Abstract
Background
Trauma scoring systems can identify patients who should be transferred to referral hospitals, but their utility in LMICs is often limited. The Malawi Trauma Score (MTS) reliably predicts mortality at referral hospitals but has not been studied at district hospitals. We sought to validate the MTS at a Malawi district hospital and evaluate whether MTS is predictive of transfer to a referral hospital.
Methods
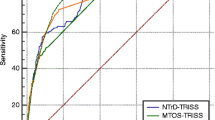
We performed a retrospective study using trauma registry data from Salima District Hospital (SDH) from 2017 to 2021. We excluded patients brought in dead, discharged from the Casualty Department, or missing data needed to calculate MTS. We used logistic regression modeling to study the relationship between MTS and mortality at SDH and between MTS and transfer to a referral hospital. We used receiver operating characteristic analysis to validate the MTS as a predictor of mortality.
Results
We included 2196 patients (84.3% discharged, 12.7% transferred, 3.0% died). These groups had similar ages, sex, and admission vitals. Mean (SD) MTS was 7.9(3.0) among discharged patients, 8.4(3.9) among transferred patients, and 14.2(8.0) among patients who died (p < 0.001). Higher MTS was associated with increased odds of mortality at SDH (OR 1.21, 95% CI 1.14–1.29, p < 0.001) but was not related to transfer. ROC area for mortality was 0.73 (95% CI 0.65–0.80).
Conclusions
MTS is predictive of district hospital mortality but not inter-facility transfer. We suggest that MTS be used to identify patients with severe trauma who are most likely to benefit from transfer to a referral hospital.





Similar content being viewed by others
References
World Health Organization. Injuries and Violence. Published 2021. Accessed May 13, 2022. https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence
Beard JH, Ohene-Yeboah M, deVries CR, Schecter WP (2015) Hernia and Hydrocele. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds) Disease control priorities, third edition (Volume 1): essential surgery. The World Bank, pp 151–171. https://doi.org/10.1596/978-1-4648-0346-8_ch9
Mock C, Joshipura M, Arreola-Risa C, Quansah R (2012) An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg 36(5):959–963. https://doi.org/10.1007/s00268-012-1459-6
Alharbi RJ, Shrestha S, Lewis V, Miller C (2021) The effectiveness of trauma care systems at different stages of development in reducing mortality: a systematic review and meta-analysis. World J Emerg Surg 16(1):1–13. https://doi.org/10.1186/s13017-021-00381-0
Adzemovic T, Murray T, Jenkins P et al (2019) Should they stay or should they go? Who benefits from interfacility transfer to a higher-level trauma center following initial presentation at a lower-level trauma center. J Trauma Acute Care Surg 86(6):952–960. https://doi.org/10.1097/TA.0000000000002248
Davis JW, Dirks RC, Sue LP, Kaups KL (2017) Attempting to validate the overtriage/undertriage matrix at a level I trauma center. J Trauma Acute Care Surg 83(6):1173–1178. https://doi.org/10.1097/TA.0000000000001623
Maine RG, Kajombo C, Mulima G et al (2020) Secondary overtriage of trauma patients to a central hospital in Malawi. World J Surg 44(6):1727–1735. https://doi.org/10.1007/s00268-020-05426-0
Gomez D, Alali AS, Xiong W, Zarzaur BL, Mann NC, Nathens AB (2015) Definitive care in level 3 trauma centres after severe injury: a comparison of clinical characteristics and outcomes. Injury 46(9):1790–1795. https://doi.org/10.1016/j.injury.2015.05.047
Feldhaus I, Carvalho M, Waiz G et al (2020) Thefeasibility, appropriateness, and applicability of trauma scoring systems in low and middle-income countries: a systematic review. Trauma Surg Acute Care Open 5(1):1–8. https://doi.org/10.1136/tsaco-2019-000424
Gallaher J, Jefferson M, Varela C, Maine R, Cairns B, Charles A (2019) The Malawi trauma score: a model for predicting trauma-associated mortality in a resource-poor setting. Injury 50(9):1552–1557. https://doi.org/10.1016/j.injury.2019.07.004
Haac B, Varela C, Geyer A, Cairns B, Charles A (2015) The utility of the Kampala trauma score as a triage tool in a sub-Saharan African trauma cohort. World J Surg 39(2):356–362. https://doi.org/10.1007/s00268-014-2830-6
Gallaher JR, Chise Y, Reiss R, Purcell LN, Manjolo M, Charles A (2020) Underutilization of operative capacity at the district hospital level in a resource-limited setting. J Surg Res 2021(259):130–136. https://doi.org/10.1016/j.jss.2020.11.031
Hung YW, He H, Mehmood A et al (2017) Exploring injury severity measures and in-hospital mortality: a multi-hospital study in Kenya. Injury 48(10):2112–2118. https://doi.org/10.1016/j.injury.2017.07.001
Chardoli M, Rahimi-Movaghar V (2006) Analysis of trauma outcome at a university hospital in zahedan, iran using the TRISS method. East Afr Med J 83(8):440–442
MacLeod JBA, Kobusingye O, Frost C, Lett R, Kirya F, Shulman C (2003) A comparison of the kampala trauma score (KTS) with the revised trauma score (RTS), injury severity score (ISS), and the TRISS method in a ugandan trauma registry: is equal performance achieved with fewer resources? Eur J Trauma 29(6):392–398. https://doi.org/10.1007/s00068-003-1277-5
Tignanelli CJ, Vander Kolk WE, Mikhail JN, Delano MJ, Hemmila MR (2018) Noncompliance with American college of surgeons committee on trauma recommended criteria for full trauma team activation is associated with undertriage deaths. J Trauma Acute Care Surg 84(2):287–294. https://doi.org/10.1097/TA.0000000000001745
Yohann A, Kratzke I, Williams B, Charles A (2022) The effect of transfer status on trauma outcomes in low- and middle-income countries: a systematic review and meta-analysis. Injury 53(3):885–894. https://doi.org/10.1016/j.injury.2021.10.010
Pouramin P, Li CS, Busse JW et al (2020) Delays in hospital admissions in patients with fractures across 18 low-income and middle-income countries (INORMUS): a prospective observational study. Lancet Glob Heal 8(5):e711–e720. https://doi.org/10.1016/S2214-109X(20)30067-X
Reynolds TA, Sawe H, Rubiano AM, Shin SD, Wallis L, Mock CN (2017) Strengthening health systems to provide emergency care. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R (eds) Disease control priorities, third edition (Volume 9): improving health and reducing poverty. The World Bank, pp 247–265. https://doi.org/10.1596/978-1-4648-0527-1_ch13
American College of Surgeons Committee on Trauma. Resources for Optimal Care of the Injured Patient.; https://doi.org/10.1097/00043860-200007000-00002
Stewart BT (2018) Commentary on ‘a consensus-based criterion standard for the requirement of a trauma team:’ low-resource setting considerations. World J Surg 42(9):2810–2812. https://doi.org/10.1007/s00268-018-4616-8
Jenson A, Hansoti B, Rothman R, De Ramirez SS, Lobner K, Wallis L (2018) Reliability and validity of emergency department triage tools in low- and middle-income countries: a systematic review. Eur J Emerg Med 25(3):154–160. https://doi.org/10.1097/MEJ.0000000000000445
Mullan PC, Torrey SB, Chandra A, Caruso N, Kestler A (2014) Reduced overtriage and undertriage with a new triage system in an urban accident and emergency department in Botswana: a cohort study. Emerg Med J 31(5):356–360. https://doi.org/10.1136/emermed-2012-201900
Nkurunziza T, Toma G, Odhiambo J et al (2016) Referral patterns and predictors of referral delays for patients with traumatic injuries in rural Rwanda. Surg (United States) 160(6):1636–1644. https://doi.org/10.1016/j.surg.2016.08.006
Nakahara S, Saint S, Sann S et al (2010) Exploring referral systems for injured patients in low-income countries: a case study from Cambodia. Health Policy Plan 25(4):319–327. https://doi.org/10.1093/heapol/czp063
Palmer C (2007) Major trauma and the injury severity score - where should we set the bar? Assoc Adv Automot Med 51:13–29
Boyd CR, Tolson MA, Copes WS (1987) Evaluating trauma care: the TRISS method. J Trauma - Inj Infect Crit Care 27(4):370–378. https://doi.org/10.1097/00005373-198704000-00005
Acknowledgements
This study was supported by the NIH Fogarty International Center (Grant #D43TW009340).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest to declare.
Study Approval
This study was approved by the University of North Carolina Institutional Review Board and the Malawi National Health Sciences Research Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yohann, A., Chise, Y., Manjolo, C. et al. Malawi Trauma Score is Predictive of Mortality at a District Hospital: A Validation Study. World J Surg 47, 78–85 (2023). https://doi.org/10.1007/s00268-022-06791-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06791-8