Abstract
Background
Open mesh repair of incisional hernia is associated with different local complications, particularly bleeding and seroma formation. Traditionally, drains have been placed perioperatively to prevent these complications, despite the lack of scientific evidence or expert consensus. We formulated the hypothesis that the absence of drainage would reduce number of patients presenting collections or complications. The present study aimed to compare postoperative complication rates after open mesh repair for incisional hernia with or without prophylactic wound drainage.
Methods
Prospective randomized study using standardized surgical technique and drain placement. The primary endpoint was the evaluation of residual fluid collection with ultrasound on postoperative day 30. Other complications, subdivided into medical and surgical, were analyzed as secondary endpoints.
Results
There were 144 patients randomized (70 with drain, 74 without drain). No difference was identified between both groups for fluid collection at 30 days (60.3% vs. 62%, p = 0.844). However, less surgical complications were identified in the drain group (21.7% vs. 42.7%, p = 0.007), with a lower wound dehiscence rate (1.5% vs. 9.3%, p = 0.041).
Conclusions
Prophylactic drainage in open incisional hernia repair does not objectively reduce the rate of postoperative fluid collections. Therefore, our results do not support the use of routine drainage in incisional hernia repair.
Trial registration
Trial registration on clinicaltrials.gov (NCT00478348).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Incisional hernia formation presents a major burden of care after open abdominal surgery. It may occur in up to 20% of patients after median laparotomy [1,2,3,4] and the risk factors have been well described [3, 5]. It is estimated that approximately 100,000 incisional hernia repairs are performed annually in the United States [2, 3, 6]. In Europe, approximately 3900 incisional hernia repairs are performed each year in Netherland and 1800 were performed in Denmark between 2007 and 2008 [7, 8].
The most common complications after open mesh incisional hernia repairs are surgical site infections and collections [4, 9]. Drains are commonly used to decrease the occurrence of postoperative fluid collections in the surgical field even though the exact etiology of seroma formation remains controversial. Klink et al. reported that the nature of the fluid collection could predict the subsequent development of a seroma [10]. Whether or not drains have an influence on the formation of fluid collections is an ongoing debate and experts have not yet reached a consensus. Some authors suggest that wound infections are more frequent and that complications are not reduced with the use of drains [11], while others argue that even if drains don’t prevent infections, they may be beneficial [12]. In 2017, the Australian Supreme Court debated this subject and ruled that standard management requires the placement of a drain in complex cases [13]. A survey among members of the Australian Society of General Surgery regarding the placement of drains in incisional hernia repair outlined a variety of practices and beliefs [14]. This result was confirmed by a retrospective audit which concluded that drains were placed in only a minor proportion of cases [15].
Indeed there are few prospective studies comparing outcomes with and without drains after incisional hernia repair [16, 17]. In 2015, a Brazilian group prospectively compared drains and quilting sutures in incisional hernia repair and found similar rates of seroma and surgical wound infections [18].
We formulated the hypothesis that the absence of drainage would not influence the number of patients presenting collections or complications after incisional hernia repair. This current prospective, randomized controlled trial aimed to determine the influence of prophylactic drainage in incisional hernia repair on postoperative fluid collections and complications.
Material and methods
Compliance with ethical standards
This prospective randomized multicentric study was conducted according to the CONSORT statement guidelines [19]. The study was approved by the local ethic committee (CER-VD 31/07, DP-2007-CHV-UNIL) and was registered as a prospective randomized clinical trial on clinicaltrials.gov (NCT00478348).
Patients
Patients were screened preoperatively at the outpatient clinic of the Department of visceral surgery, Lausanne University Hospital CHUV. Inclusion criteria were patients between 20 and 80 years old requiring an elective open incisional hernia repair with a physical status classification according to the American Society of Anesthesiologists (ASA) between 1 and 3. Exclusion criteria were a hernia defect of less than 2 cm, inguinal hernia, ongoing antibiotic treatment before admission, and emergency surgery for an incarcerated or strangulated hernia. In addition, we excluded laparoscopic hernia procedures and patients under immunosuppressive therapy.
All included patients completed an informed consent form validated by the local ethics committee.
Sample size calculation
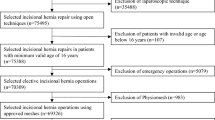
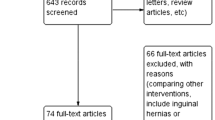
The complication rate in the drainage group was estimated to reach 20%. No prospective study comparing drainage and without drainage was available in the literature when the study was started. Rates of complications were estimated according to a consensus between surgeons participating to the study. We hypothesized that the absence of drainage would decrease the occurrence of either surgical site infection, seroma, hematoma, or early hernia recurrence by 50% within 30 days after surgery. The sample size was calculated with an 80% power; and a significance level with a p-value under 0.05 was established. The sample size calculation according to power yielded 398 patients. Approximately 60 patients per year present an incisional hernia requiring surgery. With a participation rate of 80% among eligible patients, the study was estimated to last over 8 years. A second hospital was included to reduce the study duration. The study was however prematurely interrupted due to the emergence of concurrent minimally invasive techniques and the number of 398 patients was not reached. Despite laparoscopic intraperitoneal onlay mesh (IPOM) technique has been known for more than 20 years, the penetration and adoption of this technique required some time to be achieved in our teaching department. However, laparoscopic IPOM techniques have become very popular during the study period and compete with our recruitment.
Surgical techniques and randomization
Patients were electronically randomized on the day before surgery. They were allocated to the treatment group (with drainage) or the control group (without drainage). A clinical nurse performed the randomization through a web-based service (https://www.randomizer.at—Institute for Medical Informatics Statistics and Documentation, Medical University of Graz, Austria).
This study was not blinded due to technical limitations. Indeed, it would have been difficult to blind the operators placing a drain and to blind the patients due to the presence of dressings and drain bottles.
The surgical technique was standardized in both groups. All patients underwent an open repair according to the Rives-Stoppa procedure [20]. This procedure consists of the placement and fixation of a mesh in the retromuscular position after dissection and reduction of the hernial sac and closure of the posterior sheath. The closure of the anterior sheath with or without relaxing incisions allows for closure above the mesh. Mesh type choice was at the discretion of the surgeon. Redon drains (10 French, closed active-suction drainage) were placed in the retromuscular and preaponeurotic (subcutaneous) planes. In the drainage group, drains were removed sequentially when the output was <30 ml/day. This volume was defined by a consensus between surgeons participating to the study because no data exist in the literature about volume or duration of drainage.
Endpoints
The endpoints were registered during a follow up period of thirty days. The primary endpoint was the presence of a fluid collection on postoperative day 30 (POD 30). All patients underwent an ultrasound to objectively assess the presence or absence of a collection. Collections were subdivided into seroma, hematoma and abscess. Seroma was defined as a subcutaneous fluid collection without a solid component. The hematoma was characterized by the presence of debris, and abscess was confirmed by the presence of pus on a puncture.
Secondary endpoints were complications, classified according to Clavien-Dindo classification [21] and Comprehensive Complication Index (CCI) [22]. Complications were pre-defined when the study was elaborated and more than one complication was registered per patient in order to calculate Clavien-Dindo score but also the CCI. These complications were also subdivided in a second time into surgical versus medical complications. Surgical complications included early recurrence, surgical site infection classified according to Center for Disease Control and Prevention (CDC) criteria [23], evisceration, wound dehiscence, or ileus. Medical complications such as cardiac arrhythmia or ischemia, pneumonia, pulmonary edema, thromboembolic events, urinary tract infections or obstructions, and withdrawal syndrome were also reported.
Statistical analysis
The null hypothesis was the absence of difference between both groups and the alternative hypothesis was a decrease of complications without drain. The normal distribution of the variables was assessed with a Kolmogorov–Smirnov test. Continuous variables were analyzed with a Student’s t-test and categorial binary variables with a Pearson’s chi-square test or a Fisher’s exact test. A p-value smaller than 0.05 was considered statistically significant.
Results
Demographics
From October 2007 to January 2017, 144 patients (80 males, 64 females) with a median age of 64 years were included according to the eligibility criteria (Fig. 1). Patient’s demographics are presented in Table 1. Both groups were comparable.
Endpoints
The rate of fluid collection at POD 30, which was defined as the primary endpoint, was high in both groups, but the difference between both groups (60.3% drain group vs. 62.0% no drain group, p = 0.844) was not statistically significant. The median drainage duration was 4 days. No difference was found when each subtype of complication was considered independently: seroma (46% drain group vs. 45.1% no drain group, p = 0.911), hematoma (11.1% drain group vs. 16.9% no drain group, p = 0.338) and abscess (4.8% drain group vs. 4.2% no drain group, p = 0.881). We recorded the size of all collections and performed analysis with different volume categories, without finding any difference between the groups. No difference in terms of collection was demonstrated based on hernia defect size. However, there was a statistically significant reduction in overall complications on POD 30 in the drain group (29% vs. 50.7%, p = 0.008), with a lower mean CCI (7.3% vs. 24%, p = 0.006) and a lower rate of surgical complications (21.7% vs. 42.7%, p = 0.007). Both groups were similar regarding medical complications as depicted in Table 2. Length of hospital stay and readmission rates were similar in both groups. The operative mean time was 151 and 135 min for the drain and no-drain group, respectively. Details of all complications are available in the supplementary material.
Follow up
The follow up was complete for all patients, with a clinical and radiological control at POD 30.
Discussion
This prospective randomized study assessed the role of intraoperatively placed drains to avoid postoperative fluid collection after open incisional hernia repair. Postoperative fluid collections were observed in both groups in up to 65% of patients, and drain placement could not decrease the incidence of that particular complication at POD 30. This rate of collection seems important; however, only a small amount was clinically relevant. Although the trial was negative on the primary endpoint, the secondary endpoints highlighted significant results in terms of morbidity. There were significantly fewer overall complications on POD 30 in the drain group and a lower rate of surgical complications. These findings will be discussed in more detail below.
There is no clear evidence in the current literature regarding the prophylactic use of drains. In a prospective study including 42 patients in 2015, Westphalen et al. reported a similar rate of seroma in patients with drains (52.4%) versus quilting sutures (42.9%) on POD 30. A retrospective study of Krpata et al. in 2017 analyzed complications after drainage in incisional hernia repair with a retromuscular mesh [24]. This large study (n = 581) with 82.8% of drainage use showed a preventing role for seroma development. However, their rates of seroma in the drainage group (1%) and the control group (8%) were largely inferior to our findings, most likely related to diagnostic methods and definitions used by the authors to detect seroma. This difference calls into question the clinical relevance of fluid collection, which may be clinically silent while radiologically detectable. Moreover, we have to bear in mind the methodological difference in drain placement. The difference observed between the findings of Krpata et al. and ours could be also explained by the number and different sites of drainage between our studies. For example, the retromuscular drainage is a less extensible space than the subcutaneous, and therefore less prone to large collections.
The high complication rate in our study (29% in the drainage group; 50.7% in the control group) is explained by a compulsory and institutionally-organized system of complication recording, including minor complications graded I and II according to Clavien-Dindo classification. The higher rate of surgical complications in the group without drainage might suggest that drainage could prevent complications other than fluid collection, and therefore positively influence postoperative outcomes. Although drainage was predictive of a lower CCI, it did not reflect on hospital stay or readmission rate. In addition, the severity of complications graded by Clavien-Dindo classification was similar in both groups.
We investigated which subtype of complication was most present in each group. The surgical site infection rate was comparable in both groups (5.9% vs. 9.3%, p = 0.439), remarkably close to literature [25], especially to reports from Krpata et al. (6–3%) and Westphalen et al. (19.1–23.8%). Although the absence of drainage seems to be a predictive factor for wound dehiscence according to our results (p = 0.041), these dehiscences only required local care and were not associated with more surgical site infection. These results may assume that drains may prevent local fluid retention, while the absence of drainage may favor the evacuation of remaining fluid through the wound, translating into wound dehiscence, ultimately delaying wound healing. Although a statistically significant difference is found for surgical complications (p = 0.007), in our opinion, no strong recommendation can be made with our results given that the subcategories show only slightly significant differences (p = 0.041).
The strength of the present study relies on its high-standard prospective, randomized design and also on the recording of objective and quantifiable endpoints. External validity is high since inclusion criteria did not select the type of initial surgery or patient comorbidities. The sample represents a standard population making it easily reproducible for further investigation. The 10-year recruitment period is a drawback since laparoscopic surgeries have become widely popular. These minimally-invasive procedures competed with our study and limited recruitment. After careful evaluation of this situation with our ethical committee, the study had to be terminated prematurely and the number of participants estimated by the initial power calculation has not been reached. In our opinion, the value of the present study remains strong, as these novel approaches are still not widely accepted or implemented, and open surgery remains the gold standard for the majority of surgeons. In addition, the 144 included patients represent a large population when compared to other series. Since this study was terminated prematurely due to the expansion of minimally invasive techniques, it would be interesting to repeat this research with other techniques, such as minimal invasive approaches or onlay mesh placement. Finally, according to our primary endpoint, the study was negative. However, a clinically relevant conclusion is in our view appropriate.
Conclusion
Prophylactic drainage in open incisional hernia repair does not objectively reduce the rate of postoperative fluid collections. Therefore, our results do not support the use of routine drainage in incisional hernia repair.
References
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Diener MK, Voss S, Jensen K et al (2010) Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg 251:843–856
Sanders DL, Kingsnorth AN (2012) The modern management of incisional hernias. BMJ 344:e2843
Kaafarani HMA, Hur K, Hirter A et al (2009) Seroma in ventral incisional herniorrhaphy: incidence, predictors and outcome. Am J Surg 198:639–644
Bickenbach KA, Karanicolas PJ, Ammori JB et al (2013) Up and down or side to side? A systematic review and meta-analysis examining the impact of incision on outcomes after abdominal surgery. Am J Surg 206:400–409
Heniford BT, Park A, Ramshaw BJ et al (2003) Laparoscopic repair of Ventral Hernias: Nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–400
Helgstrand F, Rosenberg J, Bay-Nielsen M et al (2010) Establishment and initial experiences from the Danish Ventral Hernia Database. Hernia 14:131–135
Burger JWA, Luijendijk RW, Hop WC et al (2004) Long-term Follow-up of a Randomized Controlled Trial of Suture Versus Mesh Repair of Incisional Hernia. Ann Surg 240:578–585
den Hartog D, Dur AHM, Tuinebreijer WE et al (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev 3:CD006438
Klink CD, Binnebösel M, Lucas AH et al (2010) Do drainage liquid characteristics serve as predictors for seroma formation after incisional hernia repair? Hernia 14:175–179
White TJ, Santos MC, Thompson JS (1998) Factors affecting wound complications in repair of ventral hernias. Am Surg 64:276–280
Coletta D, Del Basso C, Giuliani G et al (2019) Subcutaneous suction drains do not prevent surgical site infections in clean-contaminated abdominal surgery—results of a systematic review and meta-analysis. Langenbecks Arch Surg 404:663–668
Wysocki AP, McGowan B (2018) To drain or not to drain: Supreme Court has the answer. ANZ J Surg 88:115–115
Luo Y, Mohammed Jinnaah S, Masood D et al (2020) Drain tube use in incisional hernia repair: a national survey. Hernia 25(2):427–433
Luo Y, Masood D, Jinnaah S et al (2020) Do drain tubes help reduce risks of post-operative complications in complex incisional hernia repair (as defined by a recent court ruling)? ANZ J Surg 90:1080–1085
Massey LH, Pathak S, Bhargava A et al (2018) The use of adjuncts to reduce seroma in open incisional hernia repair: a systematic review. Hernia 22:273–283
Gurusamy KS, Allen VB (2013) Wound drains after incisional hernia repair. Cochrane Database Syst Rev 12:CD005570
Westphalen AP, Araújo ACF, Zacharias P et al (2015) Repair of large incisional hernias. To drain or not to drain. Randomized clinical trial. Acta Cir Bras 30:844–851
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Tastaldi L, Alkhatib H (2018) Incisional Hernia repair: open retromuscular approaches. Surg Clin North Am 98:511–535
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Slankamenac K, Graf R, Barkun J et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Horan TC, Andrus DG, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Krpata DM, Prabhu AS, Carbonell AM et al (2017) Drain placement does not increase infectious complications after retromuscular ventral hernia repair with synthetic mesh: an AHSQC analysis. J Gastrointest Surg 21:2083–2089
Sauerland S, Walgenbach M, Habermalz B et al (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 3:CD007781
Acknowledgements
The authors would like to thanks Dr Paroz A., Dr Vuilleumier H. and Dr Donadini A. for their respective contribution to the study, regarding the design, the implementation and patient’s recruitment. The authors declare that they have no conflict of interest. Abdominal wall ultrasound carried out systematically on post-operative day 30 were supported by the research fund of the Visceral Surgery Department of Lausanne University Hospital CHUV, Lausanne, Switzerland.
Funding
Open access funding provided by University of Lausanne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Abdominal wall ultrasounds carried out systematically on post-operative day 30 were supported by the research fund of the Visceral Surgery Department of Lausanne University Hospital CHUV, Lausanne, Switzerland. The study was approved by the local ethics committee (CER-VD 31/07, DP-2007-CHV-UNIL) and was registered as a prospective randomized clinical trial on clinicaltrials.gov (NCT00478348).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Willemin, M., Schaffer, C., Kefleyesus, A. et al. Drain Versus No Drain in Open Mesh Repair for Incisional Hernia, Results of a Prospective Randomized Controlled Trial. World J Surg 47, 461–468 (2023). https://doi.org/10.1007/s00268-022-06725-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06725-4