Abstract
Background
Acute appendicitis is a common surgical emergency with an estimated lifetime prevalence of 8.6% for males and 6.7% for females. Despite the frequency of presentation, considerable variation in clinical practice exists. Our study aimed to explore temporal trends in the investigation, treatment and outcomes for patients with appendicitis between 2002 and 2016.
Methods
Data collected included all patients aged ≥16 years across the NHS trusts in Northern England between 01/01/2002 and 31/12/2016 diagnosed with appendicitis. Patient demographics, co-morbidity and management strategies were included. Outcomes of interest were length of stay and inpatient mortality.
Results
Over a 15 years period, 22,137 patients were admitted with acute appendicitis. A consistent male preponderance (n = 11,952, 54%) was observed, and median age increased over time (2002–2006: 36.4 vs. 2012–2016: 39.5, p < 0.001). Comorbidity of patients also increased (p < 0.001) in recent years. Computed tomography (CT) use increased from 0.8 to 21.9% (p < 0.001) over the study period. Following CT scanning, there was a longer time to theatre (1.22 vs. 0.70 days, p < 0.001), and patients were more frequently managed non-operatively (23.8% vs. 5.7%, p < 0.001). The utilisation of laparoscopic approaches significantly increased from 4.1 to 70.4% (p < 0.001). Laparoscopic patients had a shorter median length of stay (2.97 days) when compared with open surgery (4.44 days) or non-operative (6.19 days) patients. The 30-day mortality rate was 0.33% overall and decreased with time (p = 0.004).
Conclusions
CT and laparoscopic surgery are increasingly utilised in the management of appendicitis. Along with other advances in clinical practice, they have led to reduced lengths of stay and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appendicitis is a common pathology worldwide that requires urgent treatment [1]. The UK incidence is approximately 81 cases per 100,000 person-years [2] and rose during the twentieth century. There is a lifetime prevalence of 8.6% for males and 6.7% for females [3]. Despite the lower prevalence, a higher rate of negative appendicectomy has been observed in females [4]. This is likely reflective of a greater difficulty in establishing a diagnosis where ovarian pathologies can present similarly to appendicitis [4, 5]. The overall negative appendicectomy rate in the UK of 20% is comparatively higher than other European countries (6%) [4].
The role of computed tomography (CT) in the diagnostic pathway for appendicitis has been debated. Potential benefits include improved diagnostic accuracy, identification of complicated pathology and of patients who may benefit from conservative treatment [6]. Disadvantages include requiring contrast to improve diagnostic accuracy, radiation exposure and increased cost, when compared to abdominal ultrasound [6]. The sensitivity and specificity of CT are estimated to be 95 and 94%, respectively, providing high yield diagnostic value, with even low-dose CT achieving equivalent accuracy [6]. Ultrasound (US) can be used in isolation or sequentially with CT as part of the diagnostic work up [6]. While US is free from ionising radiation exposure and useful for identifying gynaecological pathology, the appendix can be difficult to visualise and sensitivity and specificity for appendicitis are poor [7].
The World Society of Emergency Surgery (WSES) and European Association of Emergency Society (EAES) have proposed guidelines [8, 9] recommending routine risk scoring based on clinical assessment and biochemistry alongside imaging. These guidelines suggest the use of laparoscopic surgery in all cases of appendicitis, unless contraindicated [8, 9]. Laparoscopic appendicectomy carries significant advantages over open for reducing pain intensity on postoperative day one, wound infections, length of hospital stay and time to resume normal activities [10, 11]. The use of antibiotics to treat uncomplicated appendicitis has also been explored. Studies have not demonstrated a sound conclusion in efficacy of antibiotics compared to the standard appendicectomy [12, 13] but have highlighted the high risk of recurrence [14].
The aim of this study was to evaluate trends in clinical presentation, changes in the use of CT, management approach and outcomes for patients diagnosed with appendicitis across NHS hospitals in the North of England over a 15 years period.
Methods
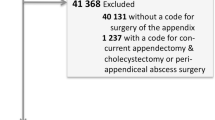
Data for hospital admissions are routinely collected by the Health and Social Care Information Centre to provide Hospital Episode Statistics (HES) [15]. Following Caldicott approval, data from acute NHS foundation trusts in the North of England were retrieved (“Appendix 1”). All emergency admissions under a general surgeon between 1 December 2001 and 30 November 2016 were requested. The data fields requested are listed in (“Appendix 2”). Patient data were irreversibly anonymised prior to being sent to the authors.
Data definitions and management
The cohort comprised of patients aged 16 years and older, admitted under a general surgeon as an emergency with a diagnosis of appendicitis. Postal codes were converted to Index of Multiple Deprivation (IMD) scores using the online postcode conversion tool [16] and then converted to deprivation quintiles [17]. Weekends were defined as Saturday and Sunday, including bank holidays, and weekdays defined as Monday to Friday. Data on co-morbidities were generated by mapping secondary ICD-10 diagnostic codes to the relevant co-morbidity before applying weightings employed by the hospital standardised mortality ratio [18, 19] to determine the Charlson score [17, 20].
The data provided was used to calculate age at admission, day of admission, season of admission, duration of hospital stay, time to procedure from admission, day of procedure and day of in-hospital death. Overall in-hospital death within 30 days was the mortality outcome of interest. The named responsible consultant for the relevant hospital spell was provided in the dataset, and consultant subspeciality was determined using information from NHS search and other subspecialist society websites [21,22,23]. Names were mapped to the appropriate subspeciality based on that which the consultant predominantly practiced during the year group of the study. Subspecialties were categorised as GI or other ‘general’ surgeons with the latter group consisting of breast, vascular and other non-gastrointestinal subspeciality ‘general’ surgeons working on emergency on-call rotas during the study period.
Statistical analysis
Categorical data were summarised using frequencies and percentages, and continuous data using the mean and 95% confidence interval. Differences in case mixes between these groups were investigated using Pearson's χ2 test for categorical variables trends. Continuous data were assessed using the mean and 95% confidence intervals with differences between these variables determined by either students t-test or ANOVA with post-hoc testing. Comparisons of non-parametric data between two groups were performed using a Mann–Whitney U test or Kruskal–Wallis test when comparing more than 2 groups. Data were stored and processed in Excel® 2010, and analyses were undertaken using IBM SPSS Statistics v27.0 (SPSS, Chicago, Illinois, USA) and STATA 16.1 (StataCorp, College Station, Texas, USA) software. Statistical significance was defined in all cases as P < 0.050.
Results
Changes in patient characteristics over time
Over the 15 years study period, 22,137 patients were admitted with appendicitis to NHS hospitals in the North of England (Table 1). These accounted for 4.5% of acute surgical admissions. The number of presentations increased from 6844 (2002–2006) to 7507 (2012–2016, p < 0.001). Whilst most patients were young (“Appendix 3”), the average age of presentation rose significantly (p < 0.001). Patients were increasingly co-morbid, demonstrated by higher Charlson scores (p < 0.001). A greater proportion were admitted via A&E latterly (39.9–60.2%, p < 0.001) corresponding with a reduction in direct GP admissions (50.4–27.5%). An increased proportion of patients presented to smaller trusts (p < 0.001). An increasing trend of admission under gastrointestinal surgeons was observed while admissions under other general surgery subspecialists reduced (p < 0.001). No significant trend in admissions was evident between seasons or day of the week.
Changes in patient investigation and management
Usage of CT significantly increased over time (from 0.8 to 21.9%, p < 0.001, Table 1). There was a rise in proportion of older patients investigated with CT (Fig. 1). It was also noted that patients from areas of greater deprivation were slightly less likely to undergo a CT scan (p < 0.001). Patients who underwent a CT were significantly more likely to be managed non-operatively (23.8% vs. 5.7%) or undergo a right hemicolectomy (3.3% vs. 0.8%, Table 2) and spent longer in hospital (“Appendix 4”). Time to operation, amongst those who did not undergo a CT scan, remained consistently low (Table 2).
There was a significant reduction in open operating and a rise in laparoscopic procedures (Fig. 2, Table 1). The proportion of laparoscopic converted to open procedures decreased from 14.0 (2002–06) to 5.8% (2012–16) (p < 0.001). The number of patients treated non-operatively increased from 5.7 to 10.2%; they were significantly older and more co-morbid. Those who underwent a right hemicolectomy were the oldest and most co-morbid (“Appendix 5”). Patients who successfully underwent laparoscopic appendicectomy were younger, with fewer co-morbidities, admitted via A&E and under the care of a GI specialist.
Changes in patient outcomes over time
The median length of stay in hospital significantly reduced by approximately one day (Table 3). This is reflected by the decreased length of stay in patients treated non-operatively and laparoscopically, with a slight increase in patients who were converted to open surgery from laparoscopic
Thirty-day mortality, though low throughout, significantly decreased over time (p = 0.004). Improved post-operative mortality was particularly evident amongst those treated non-operatively (2002–2006; 3.1% vs. 2012–2016; 1.1%, p = 0.009).
Appendicitis in older patients
Older patients were more likely to have significant co-morbidities, undergo CT and receive non-operative management (all p < 0.001, Table 4). Their commonest route of admission was via A&E (49.3%, p = 0.027). Older patients were also more likely to require a right hemicolectomy (50–59; 1.4% vs. ≥80; 4.6%, p < 0.001).
Older patients waited longer for their operation, had a longer length of stay in hospital and a higher mortality rate after 30 days (Table 5). The time to operation almost doubled from 0.78 (50–59 years) to 1.5 (≥80 years) days (p < 0.001) with advancing age. The oldest patients had the longest stay in hospital, averaging 12.35 days (≥80 years) compared to 4.59 days (50–59 years) (< 0.001). Those aged ≥80 also had the poorest outcomes with an 8.3% 30-day mortality rate, compared to 0.1% in younger patients (p < 0.001).
Discussion
This study reports 22,137 cases of appendicitis across the 15 years study period in the North of England. We note significant changes in patient demographics, CT usage and operative approach.
Appendicitis is regarded as a disease of the young, and this is concordant with our findings of peak incidences between ages 16–29 (“Appendix 3”). We note an increase in the age of presentation (Table 1), similar to other studies [24, 25]. This is likely because of the increasing life expectancy over the study period [26], and with the increased usage of CT, the higher diagnosis rate of appendicitis.
A higher proportion of patients were male, which is concordant with other studies [4, 13, 14]. Males drove the increased incidence in the younger population (“Appendix 6”). The RIFT study demonstrated that two thirds of patients referred to a general surgeon with undifferentiated right iliac fossa (RIF) pain were female, yet less than 20% had a confirmed diagnosis of appendicitis [4]. It is known that gynaecological conditions in younger patients often present similarly to appendicitis and frequently lead to mislabelled differential diagnoses. Incidence of appendicitis in females is however increasing, and the rise in use of CT (Table 1) may be contributing towards improved diagnostic rates. Above 40 years, this discrepancy subsides leading to a similar, if not reversed trend thereafter. Gynaecological differential diagnoses have a lower prevalence in this age group making appendicitis a more viable diagnosis [27, 28].
We noted a significant increase in co-morbidity of patients over time (Table 1), likely associated with the rising trend of age. The increase in admission under a GI subspecialist reflects the changes in surgical training and a move towards more GI sub-specialists working a greater proportion of emergency cover [29].
Proposed international guidelines [8, 9] set out a diagnostic pathway for appendicitis. Patients can be categorised into low, intermediate, or high risk based on clinical biochemistry and risk scores using the Alvarado Score (AS) [30], Appendicitis Inflammatory Response Score (AIRS) [31] or Adult Appendicitis Score (AAS) [32]. Recommendations are to use AAS in women and AIRS in men [4]. Alone, these scores provide limited information, so imaging is recommended in higher risk patients to clarify diagnostic uncertainty [8, 9].
CT is widely used due to greater availability, reduced cost and high sensitivity and specificity [6]. All hospitals in the North of England gained access to out-of-hours radiology services during the study period, where CT reporting may have aided diagnosis and informed decision making. It could be suggested that CT can identify patients with uncomplicated appendicitis who may benefit from non-operative management [6, 8]. Our results suggest that the rise in CT usage was predominantly driven by older patients (Fig. 1). Guidelines recommend CT to rule out alternative diagnoses such as malignancy which can mask the presentation of appendicitis [33].
CT has a high specificity but low sensitivity for differentiating complicated from uncomplicated appendicitis lowering accuracy for identifying patients who can be medically managed [34]. Guidelines suggest surgical management should be pursued in all cases unless contraindicated [6, 8, 9]. We propose that CT is useful for guiding surgical management rather than identifying patients with uncomplicated disease who could be managed non-operatively, as previously suggested [6].
The increase in laparoscopy and reduction in open surgery is concordant with the current gold standard treatment [6, 8, 9]. We identified increasing success in laparoscopic approach, with a significant reduction in laparoscopic converted to open appendicectomies (14.0–5.8%, p < 0.001). One meta-analysis found similar results; conversion rates between 20–45% before 2000 and 0–18% over the last decade [35]. The success of laparoscopy can be attributed in part to the increase in GI subspecialists treating patients who have likely found confidence with laparoscopy from their elective practice.
Non-operative management of appendicitis became increasingly relevant in the current SARS-Cov-2 pandemic. The proportion of patients managed non-operatively rose to 64% during the peak of the pandemic [36]. COVID-19 causes an inflammatory viral-induced cytokine storm increasing surgical mortality risk [37]. Despite little evidence supporting viral transmission through aerosolised procedures, studies recommend modifications to standard practice to minimise risk of transmission [38]. Benefits of antibiotic therapy as an alternative to surgery have been explored [36, 39]. Recent literature found that although antibiotics had a lower infection rate, their rate of reoperation and disease recurrence was higher than surgical intervention [14, 40]. Poorer quality of life has been discovered with antibiotics alone; no difference has been identified in hospital length of stay [41]. Consequently, laparoscopic surgery remains the gold standard treatment [6, 8, 9] as supported by our results (Table 3).
The rise in patients managed non-operatively may be due to the changing demographics of the cohort over time. Our results demonstrated that patients receiving non-operative management were amongst the oldest and most comorbid (“Appendix 5”), and these factors will commonly lead to an increased risk from surgical intervention. One meta-analysis described a reduced complication rate (OR 0.21–0.51) with conservative management compared to any operative approach in elderly patients, emphasising the potential age-related risk of surgical intervention [40]. Public preference for antibiotic treatment to avoid an operation is also notable from contemporary literature [42] and a shift from paternalistic medicine, towards patient-centred care may also be contributing to the rising non-operative treatment.
The improved length of stay is likely driven by the rising popularity of laparoscopy and reduction in overall mortality [8]. Poorest outcomes were among those managed with a right hemicolectomy or non-operatively however, these patients were more elderly and comorbid (“Appendix 5”). Length of stay and overall mortality improved across the study period in both age groups.
Appendicitis is complicated in the elderly. Differential diagnoses of RIF pain increase with age as often presentation can be vague. Previous literature indicates that CT is preferred to investigate as it improves diagnostic accuracy and reduces negative appendicectomy rates [43]. When surgery is chosen, it incurs longer operation waiting times and length of stay in hospital, which may reflect reluctance to operate or diagnostic challenges [43], reinforced by our findings.
The hospital episode statistics data utilised, relies on accurate clinical coding, which depends on good documentation. In large datasets like this, small individual inaccuracies in coding are likely to be insignificant and unlikely to bias overall results. These data don’t allow accurate analysis of negative appendicectomy rates as histological data was unavailable, nor were details of complications, readmissions, or antibiotic use in this population. Data on clinical biochemistry and calculated risk scores for individual patients would have allowed risk stratification using AAS, AIRS and AS but unfortunately this was not able to be performed for this study. Details of a broader population with undifferentiated RIF pain would have allowed us to comment on the proportions of patients who went on to be diagnosed with appendicitis. Admissions are coded by the consultant responsible for care, rather than the operative consultant. The majority of appendicectomies in public hospitals are performed by non-consultant grade surgeons [44], thus the two may differ limiting conclusions drawn on operative influence.
Our results highlight improvements made in managing appendicitis over time. These results are highly suggestive that improved outcomes are due to laparoscopic operating and CT usage, emphasising the importance of laparoscopic appendicectomy as the gold standard treatment for appendicitis [6, 8, 9].
References
Bhangu A, Søreide K, Di Saverio S et al (2015) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 386(10000):1278–1287
Ferris M, Quan S, Kaplan BS et al (2017) The global incidence of appendicitis. Ann Surg 266(2):237–241
Addiss DG, Shaffer N, Fowler BS et al (1990) The epidemiology of appendicitis and appendectomy in the Unites States. Am J Epidemiol 132(5):910–925
Bhangu A, Nepogodiev D, Matthews JH et al (2019) Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg 107(1):73–86
Nepogodiev D, (2018) Right Iliac Fossa Pain Treatment (RIFT) study: protocol for an international, multicentre, prospective observational study. BMJ open 8(1). https://pubmed.ncbi.nlm.nih.gov/29331965/
Rud B, Vejborg TS, Rappeport ED, et al. (2019) Computed tomography for diagnosis of acute appendicitis in adults. Cochrane database Syst Rev 2019(11). https://pubmed.ncbi.nlm.nih.gov/31743429/
Souza ND, Souza CD, Grant D et al (2015) The value of ultrasonography in the diagnosis of appendicitis. Int J Surg 13:165–169
Di Saverio S, Podda M, De Simone B et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15(1):1–42. https://doi.org/10.1186/s13017-020-00306-3
Gorter RR, Eker HH, Gorter-Stam MAW et al (2016) Diagnosis and management of acute appendicitis eaes consensus development conference 2015. Surg Endosc 30(11):4668–90
Wang D, Dong T, Shao Y et al (2019) Laparoscopy versus open appendectomy for elderly patients, a meta-analysis and systematic review. BMC Surg 19(1):1–11
Ukai T, Shikata S, Takeda H et al (2016) Evidence of surgical outcomes fluctuates over time: results from a cumulative meta-analysis of laparoscopic versus open appendectomy for acute appendicitis. BMC Gastroenterol. https://doi.org/10.1186/s12876-016-0453-0
Vons C, Barry C, Maitre S et al (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377(9777):1573–1579
Salminen P, Paajanen H, Rautio T et al (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA - J Am Med Assoc 313(23):2340–2348
Podda M, Gerardi C, Cillara N et al (2019) Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg 270(6):1028–1040
Health and Social Care Information Centre, Hospital Episode Statistics (2015)
Education D of. Education and Skills (2015) In: Your Area: IDACI Score and Rank of IDACI. UK Government
Clinical Indicators Team (2014) Analysis of the impact of deprivation on the summary hospital-level mortality indicator (SHMI). Heal. Soc. Care Inf. Cent., p 6
Quan H, Li B, Couris CM et al (2011) Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173(6):676–682
Clinical Indicators Team, Summary Hospital-level Mortality Indicator. (2018). https://files.digital.nhs.uk/3F/80BAA0/SHMIspecification.pdf
Charlson M, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
NHS, Find Hospital Consultants (2021) https://www.nhs.uk/Service-Search/Hospital/LocationSearch/8/Consultants. Accessed 12 Aug 2021
AUGIS, Find an AUGIS specialist (2021) http://www.augis.org/find-a-specialist/. Accessed 12 Aug 2021
ACPGBI, Find a surgeon (2018) https://www.acpgbi.org.uk/patients/surgeon_directory/. Accessed 12 Aug 2021
Buckius MT, McGrath B, Monk J et al (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175(2):185–190
Ceresoli M, Zucchi A, Allievi N et al (2016) Acute appendicitis: epidemiology, treatment and outcomes- analysis of 16544 consecutive cases. World J Gastrointest Surg 8(10):693–699
Leon DA, Jdanov DA, Shkolnikov VM (2019) Trends in life expectancy and age-specific mortality in England and Wales, 1970–2016, in comparison with a set of 22 high-income countries: an analysis of vital statistics data. Lancet Public Health 4(11):575–582
Unemo M, Bradshaw CS, Hocking JS et al (2017) Sexually transmitted infections: challenges ahead. Lancet Infect Dis 17(8):235–279
Robertson JJ, Long B, Koyfman A (2017) Myths in the evaluation and management of ovarian torsion. J Emerg Med 52(4):449–456
Harries RL, Rashid M, Smitham P et al (2016) What shape do UK trainees want their training to be? Results of a cross-sectional study. BMJ Open 6(10):1–11
Alvarado A (1986) A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 15(5):557–564
Andersson M, Andersson RE (2008) The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the alvarado score. World J Surg 32(8):1843–1849
Sammalkorpi HE, Mentula P, Savolainen H et al (2017) The introduction of adult appendicitis score reduced negative appendectomy rate. Scand J Surg 106(3):196–201
Siddharthan RV, Byrne RM, Dewey E et al (2019) Appendiceal cancer masked as inflammatory appendicitis in the elderly, not an uncommon presentation (Surveillance Epidemiology and End Results (SEER)-Medicare Analysis). J Surg Oncol 120(4):736–739
Kim HY, Park JH, Lee YJ et al (2018) CT in differentiating complicated from uncomplicated appendicitis: presence of any of 10 ct features versus radiologists’ gestalt assessment. Am J Roentgenol 287(1):218–227
Athanasiou C, Lockwood S, Markides GA (2017) Systematic review and meta-analysis of laparoscopic versus open appendicectomy in adults with complicated appendicitis: an update of the literature. World J Surg 41(12):3083–3099. https://doi.org/10.1007/s00268-017-4123-3
Javanmard-Emamghissi H, Boyd-Carson H et al (2020) The management of adult appendicitis during the COVID-19 pandemic: an interim analysis of a UK cohort study. Tech Coloproctol 25(4):401–411
Lei S, Jiang F, Su W et al (2020) Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 21:100331. https://doi.org/10.1016/j.eclinm.2020.100331
Vigneswaran Y, Prachand VN, Posner MC et al (2020) What is the appropriate use of laparoscopy over open procedures in the current covid-19 climate? J Gastrointest Surg 24(7):1686–1691
Collard M, Lakkis Z, Loriau J et al (2020) Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: changes in treatment modalities related to the COVID-19 health crisis. J Visc Surg 157(3):33–42
Yang Z, Sun F, Ai S et al (2019) Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg 19(1):1–10
O’Leary DP, Walsh SM, Bolger J et al (2021) A randomised clinical trial evaluating the efficacy and quality of life of antibiotic only treatment of acute uncomplicated appendicitis. Ann Surg 24(2):240–247
Bom WJ, Scheijmans JCG, Gans SL, et al. (2021). Population preference for treatment of uncomplicated appendicitis. BJS open. 5(4). https://academic.oup.com/bjsopen/article/5/4/zrab058/6342604
Calis H (2018) Morbidity and mortality in appendicitis in the elderly. J Coll Physicians Surg Pakistan 28(11):875–8
Mackrill D, Allison S (2015) Laparoscopic appendicectomy: an operation for all trainees but does the learning curve continue into consultanthood? ANZ J Surg 85(5):349–352
Calderdale and Kirklees 999 Call for the NHS (2019) Massive North Cumbria and North East Integrated Care System to go live in the Spring. https://calderdaleandkirklees999callforthenhs.wordpress.com/2019/02/02/massive-north-cumbria-and-north-east-integrated-care-system-to-go-live-in-the-spring/
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authorship group declare that they have no conflicts of interest and received no funding for this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: A map of the Northeast of England and its relevant trusts

Source: Calderdale and Kirklees 999 Call for the NHS, 2019 [45].
Appendix 2: Data fields requested from the National Health Service Foundation Trusts’ Caldicott Guardian
Demographic fields | Age, sex, postcode |
|---|---|
Co-morbidity fields | ICD-10 diagnosis 2 onwards |
Diagnosis/operation fields | Primary diagnosis (ICD-10 diagnosis 1), operation date, operation type (OPCS codes for operation 1 onwards), consultant name |
Outcome fields | Admission date and source, discharge date and location, mortality (time to death) |
Appendix 3: Comparison of proportion of patients admitted with appendicitis, by age and study period

Appendix 4: Outcomes for patients presenting with appendicitis by CT utilisation
CT performed (n = 2491) | CT Not performed (n = 19,646) | Overall (n = 22,137) | p value | |
|---|---|---|---|---|
Length of stay*‡ | 5 (3,8) | 3 (2,4) | 3 (2,5) | < 0.001 |
Non-operative | 5 (3,7) | 3 (2,6) | 4 (2,7) | < 0.001 |
Appendicectomy | 5 (3,8) | 3 (2,4) | 3 (2,4) | < 0.001 |
Laparoscopic | 4 (2,6) | 2 (2,3) | 2 (2,3) | < 0.001 |
Laparoscopic to open | 7 (5,10) | 4 (3,6) | 5 (3,7) | < 0.001 |
Open | 6 (4,10) | 3 (2,4) | 3 (2,5) | < 0.001 |
Right Hemicolectomy | 10 (8,14) | 9 (6,14) | 9 (7,14) | 0.144 |
30-day mortality | 17 (0.7) | 57 (0.3) | 74 (0.3) | 0.001 |
Non-operative | 9 (1.5) | 16 (1.4) | 25 (1.5) | 0.877 |
Appendicectomy | 7 (0.4) | 35 (0.2) | 42 (0.2) | 0.082 |
Laparoscopic | 2 (0.2) | 3 (0.0) | 5 (0.1) | 0.038 |
Laparoscopic to open | 1 (0.5) | 2 (0.3) | 3 (0.4) | 0.691 |
Open | 4 (0.7) | 30 (0.3) | 34 (0.3) | 0.149 |
Right Hemicolectomy | 1 (1.2) | 6 (3.9) | 7 (2.9) | 0.246 |
Appendix 5: Characteristics of patients presenting with appendicitis, by management approach
Management approach | |||||||
|---|---|---|---|---|---|---|---|
Non-Operative (n = 1717) | Appendicectomy (n = 20,182) | Right Hemicolectomy (n = 238) | Overall (n = 22,137) | p-value | |||
Open (n = 10,155) | Laparoscopic to Open (n = 868) | Laparoscopic (n = 9158) | |||||
Age*‡ | 48 (3166) | 33 (2248) | 43 (2756) | 31 (2246) | 56.5 (4069) | 34 (2249) | < 0.001 |
Sex | 0.349 | ||||||
Female | 804 (46.8) | 4202 (41.4) | 416 (47.9) | 4643 (50.7) | 119 (50.0) | 10,184 (46.0) | |
Male | 913 (53.2) | 5953 (58.6) | 452 (52.1) | 4515 (49.3) | 119 (50.0) | 11,952 (54.0) | |
Charlson Category Score | < 0.001 | ||||||
0–1 | 1574 (91.7) | 9944 (97.9) | 832 (95.9) | 8992 (98.2) | 185 (77.7) | 21,527 (97.2) | |
2–4 | 125 (7.3) | 197 (1.9) | 34 (3.9) | 159 (1.7) | 38 (16.0) | 553 (2.5) | |
≥5 | 18 (1.0) | 15 (0.2) | 2 (0.2) | 7 (0.1) | 15 (6.3) | 57 (0.3) | |
Season | 0.613 | ||||||
Spring | 470 (27.4) | 2624 (25.8) | 216 (24.9) | 2395 (26.2) | 55 (23.1) | 5760 (26.0) | |
Summer | 464 (27.0) | 2599 (25.6) | 257 (29.6) | 2456 (26.8) | 62 (26.1) | 5838 (26.4) | |
Autumn | 405 (23.6) | 2388 (23.5) | 200 (23.0) | 2363 (25.8) | 61 (25.6) | 5417 (24.5) | |
Winter | 378 (22.0) | 2545 (25.1) | 195 (22.5) | 1944 (21.2) | 60 (25.2) | 5122 (23.1) | |
Deprivation Quintile | 0.275 | ||||||
1 (most) | 328 (22.3) | 2321 (26.1) | 188 (24.3) | 2004 (24.3) | 46 (23.0) | 4887 (25.0) | |
2 | 351 (24.0) | 1993 (22.5) | 172 (22.3) | 1828 (22.2) | 42 (21.0) | 4386 (22.4) | |
3 | 264 (18.0) | 1514 (17.1) | 141 (18.3) | 1479 (18.0) | 31 (15.5) | 3429 (17.6) | |
4 | 196 (13.4) | 1215 (13.7) | 105 (13.6) | 1109 (13.5) | 29 (14.5) | 2654 (13.6) | |
5 (least) | 326 (22.3) | 1834 (20.6) | 166 (21.5) | 1812 (22.0) | 52 (26.0) | 4190 (21.4) | |
Admission route | < 0.001 | ||||||
A&E | 800 (47.5) | 4439 (43.9) | 478 (55.4) | 5467 (61.8) | 98 (41.5) | 11,282 (51.9) | |
GP | 621 (36.8) | 4658 (46.1) | 331 (38.4) | 2594 (29.3) | 99 (41.9) | 8303 (38.2) | |
Consultant Clinic | 37 (2.2) | 22 (0.2) | 2 (0.2) | 104 (1.2) | 5 (2.1) | 170 (0.8) | |
Other | 228 (13.5) | 987 (9.8) | 52 (6.0) | 685 (7.7) | 34 (14.5) | 1986 (9.1) | |
Consultant subspeciality | 0.064 | ||||||
General Surgeon | 786 (45.8) | 5919 (58.3) | 431 (49.7) | 3168 (34.6) | 128 (53.8) | 10,432 (47.1) | |
GI Sub-specialist | 931 (54.2) | 4237 (41.7) | 437 (50.3) | 5990 (65.4) | 110 (46.2) | 11,705 (52.9) | |
Trust Size | < 0.001 | ||||||
Small/Medium | 998 (58.1) | 4979 (49.0) | 435 (50.1) | 4890 (53.4) | 128 (53.8) | 11,430 (51.6) | |
Large/Very Large | 719 (41.9) | 5177 (51.0) | 433 (49.9) | 4268 (46.6) | 110 (46.2) | 10,707 (48.4) | |
Day of week of admission | < 0.001 | ||||||
Weekday | 1356 (79.0) | 7616 (75.0) | 626 (72.1) | 6891 (75.2) | 202 (84.9) | 16,691 (75.4) | |
Weekend or Bank Holiday | 361 (21.0) | 2540 (25.0) | 242 (27.9) | 2267 (24.8) | 36 (15.1) | 5446 (24.6) | |
Day of week of operation | 0.044 | ||||||
Weekday | 116 (82.3) | 6907 (73.5) | 537 (72.0) | 6392 (73.6) | 168 (76.0) | 14,120 (73.6) | |
Weekend of Bank Holiday | 25 (17.7) | 2486 (26.5) | 209 (28.0) | 2298 (26.4) | 53 (24.0) | 5071 (26.4) | |
Computed Tomography scan performed | < 0.001 | ||||||
No | 1124 (65.5) | 9554 (94.1) | 663 (76.4) | 8,150 (89.0) | 155 (65.1) | 19,646 (88.7) | |
Yes | 593 (34.5) | 602 (5.9) | 205 (23.6) | 1008 (11.0) | 83 (34.9) | 2491 (11.3) | |
Appendix 6: Comparison of proportion of patients admitted with appendicitis, by sex and across the study period

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhaskar, J., McLean, R.C., Bhaskar, K. et al. Temporal Trends in the Investigation, Management and Outcomes of Acute Appendicitis over 15 Years in the North of England: A Retrospective Cohort Study. World J Surg 46, 2141–2154 (2022). https://doi.org/10.1007/s00268-022-06586-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06586-x