Abstract
Background
The pediatric resuscitation and trauma outcome (PRESTO) model was developed to aid comparisons of risk-adjusted mortality after injury in low- and middle-income countries (LMICs). We sought to validate PRESTO using data from a middle-income country (MIC) trauma registry and compare its performance to the Pediatric Trauma Score (PTS), Revised Trauma Score, and pediatric age-adjusted shock index (SIPA).
Methods
We included children (age < 15 years) admitted to a single trauma center in South Africa from December 2012 to January 2019. We excluded patients missing variables necessary for the PRESTO model—age, systolic blood pressure, pulse, oxygen saturation, neurologic status, and airway support. Trauma scores were assigned retrospectively. PRESTO’s previously high-income country (HIC)-validated optimal threshold was compared to MIC-validated threshold using area under the receiver operating characteristic curves (AUROC). Prediction of in-hospital death using trauma scoring systems was compared using ROC analysis.
Results
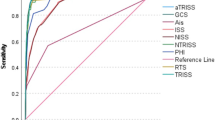
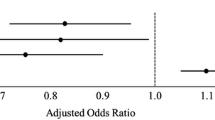
Of 1160 injured children, 988 (85%) had complete data for calculation of PRESTO. Median age was 7 (IQR: 4, 11), and 67% were male. Mortality was 2% (n = 23). Mean predicted mortality was 0.5% (range 0–25.7%, AUROC 0.93). Using the HIC-validated threshold, PRESTO had a sensitivity of 26.1% and a specificity of 99.7%. The MIC threshold showed a sensitivity of 82.6% and specificity of 89.4%. The MIC threshold yielded superior discrimination (AUROC 0.86 [CI 0.78, 0.94]) compared to the previously established HIC threshold (0.63 [CI 0.54, 0.72], p < 0.0001). PRESTO showed superior prediction of in-hospital death compared to PTS and SIPA (all p < 0.01).
Conclusion
PRESTO can be applied in MIC settings and discriminates between children at risk for in-hospital death following trauma. Further research should clarify optimal decision thresholds for quality improvement and benchmarking in LMIC settings.



Similar content being viewed by others
References
(2018) Children: reducing mortality. In: WHO | fact sheets. https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality. Accessed 30 Jul 2019
World Health Organization, Geneva (2018) Global health estimates 2016 summary tables: global deaths by cause, age and sex, 2000–2016. In: WHO | Disease burden and mortality estimates. http://www.who.int/healthinfo/global_burden_disease/estimates/en/. Accessed 30 Jul 2019
Bickler SW, Rode H (2002) Surgical services for children in developing countries. Bull World Health Organ 80:829–835. https://doi.org/10.1590/S0042-96862002001000013
Peden M, Oyegbite K, Ozanne-Smith J et al (2009) World report on child injury prevention. World Health Organization, Geneva
Callese TE, Richards CT, Shaw P et al (2015) Trauma system development in low- and middle-income countries: a review. J Surg Res 193:300–307. https://doi.org/10.1016/j.jss.2014.09.040
Reynolds TA, Stewart B, Drewett I et al (2017) The impact of trauma care systems in low- and middle-income countries. Annu Rev Public Health 38:507–532. https://doi.org/10.1146/annurev-publhealth-032315-021412
Laing GL, Bruce JL, Aldous C, Clarke DL (2014) The design, construction and implementation of a computerised trauma registry in a developing South African metropolitan trauma service. Injury 45:3–8. https://doi.org/10.1016/j.injury.2013.05.013
Schuurman N, Cinnamon J, Matzopoulos R et al (2011) Collecting injury surveillance data in low- and middle-income countries: the Cape Town Trauma Registry pilot. Glob Public Health 6:874–889. https://doi.org/10.1080/17441692.2010.516268
Stevens KA, Paruk F, Bachani AM et al (2013) Establishing hospital-based trauma registry systems: lessons from Kenya. Injury 44(Suppl 4):S70–S74. https://doi.org/10.1016/S0020-1383(13)70216-X
O’Reilly GM, Joshipura M, Cameron PA, Gruen R (2013) Trauma registries in developing countries: a review of the published experience. Injury 44:713–721. https://doi.org/10.1016/j.injury.2013.02.003
Traynor MD, Hernandez MC, Shariq O et al (2019) Trauma registry data as a tool for comparison of practice patterns and outcomes between low- and middle-income and high-income healthcare settings. Pediatr Surg Int 35:699–708. https://doi.org/10.1007/s00383-019-04453-w
St-Louis E, Bracco D, Hanley J et al (2018) Development and validation of a new pediatric resuscitation and trauma outcome (PRESTO) model using the U.S. National Trauma Data Bank. J Pediatr Surg 53:136–140. https://doi.org/10.1016/j.jpedsurg.2017.10.039
Brown JB, Gestring ML, Leeper CM et al (2017) The value of the injury severity score in pediatric trauma: time for a new definition of severe injury? J Trauma Acute Care Surg 82:995–1001. https://doi.org/10.1097/TA.0000000000001440
Haac B, Varela C, Geyer A et al (2015) The utility of the Kampala trauma score as a triage tool in a Sub-Saharan African Trauma Cohort. World J Surg 39:356–362. https://doi.org/10.1007/s00268-014-2830-6
Acker SN, Ross JT, Partrick DA et al (2015) Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg 50:331–334. https://doi.org/10.1016/j.jpedsurg.2014.08.009
Tepas JJI, Ramenofsky ML, Mollitt DL et al (1988) The pediatric trauma score as a predictor of injury severity: an objective assessment. J Trauma Acute Care Surg 28:425
Champion HR, Sacco WJ, Copes WS et al (1989) A revision of the Trauma Score. J Trauma 29:623–629. https://doi.org/10.1097/00005373-198905000-00017
Eichelberger MR, Gotschall CS, Sacco WJ et al (1989) A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann Emerg Med 18:1053–1058. https://doi.org/10.1016/S0196-0644(89)80930-8
Donovan MM, Kong VY, Bruce JL et al (2019) The hybrid electronic medical registry allows benchmarking of quality of trauma care: a five-year temporal overview of the trauma burden at a Major Trauma Centre in South Africa. World J Surg 43:1014–1021. https://doi.org/10.1007/s00268-018-04880-1
Kleinman ME, Chameides L, Schexnayder SM et al (2010) Part 14: Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.110.971101
Luscombe MD, Owens BD, Burke D (2011) Weight estimation in paediatrics: a comparison of the APLS formula and the formula “Weight = 3(age) + 7”. Emerg Med J 28:590–593. https://doi.org/10.1136/emj.2009.087288
Nordin A, Coleman A, Shi J et al (2017) Validation of the age-adjusted shock index using pediatric trauma quality improvement program data. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2017.10.023
Traynor MD, Hernandez MC, Clarke DL et al (2019) Utilization of age-adjusted shock index in a resource strained setting. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2019.08.021
Roy N, Gerdin M, Schneider E et al (2016) Validation of international trauma scoring systems in urban trauma centres in India. Injury 47:2459–2464. https://doi.org/10.1016/j.injury.2016.09.027
Hung YW, He H, Mehmood A et al (2017) Exploring injury severity measures and in-hospital mortality: a multi-hospital study in Kenya. Injury 48:2112–2118. https://doi.org/10.1016/j.injury.2017.07.001
St-Louis E, Hassamal R, Razek T et al (2019) Validation of the PRESTO score in injured children in a South-African Quaternary Trauma Center. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2019.08.008
Nielsen JW, Shi J, Wheeler K et al (2016) Resource use in pediatric blunt and penetrating trauma. J Surg Res 202:436–442. https://doi.org/10.1016/j.jss.2015.06.018
Weeks SR, Juillard CJ, Monono ME et al (2014) Is the Kampala trauma score an effective predictor of mortality in low-resource settings? A comparison of multiple trauma severity scores. World J Surg 38:1905–1911. https://doi.org/10.1007/s00268-014-2496-0
Kobusingye OC, Lett RR (2000) Hospital-based trauma registries in Uganda. J Trauma 48:498–502. https://doi.org/10.1097/00005373-200003000-00022
Young S, Leodoro B, Toukune A et al (2019) Patient-reported barriers to accessing surgical care in Northern Vanuatu. World J Surg 43:2979–2985. https://doi.org/10.1007/s00268-019-05146-0
Burstein B, Fauteux-Lamarre E, van As AB (2016) Increased morbidity associated with weekend paediatric road traffic injuries: 10-year analysis of trauma registry data. Injury 47:1236–1241. https://doi.org/10.1016/j.injury.2016.02.021
Haider AH, Hashmi ZG, Gupta S et al (2014) Benchmarking of trauma care worldwide: the potential value of an International Trauma Data Bank (ITDB). World J Surg 38:1882–1891. https://doi.org/10.1007/s00268-014-2629-5
Acknowledgements
We would like to thank Antinea Ascione for proofreading the final copy of this manuscript.
Author information
Authors and Affiliations
Contributions
MDT, ESL, DLC: concept and study design were contributed; MDT, JLB, GLL, DLC: data collection and preparation were contributed; MDT: analysis was contributed; MDT: manuscript preparation was contributed; ESL, MCH, ASA, RB, DP, VYK, DBK, CRM, MDZ, DLC: critical revision was contributed.
Corresponding author
Ethics declarations
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflicts of interest regarding this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Traynor, M.D., St. Louis, E., Hernandez, M.C. et al. Comparison of the Pediatric Resuscitation and Trauma Outcome (PRESTO) Model and Pediatric Trauma Scoring Systems in a Middle-Income Country. World J Surg 44, 2518–2525 (2020). https://doi.org/10.1007/s00268-020-05512-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05512-3