprophylaxis commenced within 24 h postoperatively. Patients were excluded if under 18 years-of-age, who underwent an emergency procedure, and those who had chemoprophylaxis initiated before skin closure. This study was approved by the Human Research Ethics Committee across all centers.
Venous thromboembolism prophylaxis
Thromboprophylaxis included both mechanical and chemical methods. Mechanical thromboprophylaxis comprised sequential compression devices (SCD) and thromboembolic deterrent stockings (TEDS). Chemoprophylaxis included subcutaneous injection of either enoxaparin (daily), heparin (twice daily), or dalteparin (daily), at doses adjusted to each patients’ creatinine clearance and weight. Postoperative chemoprophylaxis refers to administration of any of the above anticoagulants at prophylactic doses after skin closure. The type and timing of chemoprophylaxis across all centers for all operations were at the discretion of the treating team. Additionally, chemoprophylaxis was not administered within 12 h of regional anesthesia.
Data collection and quality assurance
Data was pooled from each PROTECTinG study onto a universal electronic proforma. This included patient demographics, comorbidities, perioperative parameters, operative details, postoperative timing of chemoprophylaxis, postoperative bleeding, and VTE events. As described in each PROTECTinG study, an array of quality assurance measures was undertaken to maximize data accuracy and minimize inter-observer discrepancies [6,7,8]. Consequently, a random audit of 10% of data fields for each study demonstrated a mean accuracy rate of 98.1% (range 97.7–98.4%), as outlined in Table S1.
Study endpoints and definitions
All study endpoints were stipulated and defined a priori. Our primary endpoint was postoperative bleeding risk. Secondary endpoints included rates of major bleeding, minor bleeding, reintervention for bleeding, hemoglobin changes post-surgery and 30-day clinical VTE rate. We used Caprini score to evaluate patients’ risk of VTE (≤2: low, 3–4: moderate, ≥5: high risk). We defined clinical VTE as radiologically proven (CTPA, V/Q scintigraphy, venous ultrasound) symptomatic disease occurring within 30 days post-surgery. The criteria for major bleeding included either the need for blood transfusion, reintervention (surgical, endoscopic or radiological), or a >20 g/L fall in hemoglobin from baseline [6,7,8]. Minor bleeding refers to any bleeding event failing to meet major bleeding criteria. As guided by local hospital policies, oral antiplatelets and anticoagulants (excluding aspirin) were withheld 3 to 7 days prior to surgery. For those patients who required ongoing therapeutic anticoagulation, bridging enoxaparin was used up to 24 h pre-surgery. There was a 4–6-week follow-up period for all patients following discharge.
Statistical analysis
To determine whether time to starting chemoprophylaxis affected bleeding and VTE risk, we analyzed time as a categorical and continuous variable. For the former, we separated patients into 6 hourly quartiles post-surgery. For the latter, we analyzed time as a continuum in a multivariate analysis. Continuous variables were assessed using the Student’s t-test for 2 variables and analysis of variance (ANOVA) for >2 variables. Categorical variables were assessed using the Fisher’s exact test for 2 variables and chi square for >2 variables. To determine independent predictors of post-operative bleeding and VTE, and account for differences in Australian state-based practices, a hierarchical multivariate logistic regression analysis was undertaken. In this model, covariates were treated as fixed effects, whereas Australian states were treated as a random effect. For 2 variable comparison, a two-tailed p < 0.05 and 95% confidence interval (CI) around the odds ratio (OR) that did not cross one was considered statistically significant. For comparison involving >2 variables, a Bonferroni corrected p value was calculated to account for multiple comparisons. Statistical analyses were conducted using Prism v9 (GraphPad Software, San Diego, CA, USA) and R v4.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
Power calculation
Based on our own data and published studies [3, 4], the overall risk of bleeding following major abdominal surgery in patients who receive postoperative chemoprophylaxis is approximately 3%. We considered a >1.5% absolute risk difference or >50% relative risk difference between study groups as clinically significant. Given that our entire study cohort is divided into quartiles based on the time of starting chemoprophylaxis postoperatively, and therefore we assumed a 1:1:1:1 ratio of sample size within each quartile, the total sample size required was 3200 patients (800 patients per quartile) to detect a 1.5% absolute difference (50% relative difference) in bleeding events between any two quartiles with 80% statistical power (alpha < 0.05).
Results
Baseline patient characteristics
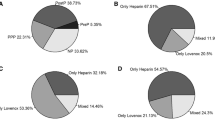
In total, we analyzed 4729 consecutive patients who underwent major abdominal surgery and had chemoprophylaxis initiated within the first 24 h post-surgery. These patients were separated into quartiles based on their timing of chemoprophylaxis administration. The median (range) time for each quartile are as follows; Quartile 1: 4.3 (0.0–6.0) hours, quartile 2: 7.5 (6.3–8.6) hours, quartile 3: 14.0 (12.0–15.7) hours, and quartile 4: 21.2 (18.0–24.0) hours. Within all four major abdominal surgery cohorts, anti-reflux surgery (N = 1787), ventral hernia repair (N = 1701), major visceral resection (N = 668) and elective cholecystectomy (N = 573), quartiles were largely comparable in demographic, operative and perioperative characteristics (Tables S3-6). Minor but statistically significant differences between quartiles were found with respect to chemoprophylaxis type for the anti-reflux surgery population (Table S3), hernia type and location for the ventral hernia repair population (Table S4), and surgeon seniority for the major visceral resection population (Table S5). Notably, Caprini score, antiplatelet, and anticoagulant use as well as duration of surgery were similar between quartiles for all four major abdominal surgery cohorts.
Postoperative chemoprophylaxis timing was not associated with bleeding
There were no significant differences in bleeding rates between quartiles for the overall cohort of patients (2.6%, 1.7%, 2.7% and 3.2%, p = 0.13). Sub-group analysis for anti-reflux surgery (0.6%, 0.4%, 1.3%, 1.2%, p = 0.373), ventral hernia repair (3.3%, 2.9%, 3.6%, 3.8%, p = 0.905), major visceral resection (8.6%, 3.5%, 7.9%, 6.2%, p = 0.243) and cholecystectomy (0.2%, 0.2%, 0.0%, 3.0%, p = 0.064) also did not show significant differences in bleeding rates between quartiles (Table 1). Furthermore, there was no significant difference in major bleeding, minor bleeding, reintervention for bleeding or hemoglobin changes between quartiles in any of these four major abdominal surgery cohorts. Patients with postoperative bleeding had a significantly longer length of stay (mean (SD), 13.3 (18.9) versus 4.2 (9.8) days, p < 0.001) compared to non-bleeders. The mean (SD) time to commence chemoprophylaxis post-skin closure was 814.9 (777.8) minutes for bleeders and 689.0 (503.4) minutes for non-bleeders (p = 0.058). Overall and within each procedural type, an optimal time for commencing postoperative chemoprophylaxis in which bleeding was significantly lower was not observed.
Postoperative chemoprophylaxis timing was not associated with thromboembolism
There was no significant difference in VTE rates between quartiles for postoperative timing of chemoprophylaxis. Clinical VTE occurred in 10 (0.8%), 2 (0.2%), 9 (0.8%) and 6 (0.5%) patients for each quartile (p = 0.131). There was similarly no significant variability amongst quartiles when VTE outcomes were separated into DVT and PE (Table 2). Additionally, on subgroup analysis, no association was found between each quartile and VTE risk for anti-reflux surgery (1.3%, 0.2%, 0.8% and 1.0%, p = 0.286), ventral hernia repair (0.5%, 0.3%, 0.4% and 0.0%, p = 0.490) and major visceral resection (0.6%, 0.0%, 2.1% and 1.0%, p = 0.243). A p-value was not derived for the cholecystectomy cohort as a VTE event (DVT) occurred in only 1 of the 573 patients. The occurrence of VTE was associated with an extended hospital stay (mean (SD), 12.4 (14.7) versus 4.4 (10.2) days, p < 0.001). The mean (SD) time to commence chemoprophylaxis post-skin closure was 713.0 (630.4) minutes for patients who developed VTE and 692.1 (511.8) minutes for those free from VTE (p = 0.833). Overall and within each procedural type, an optimal time for commencing postoperative chemoprophylaxis in which VTE rates were significantly lower was not observed.
Predictor of postoperative bleeding
Univariate analysis identified the following factors to be significantly associated with postoperative bleeding: older age, male gender, higher Caprini score, anesthesia type, surgical approach, higher ASA score, longer surgical duration, pre-existing antiplatelet or anticoagulant use, and repeated chemoprophylaxis dosing (Table 3). Of these, multivariate analysis identified older age (OR 1.02, 95% CI 1.01–1.04, p = 0.002), longer surgical duration (OR 1.89, 95% CI 1.29–2.77, p = 0.001), and pre-existing anti-platelet use (OR 1.69, 95%CI 1.09–2.62, p = 0.020) to be independent predictors of postoperative bleeding following major abdominal surgery. Importantly, chemoprophylaxis timing expressed as a categorical or continuous variable was not associated with, or predictive of, postoperative bleeding on univariate or multivariate analysis, respectively.
Predictor of postoperative venous thromboembolism
Factors that were significantly associated with postoperative VTE on univariate analysis included older age, higher Caprini score, higher ASA score, longer surgical duration, and repeated chemoprophylaxis dosing (Table 4). Multivariate analysis demonstrated higher Caprini score (OR 1.20, 95% CI 1.07–1.33, p = 0.001) and longer surgical duration (OR 2.20, 95% CI 1.16–4.17, p = 0.016) to be independent predictors of clinical VTE following major abdominal surgery. Similarly, chemoprophylaxis timing expressed as a categorical or continuous variable was not associated with, or predictive of, postoperative VTE on univariate or multivariate analysis, respectively.
Discussion
This is the first study to investigate the optimal postoperative timing of chemoprophylaxis in major abdominal surgery. Our incidence of clinical VTE and bleeding are comparable to published data on anti-reflux surgery [16,17,18,19], ventral hernia repair [20,21,22,23], major visceral resection [24,25,26], cholecystectomy [20, 27,28,29,30,31,32], and elective general surgery [33,34,35]. Whilst VTE risk necessitates chemoprophylaxis in the perioperative setting, strong evidence now exists demonstrating that chemoprophylaxis confers a clinically significant risk of bleeding [4]. Multiple studies now show that postoperative commencement of chemoprophylaxis is favored over pre- and intra-operative administration because of reduced bleeding risk while preserving VTE protection [24, 26, 36,37,38,39]. In this study, our findings indicate that there is no optimal time window for initiating chemoprophylaxis in the early postoperative period. As long as it is given within 24 h of skin closure, both VTE and bleeding risks remain acceptably low.
The significance of this finding is that it informs protocol development towards standardization of thromboprophylactic practices. The current variability in practice likely contributes to the recognized suboptimal compliance with administering chemoprophylaxis prescriptions [40, 41]. Furthermore, non-compliance has been cited as a major reason for surgeons prescribing chemoprophylaxis preoperatively (a practice associated with increased risk of bleeding and no additional VTE protection) [42]. We propose that protocolizing chemoprophylaxis on the surgical ward to set times during the day will likely be easier for nursing staff to manage. With this approach, should an operation finish after one set time, chemoprophylaxis will be given at the next designated time point. This method is different to surgeons requesting chemoprophylaxis to start at fixed intervals postoperatively, as the latter will result in multiple inpatients needing chemoprophylaxis administered at multiple, and often at odd hours of the day (or night). Such practices may lead to confusion and neglect, particularly during periods of high clinical demand, thus compromising adequate thromboprophylaxis. In contrast, standardizing postoperative chemoprophylaxis to specific times during the day fosters routine, enables integration into pre-existing workflows, and allows nursing staff to anticipate and plan, which ultimately may improve compliance to thromboprophylaxis, and patient safety.
There are inherent limitations within this retrospective study. Moreover, we did not search for an optimal chemoprophylaxis window beyond 24 h of skin closure. This is because evidence already exist demonstrating the safety of commencing therapeutic anticoagulation at 24 h post-surgery [11], and it is uncommon for clinicians to delay chemoprophylaxis beyond 24 h post-surgery unless there were specific concerns for bleeding. Additionally, the incidence of clinical VTE may be underestimated in this study as patients may present to other health services for treatment. However, all patients were followed-up between 4–6 weeks post-surgery, and as noted earlier, our reported rates of clinical VTE are comparable to contemporary series [33,34,35]. We are unable to provide 90-day bleeding or clinical VTE rates as patients were not universally followed-up after 6 weeks post-surgery.
Conclusion
The timing of initiating chemoprophylaxis within 24 h postoperatively is not significantly associated with bleeding and clinical VTE after major abdominal surgery. Given the low risk of bleeding and clinical VTE associated with postoperative chemoprophylaxis, our findings advocate for standardization of chemoprophylaxis timing in the postoperative period to improve compliance with administration.
References
Access Economics (2008) The burden of venous thromboembolism in Australia. Report for The Australia and New Zealand Working Party on the Management and Prevention of Venous Thromboembolism. Available at: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/burden-venous-thromboembolism-australia. Accessed 15 Sept 2022
Kakkar AK, Cohen AT, Tapson VF et al (2010) Venous thromboembolism risk and prophylaxis in the acute care hospital setting (ENDORSE survey): findings in surgical patients. Ann Surg 251:330–338
Liu DS, Stevens S, Wong E et al (2020) Variations in practice of thromboprophylaxis across general surgical subspecialties: a multicentre (PROTECTinG) study of elective major surgeries. ANZ J Surg 90:2441–2448
Leonardi MJ, McGory ML, Ko CY (2006) The rate of bleeding complications after pharmacologic deep venous thrombosis prophylaxis: a systematic review of 33 randomized controlled trials. Arch Surg 141:790–797; discussion 797–799
Gould MK, Garcia DA, Wren SM et al (2012) Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e227S-e277S
Liu DS, Stevens S, Wong E et al (2020) Pre-operative and intra-operative chemical thromboprophylaxis increases bleeding risk following elective cholecystectomy: a multicentre (PROTECTinG) study. ANZ J Surg 90:2449–2455
Liu DS, Newbold R, Stevens S et al (2022) Early versus postoperative chemical thromboprophylaxis is associated with increased bleeding risk following abdominal visceral resections: a multicenter cohort study. J Gastrointest Surg 26:1495–1502
PROTECTinG investigators, VERITAS collaborative, (2022) Chemical thromboprophylaxis before skin closure increases bleeding risk after major ventral hernia repair: a multicenter cohort study. Surgery 172:198–204
Liu DS, Stevens SG, Watson DI et al (2022) Optimal timing of perioperative chemoprophylaxis in patients with high thromboembolic risk undergoing major abdominal surgery: a multicenter cohort study. Ann Surg. https://doi.org/10.1097/SLA.0000000000005697
Klonis C, Ashraf H, Cabalag CS et al (2022) Optimal timing of perioperative chemical thromboprophylaxis in elective major abdominal surgery: a systematic review and meta-analysis. Ann Surg. https://doi.org/10.1097/SLA.0000000000005764
Douketis JD, Spyropoulos AC, Duncan J et al (2019) Perioperative management of patients with atrial fibrillation receiving a direct oral anticoagulant. jama intern med 179:1469–1478
Douketis JD, Spyropoulos AC, Murad MH, et al (2022) Perioperative Management of Antithrombotic Therapy: An American College of Chest Physicians Clinical Practice Guideline Executive Summary. Chest
Australian Commission on Safety and Quality in Health Care (2020) Venous Thromboembolism Prevention Clinical Care Standard. Available from: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/venous-thromboembolism-prevention-clinical-care-standard-2020. Accessed 15 Sept 2022
Otero R, Uresandi F, Cayuela A et al (2001) Use of venous thromboembolism prophylaxis for surgical patients: a multicentre analysis of practice in Spain.
Yu HT, Dylan ML, Lin J et al (2007) Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm 64:69–76
Cuschieri A, Hunter J, Wolfe B et al (1993) Multicenter prospective evaluation of laparoscopic antireflux surgery. Preliminary report Surg Endosc 7:505–510
Nguyen NT, Hinojosa MW, Fayad C et al (2007) Laparoscopic surgery is associated with a lower incidence of venous thromboembolism compared with open surgery. Ann Surg 246:1021–1027
Schlottmann F, Strassle PD, Patti MG (2017) comparative analysis of perioperative outcomes and costs between laparoscopic and open antireflux surgery. J Am Coll Surg 224:327–333
Schlottmann F, Strassle PD, Patti MG (2018) Antireflux surgery in the USA: Influence of surgical volume on perioperative outcomes and costs-time for centralization? World J Surg 42:2183–2189
Alizadeh RF, Sujatha-Bhaskar S, Li S et al (2017) Venous thromboembolism in common laparoscopic abdominal surgical operations. Am J Surg 214:1127–1132
Helm JH, Helm MC, Kindel TL et al (2019) Blood transfusions increase the risk of venous thromboembolism following ventral hernia repair. Hernia 23:1149–1154
Pannucci CJ, Basta MN, Fischer JP et al (2015) Creation and validation of a condition-specific venous thromboembolism risk assessment tool for ventral hernia repair. Surgery 158:1304–1313
Ross SW, Kuhlenschmidt KM, Kubasiak JC et al (2020) Association of the risk of a venous thromboembolic event in emergency vs elective general surgery. JAMA Surg 155:503–511
Doughtie CA, Priddy EE, Philips P, et al (2014) Preoperative dosing of low-molecular-weight heparin in hepatopancreatobiliary surgery. Am J Surg 208:1009–1015; discussion 1015
Kakkar AK, Agnelli G, Fisher W et al (2014) Preoperative enoxaparin versus postoperative semuloparin thromboprophylaxis in major abdominal surgery: a randomized controlled trial. Ann Surg 259:1073–1079
Zaghiyan KN, Sax HC, Miraflor E et al (2016) Timing of chemical thromboprophylaxis and deep vein thrombosis in major colorectal surgery: a randomized clinical trial. Ann Surg 264:632–639
Gundogdu RH, Oduncu M, Bozkirli BO et al (2017) Does thromboprophylaxis cause bleeding after laparoscopic cholecystectomy? Bratisl Lek Listy 118:156–159
Henry ML, Abdul-Sultan A, Walker AJ et al (2020) Duration and magnitude of postoperative risk of venous thromboembolism after cholecystectomy: a population-based cohort study. Dig Surg 37:32–38
Persson G, Stromberg J, Svennblad B et al (2012) Risk of bleeding associated with use of systemic thromboembolic prophylaxis during laparoscopic cholecystectomy. Br J Surg 99:979–986
Rondelli F, Manina G, Agnelli G et al (2013) Venous thromboembolism after laparoscopic cholecystectomy: clinical burden and prevention. Surg Endosc 27:1860–1864
Stein PD, Matta F, Sabra MJ (2014) Pulmonary embolism and deep venous thrombosis following laparoscopic cholecystectomy. Clin Appl Thromb Hemost 20:233–237
Stromberg J, Sadr-Azodi O, Videhult P et al (2015) Incidence and risk factors for symptomatic venous thromboembolism following cholecystectomy. Langenbecks Arch Surg 400:463–469
Assareh H, Chen J, Ou L et al (2014) Rate of venous thromboembolism among surgical patients in Australian hospitals: a multicentre retrospective cohort study. BMJ Open 4:e005502
Mukherjee D, Lidor AO, Chu KM et al (2008) Postoperative venous thromboembolism rates vary significantly after different types of major abdominal operations. J Gastrointest Surg 12:2015–2022
Sakon M, Kakkar AK, Ikeda M et al (2004) Current status of pulmonary embolism in general surgery in Japan. Surg Today 34:805–810
Altieri MS, Yang J, Hajagos J et al (2018) Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc 32:4805–4812
Hull RD, Pineo GF, Francis C et al (2000) Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs warfarin in hip arthroplasty patients: a double-blind, randomized comparison. The North American Fragmin Trial Investigators. Arch Intern Med 160:2199–2207
McAlpine K, Breau RH, Werlang P et al (2021) Timing of perioperative pharmacologic thromboprophylaxis initiation and its effect on venous thromboembolism and bleeding outcomes: a systematic review and meta-analysis. J Am Coll Surg 233(619–631):e614
Taghlabi K, Carlson BB, Bunch J et al (2022) Chemoprophylactic anticoagulation 72 hours after spinal fracture surgical treatment decreases venous thromboembolic events without increasing surgical complications. N Am Spine Soc J 11:100141
Fanikos J, Stevens LA, Labreche M et al (2010) Adherence to pharmacological thromboprophylaxis orders in hospitalized patients. Am J Med 123:536–541
Shermock KM, Lau BD, Haut ER et al (2013) Patterns of non-administration of ordered doses of venous thromboembolism prophylaxis: implications for novel intervention strategies. PLoS ONE 8:e66311
Liu DS, Wong E, Fong J et al (2020) Perioperative thromboprophylaxis is highly variable in general surgery: results from a multicentre survey. ANZ J Surg 90:2401–2403
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Consortia
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This study was approved by Human Research Ethics Committee from all participating sites.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Correspondence to: David S. Liu, General and Gastrointestinal Surgery Research Group, The University of Melbourne Department of Surgery, Austin Health, 145 Studley Road, Heidelberg, VIC 3084, Australia; Division of Surgery, Anaesthesia and Procedural Medicine, Austin Hospital; and Division of Cancer Surgery, Peter MacCallum Cancer Centre, 305 Grattan Street, Melbourne, VIC 3000, Australia.
Email: liu.davidsh@gmail.com
lTwitter: @Dr.DavidSLiu
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
PROTECTinG investigators., VERITAS Collaborative. Postoperative Timing of Chemoprophylaxis and Its Impact on Thromboembolism and Bleeding Following Major Abdominal Surgery: A Multicenter Cohort Study. World J Surg 47, 1174–1183 (2023). https://doi.org/10.1007/s00268-023-06899-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-06899-5