Abstract
Background
Brazil is a middle-income country that aims to provide universal health coverage, but its surgical system’s efficiency has rarely been analyzed. In an effort to strengthen surgical national systems, the Lancet Commission on Global Surgery proposed bellwether procedures as quality indicators of surgical workforces. This study aims to evaluate regional inequalities in access to bellwether procedures and their associated mortality across the five Brazilian geographical regions.
Methods
Using DATASUS, Brazil’s national healthcare database, data were collected on the total amount of performed bellwether procedures—cesarean section, laparotomy, and open fracture management—and their associated mortality, by geographical region. We evaluated the years 2018–2020, both in emergent and elective conditions. Statistical analysis was performed by one-way ANOVA test and Tukey’s multiple comparisons test.
Results
During this period, DATASUS registered 2,687,179 cesarean sections, 1,036,841 laparotomies, and 648,961 open fracture treatments. The access and associated mortality related to these procedures were homogeneous between the regions in elective care. There were significant geographical inequalities in access and associated mortality in emergency care (p < 0.05, 95% CI) for all bellwether procedures. The Southeast, the most economically developed region of the country, was the region with the lowest amount of bellwether procedures per 100,000 inhabitants.
Conclusion
Brazil’s public surgical system is competent at promoting elective surgical care, but more effort is needed to fortify emergency care services. Public policies should encourage equity in the geographic allocation of the surgical workforce.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery-manageable diseases account for 28% of the global disease burden [1]. Logically, a scale-up of a functional surgical system could benefit a large portion of the global population, potentially saving millions of lives that lack access to surgical procedures. In this regard, the Lancet Commission on Global Surgery (LCoGS) was established with the goal of integrating surgery into the global health agenda, promoting political change, and defining scalable solutions for providing quality surgery to all [2]. The LCoGS stated that access to bellwether procedures could serve as a quality indicator for surgical systems.
Bellwether procedures can be defined as a group of operations that have been identified as markers of a healthcare system’s capability to provide essential and emergency surgical care [3]. They are composed of three surgical procedures, which are cesarean section (CS), a procedure in which the baby is delivered through an incision in the abdominal wall and the uterus [4]; laparotomy, an open procedure used to treat a wide range of surgically manageable diseases such as penetrating abdominal injuries and acute abdomen [5]; and treatment of open bone fractures, injuries in which the body's protective skin barrier has been broken and the potential for contamination is high [6]. Previous research found that the ability to perform bellwether procedures was strongly linked to the ability to perform all obstetric, general, basic, emergency, and orthopedic procedures in low and middle-income countries [7].
Brazil is a developing Latin-American country that aspires to provide universal health coverage through Sistema Único de Saúde (SUS) or Unified Health System. This system is based on the principles of comprehensiveness, equality, and universality, with a strong emphasis on primary care [8]. Providing equal access to SUS is a major challenge for the public healthcare system, given that the country comprises five geographical regions with distinct socioeconomic and historical backgrounds [9]. In fact, Brazil was the world's most unequal country in the 1980s, and this regional inequality became more evident in historically excluded regions of the country, such as the Northeast, Midwest, and the North, where the supply of health services is lower than in the South and Southeast regions. In those three regions, health facilities are usually located at a greater distance, making it difficult to access surgical care [9].
The primary goal of this study was to assess regional differences in access to bellwether procedures between the five Brazilian geographical regions, both in emergency and elective scenarios. We also assessed the associated mortality related to these procedures. As a result, we intend to evaluate the quality of the Brazilian public surgery system and guide future public policies to improve it.
Material and methods
The total number of bellwether procedures (CS, laparotomy, and open fracture management) performed and their associated mortality for all patient admissions in Brazil’s public hospitals were collected in the period 2018–2020, both in emergent and elective conditions. These data were compared between the five Brazilian geographical regions: Midwest, North, Northeast, South, and Southeast.
Source of data
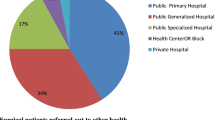
The data of this study were collected from DATASUS, a national, open-access database organized and funded by the federal government that contains aggregate data from the Hospital Information System (SIH). In this system, individual hospitals submit a monthly formal report that contemplates a variety of diagnostic and procedural statistics. SIH collects information on 60–70% of hospital admissions in the country within the Unified Health System [3]. These data do not include private healthcare information, for which approximately 28.5% of the population is covered [10].
Data about the number of bellwether procedures and their associated mortality, between 2018 and 2020 per Brazilian geographical region, were collected in elective and emergent contexts. The unique procedure-related codes used to access data on bellwether procedures in DATASUS were the same as cited in a previous study [3]. Microsoft Excel 365 was used to tabulate data and construct a figure summarizing results for Brazilian regions (Fig. 1).
Regional inequalities in access and mortality rate related to bellwether procedures in Brazil. The color gradient represents the mean amount of procedures between 2018 and 2020, per 100,000 inhabitants, with the darkest shade corresponding to the highest registered number. The gray circles represent the mean mortality rate during the same period, per 100,000 inhabitants, and their sizes are proportional to the registered value
Given the differences in population between the five Brazilian geographical regions and the biases that it could represent in the research, the results regarding the total annual number of procedures and associated mortality were divided by the total population of the region in 2021, according to Brazilian Institute of Geography and Statistics [11], which is the country's most important source of demographic data. Following, the mean amount for each bellwether procedure per 100,000 inhabitants in each region, both in elective and emergent contexts, and the associated mean mortality rate, between the years 2018 and 2020, were calculated. The standard deviations of the means were also assessed.
Statistical analysis
Statistical analyses were performed using the statistical program GraphPad Prism version 8.0.0 (GraphPad Software, California, USA). Since the total number of procedures per region and associated death rate between 2018 and 2020 were normally distributed according to the D'Agostino-Pearson normality test (p > 0.05), analysis of variance was performed by one-way ANOVA and Tukey’s multiple comparisons tests. We considered a 95% confidence interval. Differences in data that reached p < 0.05 were considered statistically significant.
Results
Cesarean section
Of the 2,687,179 procedures reported, 4.5% (121,046) were elective, and 95.5% (2,566,133) were emergencies. In terms of mortality, 1232 deaths were reported, with 3.09% (38) occurring during elective and 96.91% (1194) occurring during emergency procedures. Figure 1 synthesizes the mean results in mortality and amount of procedures, both in elective and emergent contexts on the period, for all the bellwether procedures.
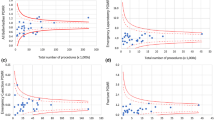
Regarding elective procedures, there were no differences in access (Fig. 2) and associated mortality (Fig. 3) between the five Brazilian geographical regions (p > 0.05). Relating to emergency procedures, all Brazilian regions presented inequalities in access, as presented in Fig. 4. Associated mortality in emergencies also presented differences between the regions as shown in Fig. 5.
Mean amount of emergency procedures per 100,000 inhabitants between 2018 and 2020. Error bars indicate the standard deviation (SD). “*” represents the statistically significant difference (p < 0.05) unless otherwise noted. All comparisons were statistically significant. a Cesarean sections. b Laparotomies. c Open fracture management
Mean associated mortality of emergency procedures per 100,000 inhabitants between 2018 and 2020. Error bars indicate the standard deviation (SD). “*” represents the statistically significant difference (p < 0.05) unless otherwise noted. a Cesarean sections. b Laparotomies. c Open fracture management
Concerning the mean amount of CS performed in the period, the Southeast region was the region that less performed this procedure both in elective and emergency contexts. In elective, the Midwest region was the region that most performed this procedure, 44.83% higher than the Southeast, and in emergency, the North was the region that most performed this procedure, 60.89% higher than the Southeast.
Related to the associated mortality of CS, in elective, Midwest was the region with the highest mortality, 331.45% higher than the Northeast, the region with the lowest mortality. In emergency, the North had the highest mortality rate, 193.98% higher than the South, which had the lowest.
Laparotomy
Of the 1,036,841 procedures reported, 37.5% (388,785) were elective procedures and 62.5% (648,056) emergency procedures. In total, 29,169 deaths were reported in the period, including 10.03% (2,924) during elective procedures and 89.97% (26,245) during emergencies.
There were no differences in access and associated mortality in elective laparotomy procedures between the five Brazilian geographical regions, and just one comparison, South versus Midwest, presented a statistically significant difference (p < 0.05) in associated mortality (Fig. 3). Concerning emergency procedures, there were significant inequalities both in access (Fig. 4) and mortality (Fig. 5).
In terms of the mean amount of laparotomies performed during the period, the lowest amount was registered for the Southeast, and the highest for the South, both in elective and emergency contexts (76.52% and 48.55% higher than the Southeast, respectively).
In elective laparotomies, associated mortality was found to be significantly higher in the South region, 59.23% higher than in the Midwest, with the lowest mortality. In emergencies, again, the South was the region with the highest mortality, 95.31% superior to the North, the region with the lowest mortality.
Treatment of open bone fractures
In the period of 2018–2020, 648,961 open fracture managements were reported in DATASUS, which included 12.98% (84,217) elective procedures and 87.02% (564,744) emergency procedures. Concerning mortalities reported in this period, 5467 deaths were reported, 4.7% (257) in elective and 95.3% (5,210) in emergency procedures.
There were no differences in access and associated mortality in elective open fracture procedures between the five regions (p > 0.05), except when comparing the access between the South and Midwest regions (Fig. 2) and the associated mortality between the Southeast and Midwest regions (Fig. 3). However, there were significant differences both in access (Fig. 4) and mortality (Fig. 5) related to emergency procedures, although associated mortality showed more statistically significant differences than access.
Concerning the mean amount in the period, in elective, the North region performed the procedure most, 78.8% higher than the Midwest, region with the lowest amount. Interestingly, in the emergency context, the scenario was opposed: the Midwest was the region that most performed this procedure, 90.02% higher than the North.
Related to the associated mortality, in elective, the Southeast was the region with the highest mortality, 216.9% higher than the Midwest, the region with the lowest mortality. In emergency, the South was the region with the highest mortality, 259.73% higher than the North, the region with the lowest number.
Discussion
In this work, we used the Brazilian public health database to evaluate differences in access and mortality rate related to bellwether procedures between the five Brazilian geographical regions, as these indicators represent the quality of the entire public surgical system. Our findings are important because it was found that while Brazil's elective environment may be effective at promoting surgical care, more has to be done to increase access and reduce mortality related to urgent procedures.
In addition to our main findings, we noticed that, despite having the highest surgical workforce density in the country [12], the Southeast region had the lowest mean amount between the three bellwether procedures per 100,000 inhabitants. It was an unexpected result because of the great proportion of academic surgical programs in this region [13]. This result could be explained by not evaluating the private practice since DATASUS represents hospital information regarding the public sector. 37.5% of the health insurance coverage in 2019 was concentrated in the Southeast region, and these unexpected findings may be due to a greater effect of the private sector in this region [10].
The key point of our work is that, despite the existence of a national healthcare system, regional variations are a major contributor to health inequalities in the country. For example, in laparotomy data, the South was the region that most performed this procedure in elective and urgent contexts. This region performed 25.06% more laparotomies by population than the Northeast, one of the poorest regions of the country, during the period evaluated. It can be related to the fact that exploratory laparotomies are high-risk and costly procedures that demand strong healthcare structures [14], which suggests that the differences observed between these two regions can be due to economic and social factors.
Additionally, emergency laparotomies had the highest mortality among the procedures analyzed in this study. It supports prior findings of other works that also observed high mortality and morbidity associated with laparotomies in emergencies [15, 16]. The South’s highest mortality rate associated with this procedure, both in emergency and elective contexts, can be due to the high surgical volume registered, but more work is needed to understand this result.
The treatment of open fractures is considered an orthopedic emergency due to the risk of contamination and death. The management of these fractures is challenging in the context of trauma care, and there are still controversies regarding its optimal timing [17]. Most of the current literature supports that the surgical treatment of open fractures should be done under urgent circumstances [18]. Our findings reveal that the surgical management regimen for open fractures in Brazil is following most of the current literature, with 87.02% of these procedures being performed as emergencies.
Based on CS data, we determined that the North, one of Brazil's poorest regions, was the one that most performed this procedure in the emergency context. The difference in rates of CS compared with the other regions could be explained by the demographic and social context of the North, where there is low coverage of public health services [9], resulting in poor prenatal care and compromising the detection of early maternal–fetal disorders that contraindicate vaginal delivery, which increases CS in an emergency scenario. This region also has the highest mortality in emergency CS, which may also be related to the difficulty of accessing medical services. In addition, the deficiency in health professionals and adequate structure to assist vaginal delivery, often demanding more time and staff, can lead to an indiscriminate amount of CS without strong clinical indication [19]. Despite CS representing a medical advancement, given its potential to save lives and avoid complications [20], there is an excess of the procedure in medical practice. In Latin America and the Caribbean, a study on CS rates in 150 countries showed that 40.5% of births occur by CS, reaching 55.6% in Brazil [19]. It represents a sociocultural problem because of the association of this procedure with increased risk to the health of the mother and the newborn [20].
The major limitation of this work, as an epidemiological study, is that it is necessary to consider reporting bias and the consequent distortion of data due to underreporting or reporting error, which is more common to occur in the North and Northeast of Brazil than in other regions [21]. Another limitation of our study is the emphasis placed on the public healthcare system, even though private insurance covers 28.5% of the population [10]. Regardless, our findings referred to a system that any Brazilian can access at any time and for free across the five Brazilian geographical regions.
Also, this study includes the year 2020 in the analysis, which is recognized by the COVID-19 international outbreak that impacted the Brazilian public health system. Previous studies show that there was a huge backlog in the delivery of elective operations during this year in Brazil, although health state-level policies were effective in ensuring minimal reductions in the delivery of emergent surgeries [22]. Our data about laparotomies and treatment of open bone fractures, available in Online Resource 1, are in accordance with these previous results, as we can see a decrease in the total number of elective procedures per 100,000 inhabitants in the year 2020.
Despite these limitations, this study utilized statistical techniques to conduct a detailed analysis of public data and provides an evaluation of regional surgical inequalities in Brazil. The access and associated mortality to the three bellwether procedures were described in this country for the first time, and the findings of this study have significant implications for the overall improvement of the public healthcare system.
Conclusion
Identifying access gaps is critical for evaluating barriers to providing equal surgical care. The current study highlights large geographical differences in emergency procedures, raising concerns about universality and equity, two of the guidelines of the Brazilian National Public Healthcare System [8]. Beyond differences in access, our results could reflect differences in practice, workforce, and the economic development of the Brazilian regions. In light of these findings, there is an urgent need to identify the origin of these differences and to solve them to overcome inequality in surgical care in Brazil. We hope that this research may contribute to the development of public policies that will improve surgical access across the country, benefiting especially those who cannot afford healthcare insurance.
References
Shrime MG, Bickler SW, Alkire BC et al (2015) Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health 3:S8–S9. https://doi.org/10.1016/S2214-109X(14)70384-5
Meara JG, Leather AJM, Hagander L et al (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624. https://doi.org/10.1016/S0140-6736(15)60160-X
Truche P, Roa L, Citron I et al (2020) Bellwether procedures for monitoring subnational variation of all-cause perioperative mortality in Brazil. World J Surg 44(10):3299–3309. https://doi.org/10.1007/s00268-020-05607-x
Antoine C, Young BK (2020) Cesarean section one hundred years 1920–2020: the good, the bad and the ugly. J Perinat Med 49(1):5–16. https://doi.org/10.1515/jpm-2020-0305
Biffl WL, Leppaniemi A (2015) Management guidelines for penetrating abdominal trauma. World J of Surg 39(6):1373–1380. https://doi.org/10.1007/s00268-014-2793-7
Sagi HC, Patzakis MJ (2021) Evolution in the acute management of open fracture treatment? Part 1. J Orthop Trauma 35(9):449–456. https://doi.org/10.1097/BOT.0000000000002094
O’Neill KM, Greenberg SL, Cherian M et al (2016) Bellwether procedures for monitoring and planning essential surgical care in low- and middle-income countries: caesarean delivery, laparotomy, and treatment of open fractures. World J Surg 40(11):2611–2619. https://doi.org/10.1007/s00268-016-3614-y
Santos N (2018) 30 Years of SUS: the beginning, the pathway and the target. SUS 30 anos: o início, a caminhada e o rumo. Ciên Saúde Colet 23(6):1729–1736. https://doi.org/10.1590/1413-81232018236.06092018
Moura M, Diego L (2017) Lack of access to surgery: a public health problem. Cad Saúde Pública 33(10):e00151817. https://doi.org/10.1590/0102-311X00151817
Souza Júnior P, Szwarcwald CL, Damacena GN et al (2021) Health insurance coverage in Brazil: analyzing data from the National Health Survey, 2013 and 2019. Ciên Saúde Colet 26(suppl 1):2529–2541. https://doi.org/10.1590/1413-81232021266.1.43532020
Brasil (2021) Estimativas da população residente no Brasil e unidades da federação com data de referência em 1o de julho de 2021. Inst Bras Geogr e Estatística [Internet] (3):1–119. https://ftp.ibge.gov.br/Estimativas_de_Populacao/Estimativas_2021/estimativa_dou_2021.pdf. Accessed 13 July 2022
Massenburg BB, Saluja S, Jenny HE et al (2017) Assessing the Brazilian surgical system with six surgical indicators: a descriptive and modelling study. BMJ Glob Health 2(2):e000226. https://doi.org/10.1136/bmjgh-2016-000226
Alonso N, Massenburg BB, Galli R et al (2017) Surgery in Brazilian health care: funding and physician distribution. Rev Col Bras Cir 44(2):202–207. https://doi.org/10.1590/0100-69912017002016
Bampoe S, Odor PM, Ramani Moonesinghe S et al (2017) A systematic review and overview of health economic evaluations of emergency laparotomy. Perioper Med 6(1):1–12. https://doi.org/10.1186/s13741-017-0078-z
Nally DM, Sorensen J, Kavanagh DO (2020) Emergency laparotomy research methodology: a systematic review. Surgeon 18(2):80–90. https://doi.org/10.1016/j.surge.2019.06.003
Chua M, Chan D (2020) Increased morbidity and mortality of emergency laparotomy in elderly patients. World J Surg 44(3):711–720. https://doi.org/10.1007/s00268-019-05240-3
Giglio PN, Cristante AF, Pécora JR et al (2015) Avanços no tratamento das fraturas expostas. Rev Bras Ortop 50(2):125–130. https://doi.org/10.1016/j.rboe.2015.02.009
Ryan SP, Pugliano V (2014) Controversies in initial management of open fractures. Scand J Surg 103(2):132–137. https://doi.org/10.1177/1457496913519773
Betrán AP, Ye J, Moller AB et al (2016) The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS ONE 11(2):e0148343. https://doi.org/10.1371/journal.pone.0148343
Torloni MR, Brizuela V, Betran AP (2020) Mass media campaigns to reduce unnecessary caesarean sections: a systematic review. BMJ Glob Health 5(2):e001935. https://doi.org/10.1136/bmjgh-2019-001935
Departamento de Informática do SUS/Ministério da Saúde. Razão entre óbitos informados e estimados - F.11 - 2006. Brasília: Ministério da Saúde, 2006. Available in: http://fichas.ripsa.org.br/2006/F-11/?l=en_US. Accessed 25 July 2022
Truche P, Campos LN, Marrazzo EB et al (2021) Association between government policy and delays in emergent and elective surgical care during the COVID-19 pandemic in Brazil: a modeling study. Lancet Reg Health Am 3:100056. https://doi.org/10.1016/j.lana.2021.100056
Funding
All the authors declare that this study has received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MDF holds a voluntary position as National Research Director at InciSioN Brazil, MGF holds a voluntary position with the National Research Team at InciSioN Brazil, JMS holds a voluntary position with the National Research Team at InciSioN Brazil and is a scientific committee member with the Society of Medical Academics of Minas Gerais, CEGM holds a voluntary position with the National Research Team at InciSioN Brazil, JVSL holds a voluntary position with the National Research Team at InciSioN Brazil,
JODH holds a voluntary position with the National Research Team at InciSioN Brazil,
SWV holds a voluntary position as National Chair at InciSioN Brazil.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Faleiro, M.D., Fernandez, M.G., Santos, J.M. et al. Geographical Inequalities in Access to Bellwether Procedures in Brazil. World J Surg 47, 593–599 (2023). https://doi.org/10.1007/s00268-022-06855-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06855-9