Abstract
Background
Laparoscopic pancreaticoduodenectomy (LPD) may induce intense inflammatory response which might be related to the patient’s outcomes. Clinical dexmedetomidine (DEX) has been widely used for opioid-sparing anesthesia and satisfactory sedation. The objective of this study was to investigate the influence of DEX on inflammatory response and postoperative complications in LPD.
Methods
Ninety-nine patients undergoing LPD were randomly assigned to two groups: normal saline (NS) and DEX. The primary outcome was the neutrophil-to-lymphocyte ratio (NLR) differences postoperatively within 48 h. Secondary outcomes were postoperative complications, the length of postoperative hospital stay and the incidence of ICU admission. Other outcomes included anesthetics consumption and intraoperative vital signs.
Results
NLR at postoperative day 2 to baseline ratio decreased significantly in the DEX group (P = 0.032). Less major complications were observed in the DEX group such as pancreatic fistula, delayed gastric emptying and intra-abdominal infection (NS vs. DEX, 21.7% vs. 13.6%, P = 0.315; 10.9% vs. 2.3%, P = 0.226; 17.4% vs. 11.4%, P = 0.416, respectively) though there were no statistical differences. Three patients were transferred to the ICU after surgery in the NS group, while there was none in the DEX group (P = 0.242). The median postoperative hospital stay between groups were similar (P = 0.313). Both intraoperative propofol and opioids were less in the DEX group (P < 0.05).
Conclusions
Intraoperative DEX reduced the early postoperative inflammatory response in LPD. It also reduced the use of narcotics that may related to reduced major complications, which need additional research further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is currently the seventh leading cause of cancer death worldwide and the third leading cause of cancer-related death in the USA [1]. Surgical manipulation is the most effective treatment for these tumors such as carcinoma of pancreatic head, ampulla carcinoma and cholangiocarcinoma [2]. Laparoscopic pancreatoduodenectomy (LPD) is one of the most challenging abdominal operations for pancreatic and periampullary tumors, which involves complex intra-abdominal dissection and reconstruction techniques that may impair patient’s immune function [3, 4]. Growing evidence indicates that immune state and inflammatory responses play a pivotal role in the development of clinically relevant postoperative complications after pancreaticoduodenectomy [5]. A variety of immune cells play their respective roles in the process of inflammation and tumors. The neutrophil-to-lymphocyte ratio (NLR) is usually served as potential surrogate markers of systemic inflammations [6]. It is an inexpensive, widely available parameters that could be used as an indicator to predict the risk of recurrence [7], and prognosis of many types of cancers [8]. Anesthetic agents in the perioperative period could also exert their unique immune and inflammatory regulatory effects and affect the outcomes of surgery [9]. Reasonable anesthesia selection can effectively reduce the level of inflammation and improve prognosis.
Dexmedetomidine (DEX) is a highly selective α2 receptor agonist and has broad pharmacologic effects such as anesthesia, analgesia, sedation, and anxiolysis [10]. It is widely used in the perioperative period and has been widely accepted as an adjunct to general anesthesia, associated with opioid-sparing and organ protective effection. In general, it can attenuate the surgical stress response by inhibiting the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic-adrenal-medullary (SAM) axis, reducing the release of catecholamines and cortisol. Besides, both in vivo and in vitro studies have confirmed that DEX can reduce the levels of inflammatory factors in the circulation, thereby posing an anti-inflammatory shift [11−14]. A single-center, retrospective, cohort study involving 2452 consecutive patients who underwent cardiac surgery showed that perioperative DEX infusion significantly reduced the mortality of postoperative 5-year. Another clinical trial showed that the elderly patients in ICU impacting of DEX increase the 2-year survival rate postoperatively [15]. The application of DEX has also been implied to influence oncological prognosis [16]. Despite the possible beneficial effects of DEX on perioperative patients, its role in pancreatic cancer surgery has not been well established.
As a result of the potential immunomodulation of DEX, we hypothesized that the use of DEX could attenuate the inflammatory response induced by LPD. In parallel, we also investigated the incidence of postoperative complications related.
Methods
Ethics
Ethical approval for this study (Z2017-129–01) was provided by the Ethics Committee of Guangdong Provincal Hospital of Chinese Medicine (Chairperson Professor Jun Liu), Guangzhou, China, on 8 September 2017. This randomized, double-blinded, controlled trial was registered on Chinese Clinical Trial Registry (ChiCTR 1,800,017,065, July 10, 2018) and conducted between 10 July 2018 and 10 January 2022 at the Department of Anaesthesiology of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, China. Written informed consent was obtained from each eligible patient on the day before surgery.
Study design
The inclusion criteria for patients were that they planned to receive LPD, aged 18 to 65 years, body mass index (BMI) <28.0 kg m−2 and American Society of anesthesiologists (ASA) classification: Grade I-III. The exclusion criteria were as follows: severe heart, lung, hepatic or renal diseases; mental disorder; substance abuse; long-term use of sedative hypnotics, antidepressants or other psychotropics; and long-term hormone used and sinus bradycardia.
Anesthesia management and groups
To ensure the randomization of groups, random number was generated by computer and stored in sequentially numbered envelopes. A nurse who did not participate in the trial prepared drug X [DEX or normal saline (NS)] according to the number in the envelope. Only this nurse was aware of patient allocation. General anaesthesia was induced with propofol (TCI 3ug ml−1) and drug X 3 µg kg−1 h−1 infusion for 10 min. Tracheal intubation was faciliated by sufentanil (0.3ug kg−1) and cis-atracurium (0.15 mg kg−1), and then anesthesia was maintained with propofol, cis-atracurium, remifentanil infusion and 1% sevoflurane in oxygen (FiO2 = 0.6). Drug X was continuous infused with 0.3 µg kg−1 h−1 until the surgical specimen resected. Depth of anesthesia was monitored by Nacrotrend-Compact (MT MonitorTechnik GmbH&Co.KG, D-24576 Bad Bramstect) and the index was maintained between 37 and 64. A volume-controlled ventilation mode with a tidal volume of 8 ml kg−1 was performed for eligible patients, and the total flow rate of 2 L·min−1 (FiO2 = 0.6, air/oxygen = 1:1). The partial pressure of end-tidal carbon dioxide (PETCO2) was maintained between 35 and 45 mmHg. Continuous invasive arterial, ECG, blood pressure, oxygen saturation (SpO2), PETCO2 and sevoflurane concentrations were monitored by a IntelliVue MX700 anesthesia monitor (Philips Medical Systems Boeblingen, Netherlands). Before anesthesia induction, by local anesthesia, radial artery was cannulated for invasive arterial monitor and connected to Vigileo/Flotrac system (Edwards Lifesciences, Irvine, CA, USA), and then stroke volume variation (SVV), stroke volume (SV), cardiac output (CO) and cardiac index (CI) were obtained.
Outcome measures
The primary outcome was NLR differences perioperatively. The secondary outcomes were the postoperative complications, the incidence of postoperative ICU admission, and the length of postoperatively hospital stay. Postoperative complications include pancreatic fistula, bile leakage, chylous leakage, postoperative hemorrhage, delayed gastric emptying, and intra-abdominal infection. Major complications include pancreatic fistula Grade B / C [17], delayed gastric emptying Grade B / C [18] and severe intra-abdominal infections [19]. Other outcomes included surgery duration, pneumoperitoneum time, intraoperative fluid volume, urine volume, anesthetic consumptions (propofol, sufentanil and remifentanil) and the intraoperative vital signs (SBP, DBP, MAP, HR, CO, CI and SVV) which were recorded at four times intervals (Baseline; 0.5 h after the beginning of operation; 1 h after the beginning of operation; surgical specimen resected). Laboratory examinations were detected on preoperative (within 72 h before operation), postoperative day (POD) 0, POD1 and POD2, respectively.
Sample size and statistical analysis
According to previous studies [20, 21], optimal cutoff values for high NLR ≥3.0, the difference between groups higher than 10% and a two-sided α level of 0.05 and power (1-β) to 0.8 with 80% power, we calculated that 44 patients in each group were needed. Data were analyzed using statistical product and service solutions 19.0 (SPSS Inc., Chicago, IL, USA). Results for normally distributed data for quantitative variables were expressed as mean ± SD, for non-normal distributed data were expressed as median [IQR] and for qualitative variables as percentage. Student’s t test was used for normally distributed data, and the Mann–Whitney U test was used for nonparametric data. Pearson’s χ2 test or Fisher’s exact test was used to qualitative variables. The generalized estimation equation (GEE) was allowed for analysis of repeated measurements. Repeated measure variables were expressed as estimated marginal mean (EMM) [95% confidence interval (95% CI)] and the working correlation matrix structure was independent structure and the regression model was linear regression model. P <0.05 was considered statistically significant.
Results
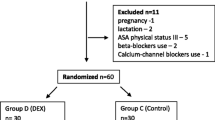
99 patients were enrolled for this trial. 9 patients were excluded because of uncontrollable hemorrhage and conversed to open pancreatoduodenectomy (OPD). 90 patients completed the study (44 in the DEX group and 46 in the NS group) (Fig. 1). Baseline patient characteristics of the trial are shown in Table 1. Preoperative variables were comparable between patients randomized for two groups. Most patients in each group were males, and the median age was 56 years. The ASA classification for all patients was grade II or III. Concomitant diseases such as hypertension and diabetes mellitus were less than 35% in both groups.
Primary outcome
Postoperative NLR in both groups increased to the peak at POD0 and then decreased gradually. In DEX group, the EMM of postoperative NLR was overally lower than that in the NS group [NS vs. DEX, 15.48 (95% CI, 13.22 to 17.75) vs. 13.29 (95% CI, 11.68 to 14.90), P = 0.122], though there were no significant difference between groups. The change of NLR was expressed as ΔNLR (POD NLR to preoperative NLR ratio), compared with the NS group, ΔNLR at POD2 was significantly lower in the DEX group (NS vs. DEX, 4.33 [2.93 to 6.08] vs. 3.87 [2.36 to 4.77], P = 0.032) (Table 2, Fig. 2, H).
Intraoperative vital signs and NLR. Repeated measurements were analyzed by the generalized estimation equation and data are showed as EMM ± SEM. EMM, estimated marginal mean; NS, normal saline; DEX, dexmedetomidine; T1, after intubation; T2, 0.5 h after the beginning of operation; T3, 1 h after the beginning of operation; T4, surgical specimen resected; Pre, preoperative; POD, postoperative day
Secondary outcomes
Approximately 78% patients suffered malignant disease, there was no statistical difference between groups (P = 0.91). Three patients were transferred to the ICU after surgery in the NS group, while there was none in the DEX group (P = 0.242). The overall incidence of major postoperative complications was 54.3% in the NS group and 38.6% in the DEX group; less major complications were observed in the DEX group such as pancreatic fistula, delayed gastric emptying and intra-abdominal infection (NS vs. DEX, 21.7% vs. 13.6%, P = 0.315; 10.9% vs. 2.3%, P = 0.226; 17.4% vs. 11.4%, P = 0.416, respectively) though there were no statistical differences (Table 3).
Other outcomes
Propofol and opioid consumptions were significant less in the DEX group than in the NS group, while the duration of anesthesia was similar between groups (NS vs. DEX, Propofol 1100 [738 to 1405] vs. 760 [528 to 1125]mg, P = 0.004; sufentanil 35 [30 to 40] vs. 30 [26 to 35]ug, P = 0.009; remifentanil 2.15 [1.72 to 2.80] vs. 1.95 [1.51 to 2.00]mg, P = 0.012). There was no significantly difference in surgery duration, pneumoperitoneum time, intraoperative fluid volume, and urine volume (Table 4).
Compared with the NS group, HR and CI were significantly lower in the DEX group [NS vs. DEX, HR, 76 (95% CI, 74 to 79) vs. 71 (95% CI, 68 to 74) bpm, P = 0.007; CI, 3.6 (95% CI, 3.4 to 3.9) vs. 3.3 (95% CI, 3.0 to 3.5) l min−1, P = 0.026]; however, the administration of atropine was similar in both groups [6 (13.0%) vs. 9 (20.5%), P = 0.346]. Also, there were no more patients required vasoconstrictor in the DEX group [NS vs. DEX, 7 (15.9%) vs. 4 (8.7%), P = 0.296]. There was no significantly difference in SBP, DBP, MAP, CO and SVV between groups, though in the DEX group, intraoperative vital signs (except SVV) were slightly lower than those of NS group (Table 4, Fig. 2, A-G).
Discussion
Surgical resection is the mainly possible cure for pancreatic cancer; however, surgery itself induces intense stress response to cause immunosuppression and excessive pro-inflammatory responses, which could promote tumor angiogenesis and increase postoperative complications [22]. The surgical stress impaired cellular immunity that promotes the proliferation of cancer cells, allowing them to escape the surveillance of the immune system and exhibit an outgrowth pattern [23]. Recent studies have indicated that inflammation markers including serum CRP and NLR are independent predictors of disease-free survival, and overall survival after pancreaticoduodenectomy [24]. Compared with OPD, patient undergoing LPD did not reduce the postoperative inflammatory response, though the length of hospital stay maybe shorter [25, 26].
As an inflammatory indicator, NLR indicates the balance between innate and adaptive immune responses and it is an excellent indicator of inflammation and stress together. Neutrophils are a part of the innate immune response, which can exert several pro-tumor activities in cancer and promote progression through different mechanisms [27]. NLR reflecting online dynamic relationship between innate (neutrophils) and adaptive cellular immune response (lymphocytes) can sensitively represent the inflammatory level and predict the cancer prognosis in many kinds of pathological states Therefore, the higher level of NLR was related to the worse outcomes of tumor diseases6. Walsh et al. were the first to apply the parameter for the prognosis of cancer patients undergoing colorectal surgery [28]. The relation between inflammation and prognosis of cancer expressed by NLR has enhanced in various solid tumors in the next nearly fifty years [29−31]. Our results showed that the application of DEX in patients undergoing LPD demonstrates lower changes in NLR postoperatively and levels of NLR at all postoperative time intervals were lower, which similar to the former researches [32]. It is well known that reasonable anesthetic strategy is of importance for the outcomes of patients. Anesthetics are not only release the pain, but also play a critical role in immunomodulatory and tumor metastasis [33]. Different anesthetics play a positive or negative role in host’s immunity, which together maintain an immune balance [34]. DEX is widely used in the perioperative period and plays a beneficial role in resection of a variety of solid cancers [35]. A recent animal experiment confirmed its anti-inflammatory effects and showed a lower tumor burden [36].Clinical researches also shown that application of DEX could reduce serum levels of inflammatory factors in patients receiving carcinoma resection including colon cancer [37], hysterectomy [38], and radical gastrectomy [39]. In addition, immunosuppression attenuated by DEX could also concerned with better outcomes of postoperative cognitive function [40], effective perioperative analgesia, less use of opioids [41]. Contrary to DEX, opioids are recognized as suppressing immunity and promoting cancer proliferation, result in potential narcotic dependence, respiratory depression, and gastrointestinal dysfunctions [42]. Recent reports suggested that the use of narcotics for perioperative analgesia can cause Oddi sphincter contraction, which maybe increase intrapancreatic pressure and lead to postoperative pancreatic fistula (POPF) [43]. We found that intraoperative DEX dramatically decreased the consumption of propofol and narcotics, since the POPF often lead to catastrophic consequences [44], the minimize of opioids by DEX gave the strong excuse for exquisite further study. Intra-abdominal infection with acute physiology and chronic health evaluation II (APACHE II) ≥10, sepsis, or acute gastrointestinal injury (AGI) grade ≥ III was defined as severe intra-abdominal infection [45]. Among mechanically ventilated patients with sepsis, sedation with DEX resulted in reduced inflammatory response and increased lactate clearance [46, 47]. Intraoperative DEX reduced the time to first flatus, first oral feeding, and first defecation [48].These results showed that this treatment may be a feasible strategy for improving postoperative gastrointestinal function recovery in patients undergoing laparoscopic operation. With agreement, our results showed that the incidences of major postoperative complications including POPF, delayed gastric emptying and severe intra-abdominal infection were reduced in the DEX group though there were no statistical significance, which means further research is urgently needed.
Limitations
There are several limitations in this study. Firstly, the inflammatory indicators we examined were relatively single, and there may be differences in other immune cells and cytokines. Furthermore, long-term indicators are important for cancer prognosis, and we only collect short-term outcome indicators and pay more attention to the immune-related situation, did not follow up after discharge from the hospital. Secondly, patients undergoing LPD include different types of periampullary carcinomas, and the bias caused by cancer type cannot be completely ruled out, although the distribution of tumor types in two groups was similar. Thirdly, we only collected and measured samples every 24 h after surgery. For the lack of detection within 24 h after surgery, the dynamic changes of inflammatory factors and immune cells may not be observed in time.
Conclusions
In summary, the use of DEX in LPD patients may attenuate the early postoperative inflammatory response and be associated with reducing the consumption of propofol and opioids. Less major postoperative complications such as pancreatic fistula, delayed gastric emptying and intra-abdominal infection were observed in the DEX group though there were no statistical differences, additional research is urgently needed to clarify the proper anesthetic strategy for LPD.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Wang M, Peng B, Liu J et al (2021) Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: a retrospective multicenter analysis of 1029 patients. Ann Surg 273:145–153
Tung S, Davis LE, Hallet J et al (2019) Population-level symptom assessment following pancreaticoduodenectomy for adenocarcinoma. JAMA Surg 154:e193348
Nickel F, Haney CM, Kowalewski KF et al (2020) Laparoscopic versus open pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 271:54–66
Sun S, He C, Wang J, Huang X, Wu J, Li S (2020) The prognostic significance of inflammation-based scores in patients with ampullary carcinoma after pancreaticoduodenectomy. BMC Cancer 20:981
Zahorec R (2021) Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy 122:474–488
Miura T, Ohtsuka H, Aoki T et al (2021) Increased neutrophil-lymphocyte ratio predicts recurrence in patients with well-differentiated pancreatic neuroendocrine neoplasm based on the 2017 World Health Organization classification. BMC Surg 21:176
Murthy P, Zenati MS, Al Abbas AI et al (2020) Prognostic value of the systemic Immune-Inflammation Index (SII) after neoadjuvant therapy for patients with resected pancreatic cancer. Ann Surg Oncol 27:898–906
Wall T, Sherwin A, Ma D, Buggy DJ (2019) Influence of perioperative anaesthetic and analgesic interventions on oncological outcomes: a narrative review. Br J Anaesth 123:135–150
Liu X, Li Y, Kang L, Wang Q (2021) Recent advances in the clinical value and potential of dexmedetomidine. J Inflamm Res 14:7507–7527
Yuki K (2021) The immunomodulatory mechanism of dexmedetomidine. Int Immunopharmacol 97:107709
Wang K, Wu M, Xu J et al (2019) Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: systematic review and meta-analysis. Br J Anaesth 123:777–794
Zhang Y, Liu M, Yang Y, Cao J, Mi W (2020) Dexmedetomidine exerts a protective effect on ischemia-reperfusion injury after hepatectomy: a prospective, randomized, controlled study. J Clin Anesth 61:109631
Huang DY, Li Q, Shi CY, Hou CQ, Miao Y, Shen HB (2020) Dexmedetomidine attenuates inflammation and pancreatic injury in a rat model of experimental severe acute pancreatitis via cholinergic anti-inflammatory pathway. Chin Med J (Engl) 133:1073–1079
Zhang DF, Su X, Meng ZT et al (2019) Impact of dexmedetomidine on long-term outcomes after noncardiac surgery in elderly: 3-year follow-up of a randomized controlled trial. Ann Surg 270:356–363
Cai Q, Liu G, Huang L et al (2022) The role of dexmedetomidine in tumor-progressive factors in the perioperative period and cancer recurrence: a narrative review. Drug Des Devel Ther 16:2161–2175
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591
Wente MN, Bassi C, Dervenis C et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the international study group of pancreatic surgery (ISGPS). Surgery 142:761–768
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Goh BK, Chok AY, Allen JC Jr et al (2016) Blood neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are independent prognostic factors for surgically resected gastrointestinal stromal tumors. Surgery 159:1146–1156
Guo J, Fang J, Huang X et al (2018) Prognostic role of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in prostate cancer: a meta-analysis of results from multivariate analysis. Int J Surg 60:216–223
Saito R, Kawaida H, Hosomura N et al (2021) Exposure to blood components and inflammation contribute to pancreatic cancer progression. Ann Surg Oncol 28:8263–8272
Tang F, Tie Y, Tu C, Wei X (2020) Surgical trauma-induced immunosuppression in cancer: recent advances and the potential therapies. Clin Transl Med 10:199–223
Taniai T, Haruki K, Furukawa K et al (2021) The novel index using preoperative C-reactive protein and neutrophil-to-lymphocyte ratio predicts poor prognosis in patients with pancreatic cancer. Int J Clin Oncol 26:1922–1928
van Hilst J, Brinkman DJ, de Rooij T et al (2019) The inflammatory response after laparoscopic and open pancreatoduodenectomy and the association with complications in a multicenter randomized controlled trial. HPB (Oxford) 21:1453–1461
Wang M, Li D, Chen R et al (2021) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 6:438–447
Poto R, Cristinziano L, Modestino L et al (2022) Neutrophil extracellular traps, angiogenesis and cancer. Biomedicines 10(2):431
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ (2013) The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol 88:218–230
Pichler M, Hutterer GC, Stoeckigt C et al (2013) Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer 108:901–907
Ohno Y, Nakashima J, Ohori M, Hatano T, Tachibana M (2010) Pretreatment neutrophil-to-lymphocyte ratio as an independent predictor of recurrence in patients with nonmetastatic renal cell carcinoma. J Urol 184:873–878
He C, Zhang Y, Cai Z, Lin X (2019) The prognostic and predictive value of the combination of the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio in patients with hepatocellular carcinoma who receive transarterial chemoembolization therapy. Cancer Manag Res 11:1391–1400
Ackerman RS, Luddy KA, Icard BE, Piñeiro Fernández J, Gatenby RA, Muncey AR (2021) The effects of anesthetics and perioperative medications on immune function: a narrative review. Anesth Analg 133:676–689
Kim R (2018) Effects of surgery and anesthetic choice on immunosuppression and cancer recurrence. J Transl Med 16:8
Cheng M, Shi J, Gao T et al (2017) The addition of dexmedetomidine to analgesia for patients after abdominal operations: a prospective randomized clinical trial. World J Surg 41:39–46
Shin S, Kim KJ, Hwang HJ, Noh S, Oh JE, Yoo YC (2021) Immunomodulatory effects of perioperative dexmedetomidine in ovarian cancer: an in vitro and xenograft mouse model study. Front Oncol 11:722743
Wang K, Li C (2018) Effects of dexmedetomidine on inflammatory factors, T lymphocyte subsets and expression of NF-κB in peripheral blood mononuclear cells in patients receiving radical surgery of colon carcinoma. Oncol Lett 15:7153–7157
Xu S, Hu S, Ju X, Li Y, Li Q, Wang S (2021) Effects of intravenous lidocaine, dexmedetomidine, and their combination on IL-1, IL-6 and TNF-α in patients undergoing laparoscopic hysterectomy: a prospective, randomized controlled trial. BMC Anesthesiol 21:3
Zheng L, Zhao J, Zheng L, Jing S, Wang X (2020) Effect of dexmedetomidine on perioperative stress response and immune function in patients with tumors. Technol Cancer Res Treat 19:1533033820977542
Wang Z, Shen Z, Wang H, Zhang L, Dong R (2020) Effect of dexmedetomidine on the cognitive function of patients undergoing gastric cancer surgery by regulating the PI3K/AKT signaling pathway. Oncol Lett 19:1151–1156
Cho JS, Seon K, Kim MY, Kim SW, Yoo YC (2021) Effects of perioperative dexmedetomidine on immunomodulation in uterine cancer surgery: a randomized. Controlled Trial Front Oncol 11:749003
Salome A, Harkouk H, Fletcher D, Martinez V (2021) Opioid-free anesthesia Benefit-risk balance: a systematic review and Meta-analysis of randomized controlled trials. J Clin Med 10(10):20
Jiang L, Ning D, Chen X (2020) Prevention and treatment of pancreatic fistula after pancreatic body and tail resection: current status and future directions. Front Med 14:251–261
Li B, Pu N, Chen Q et al (2021) Comprehensive diagnostic nomogram for predicting clinically relevant postoperative pancreatic fistula after pancreatoduodenectomy. Front Oncol 11:717087
Mazuski JE, Tessier JM, May AK et al (2017) The surgical infection society revised guidelines on the management of Intra-abdominal infection. Surg Infect 18:1–76
Miyamoto K, Nakashima T, Shima N et al (2018) Effect of dexmedetomidine on lactate clearance in patients with septic shock: a subanalysis of a multicenter randomized controlled trial. Shock 50:162–166
Ohta Y, Miyamoto K, Kawazoe Y, Yamamura H, Morimoto T (2020) Effect of dexmedetomidine on inflammation in patients with sepsis requiring mechanical ventilation: a sub-analysis of a multicenter randomized clinical trial. Crit Care 24:493
Wu Y, Cai Z, Liu L et al (2022) Impact of intravenous dexmedetomidine on gastrointestinal function recovery after laparoscopic hysteromyomectomy: a randomized clinical trial. Sci Rep 12:14640
Funding
The Guangzhou Municipal Science and Technology Project, China (Grant No.202102010243).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict on interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval for this study (Z2017-129–01) was provided by the Ethics Committee of Guangdong Provincal Hospital of Chinese Medicine (Chairperson Professor Jun Liu), Guangzhou, China, on 8 September 2017.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, YX., Du, L., Wang, LN. et al. Effects of Dexmedetomidine on Systemic Inflammation and Postoperative Complications in Laparoscopic Pancreaticoduodenectomy: A Double-blind Randomized Controlled Trial. World J Surg 47, 500–509 (2023). https://doi.org/10.1007/s00268-022-06802-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06802-8